Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Acta Obstétrica e Ginecológica Portuguesa
versão impressa ISSN 1646-5830
Acta Obstet Ginecol Port vol.12 no.2 Coimbra jun. 2018
ORIGINAL STUDY/ESTUDO ORIGINAL
Razões para a interrupção da contraceção hormonal numa região de Portugal
Reasons for interrupting hormonal contraception in a region of Portugal
José Eduardo Mendes*, Cristina Serra*, Henrique Correia*, Ana Vaz Ferreira*, Carolina Gil**
USF Mondego
*Médico Interno de MGF
**Médica de Família
Endereço para correspondência | Dirección para correspondencia | Correspondence
ABSTRACT
Overview and Aims: Due to the scarcity of available information in Portugal in relation to the number of women who use and discontinue hormonal contraceptives, the aim of this study was to evaluate the factors associated with this behaviour.
Study Design: The study population was drawn from seven primary health care units and consisted of 329 women between the ages of 18 to 45, who were users of those units. We estimated the overall proportion of past and current use of hormonal contraceptives. We then calculated the discontinuation rates and analysed the reasons for stopping and switching contraceptive methods.
Population: Women between 18 and 45 years.
Methods: Study participants anonymously completed a self-report questionnaire. The questionnaire included information on: age, marital status, educational level, and obstetric history (number of pregnancies, abortions [spontaneous and induced], number of live childbirths). All hormonal contraceptive methods available in Portugal at the time were shown, with generic and trade names.
Results and Conclusions: Overall, 58.4% reported discontinuing at least one contraceptive method. The main reasons for the discontinuation were an adverse drug reaction (25.3%) and contraindication or medical advice (23.6%). The majority (71%) of adverse drug reactions began within the first year of usage and the main ones were headache (31.7%) and oligomenorrhea or amenorrhea (28.3%). Knowing the exact reasons why women abandon a contraceptive method is of the highest importance in improving contraceptive compliance. Medical doctors rely on this information to design counselling strategies and to provide the methods most widely used and accepted by women.
Keywords: Hormonal contraception; Contraceptive discontinuation; Population based survey; Primary Health Care
Introduction
Hormonal contraceptives are a safe and effective method of protection1. In Portugal, the proportion of contraceptive use reaches 85.1% in women aged between 15 and 55 years, with combined oral contraceptives representing 58.1-65.6% of contraceptive methods used2-4. Almost all contraceptive methods are available free of charge through public Family Planning services3. Oral contraceptives are in general characterized by high discontinuation rates mainly attributed to poor adherence5,6. It has been estimated that women between 15 and 45 years of age will discontinue contraceptive use up to 10 times7. The efficacy of combined oral contraceptives is highly dependent on good adherence to the prescribed regimen, which only occurs in about half of women8. The incorrect use or discontinuation of oral contraceptives are significant contributors to unintended pregnancy, which is an important public health concern8-10. In Portugal the only available data indicates that the prevalence of unintended pregnancy is about 39%11. Despite the widespread use of hormonal contraceptives, there is no consensus on the reasons that lead to discontinuation or change of method. Side effects have been argued to be the most common reason why women discontinue contraceptive methods12. However other factors have also been associated with poor adherence to hormonal contraceptives, including sociodemographic variables such as low educational and socioeconomic level8. Efficacy and side effects are the primary concerns of women when choosing a contraceptive method3.
Since there are no published studies on the subject in Portugal, the aim of this study was to evaluate the factors associated with change or discontinuation of hormonal contraceptives. The results should provide clinicians with a better understanding of the appropriate advice and necessary recommendations to help women choose the most suitable method, promoting proper adherence.
Methods
Study design
The participants in this study were women between 18 and 45 years old, from 11 medical files of seven primary health care units from the Grouped Health Centers of Baixo Mondego (central Portugal). The eligible population from the total clinical files was 4082. The required representative sample was calculated by simple random sampling to be 352 women. The questionnaires were distributed by convenience sample, stratified by health unit, between May 2015 and February 2016. Women attending those health units were invited in person by a medical doctor, regardless of the type of consultation. Women who had any condition that prevented the completion of the questionnaire by themselves (such as illiteracy) were excluded. Written informed consent was obtained from all participants. The study was approved by the Ethics Committee of Central Portugal's Regional Health Administration.
