Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Acta Obstétrica e Ginecológica Portuguesa
versão impressa ISSN 1646-5830
Acta Obstet Ginecol Port vol.12 no.1 Coimbra mar. 2018
REVIEW ARTICLE/ARTIGO DE REVISÃO
The effect of mode of delivery on female postpartum sexuality
A influência do tipo de parto na sexualidade feminina no pós-parto
Maria do Céu Ferreira*, Catarina da Costa Campos*, Judite Sousa**, Beatriz Santos***
Serviço de Psiquiatria, Hospital de Braga
USF AmareSaúde, ACeS Cávado II, Braga
*Psychiatry Resident, Hospital de Braga
**Family Medicine Resident, USF AmareSaúde, ACeS Cavado II, Braga
***Psychiatry Assistant, Hospital de Braga
Endereço para correspondência | Dirección para correspondencia | Correspondence
ABSTRACT
Studies about the effect of mode of delivery in postpartum sexual function have shown inconsistent results, perpetuating the idea that a cesarean delivery has fewer consequences for women's sexuality.
This systematic review aims to examine the role of mode of delivery in sexual health after childbirth.
The published studies are scarce and quite heterogeneous. Any study has found a solid association between the mode of delivery and specific effects in long-term postpartum sexuality.
In light of this review, cesarean delivery does not seem to be associated with a protective effect in female postpartum sexuality.
Keywords: Delivery; Obstetric and postpartum period; Sexual behavior.
Introduction
The cesarean delivery (CD) rate has been increasing for the last two decades1. Although the maternal morbidity associated with CD is not very high, minor and severe complications associated with delivery are higher after CD (a surgical procedure) than vaginal delivery (VD)2.
The number of CD at maternal request (when a woman explicitly asks for an elective CD in the absence of any medical or obstetric indications) is also increasing3. In this regard, misperceptions about maternal health outcomes after CD and VD have led to this increase2. Common reasons include previous negative birth experiences, fear of childbirth, complications in current pregnancy, the belief that a CD will be safer for the baby, fear of damage the pelvic floor and the perception that it might be protective for preservation of sexual function1,3,4.
Data about the relationship between mode of delivery and postpartum sexual function are very heterogenic and inconclusive, perpetuating the idea that a CD has fewer consequences for women's sexuality.
The aim of this review is to examine the current literature on the role of the mode of delivery in female postpartum sexuality.
Methods
A Medline search was performed for the MeSH terms “delivery”, “obstetric and postpartum period” and “sexual behavior”. Cross-sectional, prospective and retrospective studies published in English language from January 2011 to September 2016 were appraised.
We included studies with more than 80 participants and with clear measurements of sexual function. The studies that did not focus on the relationship between sexual function and mode of delivery and were presented as case reports and short reports were excluded.
Results
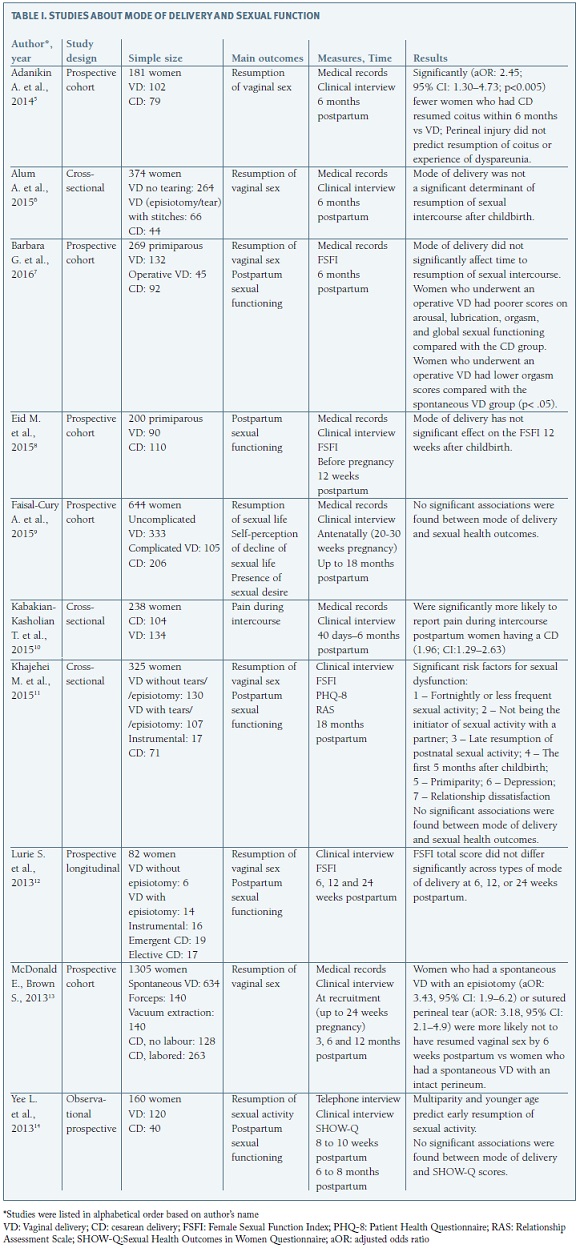
A total of 15 references were found through the Medline search; 5 were excluded through title or abstract analysis for not meeting the inclusion criteria and 10 articles were included in this review and carefully appraised (Table I).
Discussion
Surprisingly, published studies about female sexuality after childbirth are scarce and quite heterogeneous, which makes it difficult to perform a comparison of their results. In fact, one of the main limitations of these studies is related to samples' characteristics. Women having a VD are not a homogenous group and it is important to take into account the different subgroups (intact perineum after spontaneous VD, episiotomy/ /tears or operative VD). The same applies to the CD (scheduled or urgent).