Questionnaire
Study participants anonymously completed a self-report questionnaire (Attachment 1 - original Portuguese version). The questionnaire included information on: age, marital status, educational level, and obstetric history (number of pregnancies, abortions [spontaneous and induced], number of live childbirths). All hormonal contraceptive methods available in Portugal at the time were shown, with generic and trade names. In addition, it was also questioned about the frequency of use of reproductive health services and degree of information about the current contraceptive method. Women who reported having used hormonal contraception were asked about the specific reason for discontinuation of the last method used. A list of reasons was incorporated, including an option to add their own reason, and another list of possible side-effects was also incorporated, again including an option to add a side-effect.
Analysis
A questionnaire was defined as valid if the questions regarding the main information for our study was completed. Specifically, a questionnaire was considered valid if it was possible to learn which contraceptive method was used before and which is currently used and the specific reason for stopping/switching methods. A questionnaire was considered invalid if there was conflicting information. Results are given as a percentage of those who responded for each question. The characteristics of the women were described using a frequency table for categorical variables. Contingency tables of categorical variables were analyzed using the chi-squared test or Fisher exact test. Continuous variables were analyzed using a t test or an analysis of variance, for normally distributed data; non-normally distributed variables were analyzed using a nonparametric method (Mann-Whitney or Kruskal-Wallis) for independent samples. Statistical significance was set at a 2-sided p-value of < .05.
Results
Study population
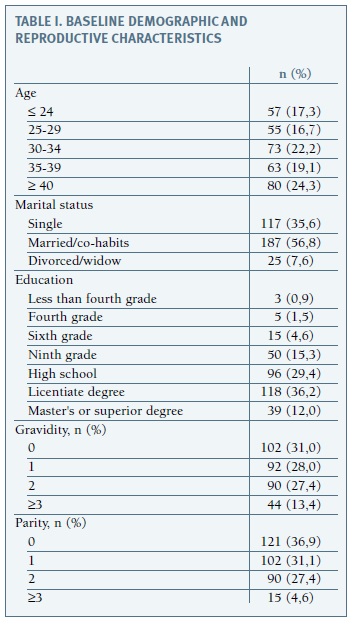
A total of 360 women were recruited to the study, of whom 329 (91.4%) completed a valid questionnaire. The demographic characteristics of the sample population are showed in Table I. Briefly, the mean age was 32.89 (range: 18-45 years). Most of them (56.8%) were married or cohabiting. The majority of women (77.6%) had at least secondary or high school education, with almost half of them (48.2%) having an university education. Most of them (68.8%) have been pregnant at least once and 63.8% have at least a child. Regarding regular follow-up (conventionally defined as an annual consultation with the family doctor or a gynaecologist), 280 women (86.2%) said they comply. Regarding information on the hormonal method they currently use, 219 women (94.4%) considered themselves well informed.
Lifetime contraceptive use
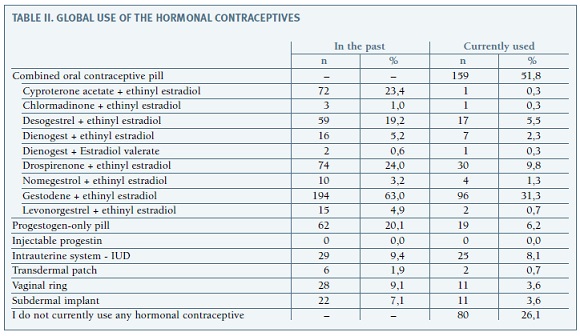
Among the 329 women who participated in the study, almost all of them (95.7%, 315) reported to currently use or to have used a hormonal contraceptive method. Starting age ranged from 10 to 44 years, with an average of 18.79 years (SD 4.155). About half of them (51.4%) started between the ages of 17 and 20 years. In women of whom it was possible to analyse all types of contraceptives used, the most popular one was any type of combined hormonal contraceptive, which was being used now or in the past by 95.7% of the respondents. Furthermore, all women who have used a hormonal contraceptive method have tried an oral combined contraceptive method. Overall, 192 women (58.4%) reported discontinuing at least one contraceptive method. The total number of hormonal methods of different classes was as follows: 128 women (41.6%) used only one method, 104 women (33.8%) used two methods, 55 women (17.9%) used three methods and only 21 women (6.8%) used four or more different methods. Of the 277 women currently using a hormonal contraceptive, 219 answered regarding duration. Use of this method ranged from 0 months to 25 years, with a mean of 73.1 months (SD 75.83), with 91.3% of women using the current method for 16 years or less and 77.6% for 10 years or less. The used contraceptives divided by class are detailed in Table II.
Reasons for discontinuation
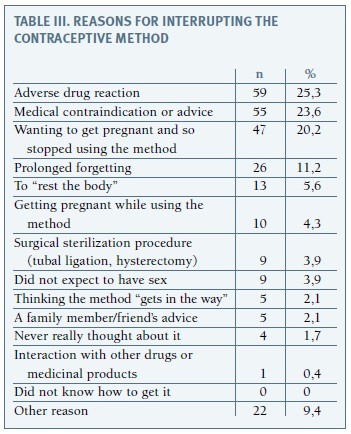
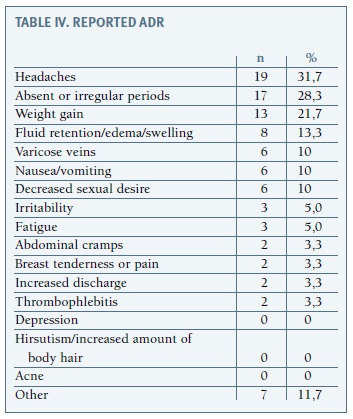
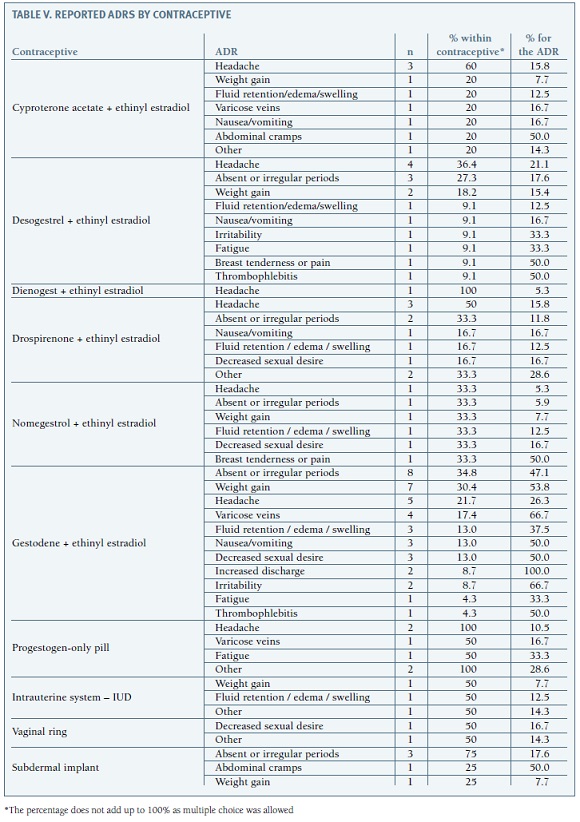
Main reasons for the discontinuation of a method were an adverse drug reaction (ADR) (25.3%), contraindication or medical advice (23.6%) and intention to become pregnant (20.2%), as shown on Table III. Of the 59 women who reported a possible ADR, only 39 responded as to its onset. ADRs were noticed on average 21 months after start using the contraceptive, varying from the first month of use to 12 years after. Nevertheless, 29% of women reported ADR in the first month and 71% in the first year. Only 5 women (16.1%) reported starting the reaction after 3 years of use. More than half of the women reported a single ADR (61%). As shown in Table IV, the most reported ADR was headache (31.7%), followed by oligomenorrhea or amenorrhea (28.3%). Headache was only reported by women who used oral contraceptives, and was more frequent for progestogen-only pills (headache was mentioned by all women who discontinued this method due to an ADR) and cyproterone acetate/ /ethinyl estradiol (60%), as detailed in Table V. Menstrual irregularities were more frequently reported by women who used subdermal implant (75% of the women who reported an ADR with this contraceptive), and also for gestodene/ethinyl estradiol (34.8%) and nomegestrol/ethinyl estradiol (33.3%).
Global use of contraceptive methods
The number of times a woman was pregnant was associated with a greater number of methods, and there was a positive and statistically significant association (rs = 0.277, p <0.001). The same is true for the number of children (rs=0.300; p<0.001). Adjusting for age, there are statistically significant differences regarding marital status, with single women presenting, in average terms, a smaller number of methods used when compared to the divorced or widowed (1.61 SD 0.774 and 2.17 SD 0.984, respectively). This difference in the number of methods is not significant when comparing single women with married women (2.08 SD 1.112). Despite the low representation of women with basic education, we can infer that there are no statistically significant differences between educational level and the number of methods used (p = 0.174).
Regarding the use of IUDs, we can draw a median profile, being that its users were older women who have had more pregnancies and more children: age 39.03 SD 5.102 vs 32.47 SD 7.231, pregnancies 2.03 vs 1.25, children 1.83 vs 0.94 (p <0.001). The percentage of IUD use is higher in divorced/widowed women than in single or married women (17.4% vs. 13.5 and 0.9, respectively). This difference was statistically significant (p = 0.001). The opposite happens with the combined oral contraceptive pill, in which there is no relation with age, marital status, pregnancies or number of children.
Women with regular follow-up used, in median terms, more methods (2 vs 1), with statistically significant difference (p = 0.004). There were no differences between the perception of the extent of knowledge they have about the method and the number of different methods used.
Discussion
The main strength of this study was its extensive scope in including all the different types of hormonal contraceptive methods. The data was collected from multiple health centers, with a high number of women and valid questionnaires, despite not statistically representative. Women attending health centers were invited regardless of the type of consultation, that is, the amplitude was broader than just users of Family Planning consultations. The language used in the questionnaire was accessible and there was always an available option for the women to explain their own reason(s). To our knowledge, it is the most extensive study regarding this matter ever conducted in Portugal. The limitations are mainly related to memory bias, which necessarily exists in this type of studies. Another limitation is the required representative sample was 352 but only 329 valid questionnaires were obtained.
The desire to become pregnant was the reason of interrupting the method in 20.2%, which is higher than the number found in a large study in women in the same age group13 and another study with a similar size to ours14. Considering that medical advice and intention to become pregnant were two of the main reasons for method discontinuation, as well as the fact that none of the women stopped using a contraceptive because they did not know how to get it, may demonstrate that Family Planning works. This is supported by a recent study by Águas et al, in which advice for the use of the method was made mostly by a physician, and almost half of the women obtain it gratuitously at a Health Center4. Regarding the use of IUDs, our study finds that its users are older women, who have had more pregnancies and children, which is coincident with the literature4,15, as IUDs are usually not the first choice for contraception. The fact that women with regular follow-up used more different contraceptive methods may be explained by the fact that on a regular follow-up there is a trend towards a greater level of doctor-patient communication, and thus a greater predisposition to find the most appropriate method for women, leading to a greater number of methods used.
The widespread use of hormonal contraceptive methods, especially combined oral contraceptives, is consistent with the available national data2,3. As in many other countries in Europe, Brazil and the USA, oral contraceptives are also the most commonly used1,5,8,13,14,16,17.
Regarding the reasons for abandoning a contraceptive method, the results are difficult to compare with those in the existing literature, since characteristics of the population and measures of discontinuation differ across studies. Our results show the main reason for abandonment or change of contraceptive method were ADRs, referred by 25.3% of the women. Although this is one of the main reasons reported in several studies7,14,18,19, the percentage varies greatly, even among studies conducted in the same country: 11.8% for “the pill” in a study by Leite et al.13 to 57.3% in a study by Bahamondes et al.5, both in Brazil and to 25% among young women in the United States20. The most commonly reported ADR also vary between studies, with one study having a similar percentage to ours5 and other study showing that women who report headache are more likely to discontinue21. On the other hand, another study that evaluated the main ADR that motivated a medical consultation, had more women with breast tenderness but, similar to ours, many women with changes in weight and concerns about weight17. The results alert us to cases where women may report symptoms long after the onset of a hormonal contraceptive method which they assume to be a side effect. Knowing the precise reasons why women abandon a specific contraceptive method is of the highest importance in order to improve contraceptive compliance. Medical doctors rely on this information to better advise women and to know what to expect with certain contraceptive methods. Local health authorities and the government also rely on this information to, for example, provide the methods most widely used and accepted by women.
REFERENCES
1. de Zarate TM-A-O, Díaz-Martín T, Martínez-Astorquiza-Corral T. Evaluation of factors associated with noncompliance in users of combined hormonal contraceptive methods: a cross-sectional study: results from the MIA study. BMC Womens Health 2013;13(1):38. [ Links ]
2. Carvalho A de C, Miguel JP. Inquérito Nacional de Saúde 2005/2006. Lisboa: Instituto Nacional de Estatística; 2009.
3. Costa ARR, Palma F, Sá JL, Vicente L, Bombas T, Nogueira AM, et al. Impact of a women's counselling programme on combined hormonal contraception in Portugal - The IMAGINE Study. Eur J Contracept Reprod Health Care. 2011 Dec;16(6):409-17. [ Links ]
4. Águas F, Bombas T, Silva DP da. Avaliação das práticas contracetivas das mulheres em Portugal. Acta Obstétrica E Ginecológica Port 2016;10(3):184-192.
5. Bahamondes L, Pinho F, Melo NR de, Oliveira E, Bahamondes MV. Fatores associados à descontinuação do uso de anticoncepcionais orais combinados. Rev Bras Ginecol Obstet 2011;33(6): 303-309. [ Links ]
6. Halpern V, Lopez LM, Grimes DA, Stockton LL, Gallo MF. Strategies to improve adherence and acceptability of hormonal methods of contraception. Cochrane Libr 2006;1
7. Moreau C, Cleland K, Trussell J. Contraceptive discontinuation attributed to method dissatisfaction in the United States. Contraception 2007;76(4):267-72. [ Links ]
8. Molloy GJ, Graham H, McGuinness H. Adherence to the oral contraceptive pill: a cross-sectional survey of modifiable behavioural determinants. BMC Public Health 2012;12(1):838. [ Links ]
9. Grunloh DS, Casner T, Secura GM, Peipert JF, Madden T. Characteristics Associated With Discontinuation of Long-Acting Reversible Contraception Within the First 6 Months of Use. Obstet Gynecol 2013;122(6):1214-1221. [ Links ]
10. Wellings K, Brima N, Sadler K, Copas AJ, McDaid L, Mercer CH, et al. Stopping and switching contraceptive methods: findings from Contessa, a prospective longitudinal study of women of reproductive age in England. Contraception 2015;91(1):57-66. [ Links ]
11. Tavares M, Barros H. Gravidez não planeada em Portugal. Acta Med Port 1997;10:351-6. [ Links ]
12. Inoue K, Barratt A, Richters J. Does research into contraceptive method discontinuation address women's own reasons? A critical review. J Fam Plann Reprod Health Care 2015;41(4): 292-299. [ Links ]
13. Leite IC, Gupta N. Assessing regional differences in contraceptive discontinuation, failure and switching in Brazil. Reprod Health 2007;4:6. [ Links ]
14. Brunner Huber LR, Hogue CJ, Stein AD, Drews C, Zieman M, King J, et al. Contraceptive use and discontinuation: Findings from the contraceptive history, initiation, and choice study. Am J Obstet Gynecol 2006;194(5): 1290-1295. [ Links ]
15. Sonfield A. Popularity Disparity: Attitudes About The IUD in Europe and the United States. Guttmacher Policy Review 2007;10(4):19-24. [ Links ]
16. Moreau C, Bouyer J, Bajos N, Rodriguez G, Trussell J. Frequency of discontinuation of contraceptive use: results from a French population-based cohort. Hum Reprod 2009;24(6): 1387-1392. [ Links ]
17. Rosenberg MJ, Waugh MS, Burnhill MS. Compliance, counseling and satisfaction with oral contraceptives: a prospective evaluation. Fam Plann Perspect 1998;89-104.
18. Ersek JL, Brunner Huber LR, Thompson ME, Warren-Findlow J. Satisfaction and Discontinuation of Contraception by Contraceptive Method Among University Women. Matern Child Health J 2011;15(4):497-506. [ Links ]
19. Bal MD, Şahin NH. The usage and discontinuation of contraceptive methods. Arch Gynecol Obstet 2011; 284(1): 151-155.
20. Hall KS, Castaño PM, Westhoff CL. The Influence of Oral Contraceptive Knowledge on Oral Contraceptive Continuation Among Young Women. J Womens Health 2014;23(7):596-601. [ Links ]
21. Westhoff CL, Heartwell S, Edwards S, Zieman M, Stuart G, Cwiak C, et al. Oral Contraceptive Discontinuation: Do Side Effects matter?. Am J Obstet Gynecol 2007;196 (4):412.e1-412.e7. [ Links ]
Endereço para correspondência | Dirección para correspondencia | Correspondence
José Eduardo Mendes
USF Mondego
Coimbra, Portugal
E-mail: josemendes.web@gmail.com
Acknowledgements
The authors would like to thank Professor Doutor Luiz Miguel Santiago, Professor Doutor Vítor Rodrigues, Dra. Denise Alexandra, Dra. Ana Raquel Neves, Dra. Maria João Fonseca and Paulo Salvador for reviewing the protocol and questionnaires. We would also like to thank all of our colleagues who assisted in collecting the questionnaires, Filipa Negreiro and Mariana Aparício (Eurotrials) and Clinical Lab, MSD for helping with the data analysis and João Mota for reviewing the final version.
Author Disclosure Statement
No competing financial interests exist.
Recebido em: 20/06/2017
Aceite para publicação: 30/09/2017