Additionally, it is notable the lack of studies that contain a validated assessment tool for sexual function. Studies analyzed in this review investigated as primary outcomes the timing of resumption of intercourse after childbirth, presence of dyspareunia, and postpartum sexual functioning. This last measure was evaluated through the Female Sexual Function Index (FSFI) in four studies and Sexual Health Outcomes in Women Questionnaire (SHOW-Q) in one study. Only one of the studies assessed the relationship satisfaction through the Relationship Assessment Scale (RAS).
The Female Sexual Functioning Index (FSFI)15 is a brief nineteen-item self-report measure of female sexual function in the previous four weeks. It assesses six domains of sexual function: desire, arousal, lubrication, orgasm, satisfaction, and pain.
Sexual Health Outcomes in Women Questionnaire (SHOW-Q) was developed to assess the impact of pelvic problems in sexual desire, frequency, satisfaction, orgasm, and discomfort16. The Relationship Assessment Scale (RAS)17 is a brief measure of global relationship satisfaction. It consists of seven multiple-choice questions whose items are scored based on a five-point Likert scale. A score equal to or higher than 4 indicates high levels of relationship satisfaction. Research has shown that this score is correlated with other measures of love, sexual attitudes, self-disclosure, commitment, and investment in a relationship18.
Pregnancy and delivery are important periods in women's lives19. Evidence clearly shows that a significant proportion of women experience reduced sexual function during pregnancy, including decreased sexual interest, desire, frequency of sexual intercourse, sexual enjoyment, coital activity, orgasm, and satisfaction. More specifically, female sexual function declines slightly in the first trimester of pregnancy, shows variable patterns in the second trimester, and decreases sharply in the third trimester20.
Postpartum period refers to the period of time required for reproductive organs to return to their pre-pregnancy state, which takes about six weeks21. However, the resumption of sexual intercourse after childbirth does not depend only on the female physical recovery21. This is a complex process that is affected by many factors such as socio-cultural, age, parity, breastfeeding, depression, tiredness, sexual inactivity during the first trimester, postpartum body image and worries about getting pregnant again4.
Postpartum sexual dysfunction is identified in 41-83% of women at 2-3 months postpartum and dyspareunia, specifically, is extremely common in the first 3-6 months postpartum19.
Anatomically, perineal trauma contributes to dyspareunia and has important effects on both the timing and quality of the resumption of sexual intercourse. Breastfeeding may alter sexual function as a result of vaginal dryness produced by the high levels of prolactin and the low estrogen levels. Family structure and ever changing sleep patterns decrease the likelihood of women and their partners have time and privacy to reestablish intimacy.
Cultural and societal dictates regarding the resumption of sexual activity may influence individual couples. Postpartum depression with accompanying loss of sexual desire, or secondary loss of desire, arousal or ability to achieve orgasm resulting from antidepressant medications may also contribute to postpartum sexual dysfunction19.
A recent study20 emphasizes the relation between pre-pregnancy sexuality, sexuality during pregnancy and in the postpartum period. Its results are very interesting: during the first two trimesters of pregnancy and after delivery, sexuality maintains in the same direction as pre-pregnancy patterns and sexual changes during pregnancy have no effect in postpartum sexual function. Based on these findings, the authors conclude that pre-pregnancy sexuality could be protective of sexual function during pregnancy and after delivery.
Another major factor closely associated with postpartum sexual life is the satisfaction with the marital relationship. On one hand, the satisfaction with the marital relationship is strongly associated with sexual desire in the postpartum period, and on the other hand marital conflicts have been implicated in the deterioration of sexual life during the same period19,21. This is an important factor since current studies show that the relationship quality with baby´s father has a great impact on postpartum maternal depression regardless of marital status22. In fact, childbirth can bring significant changes to women's feelings about sexuality, and those who experience significant libido decreases may be vulnerable to feelings of guilt and failure23. In this context, after childbirth, the communication between partners surrounding sexual expectations is especially important, given that many women worry about their partner's sexual satisfaction24. Therefore, considerable attention should be paid to this issue during postnatal care, and sexual difficulties should be addressed during medical visits. This will help dispel myths about what is normal and abnormal, and reduce feelings of anxiety and guilt about resuming sexual activity25.
Conclusions
CD rate is increasing in part due to the perception that it might be protective for preservation of a good sexual function. However, this review allows a systematization of available studies in this field and supports the lack of evidence to recommend an elective CD for the purpose to preserve postpartum sexual health. In fact, other factors should be considered since postpartum sexual function is a multidimensional phenomenon affected by biological, psychological, social, interpersonal, and cultural factors.
Therefore, it is very important that clinicians discuss during prenatal and postpartum care this issue in order to provide to both women and their partners more information about the most appropriate mode of delivery and postpartum sexual health.
REFERENCES
1. Bodner K, Wierrani F, Grünberger W, Bodner-Adler B. Influence of the mode of delivery on maternal and neonatal outcomes: a comparison between elective cesarean section and planned vaginal delivery in a low-risk obstetric population. Arch Gynecol Obstet. 2011;283(6):1193-1198. [ Links ]
2. Li WY, Liabsuetrakul T, Stray-Pedersen B. Effect of mode of delivery on perceived risks of maternal health outcomes among expectant parents: a cohort study in Beijing, China. BMC Pregnancy Childbirth. 2014;14:12. [ Links ]
3. Sharpe AN, Waring GJ, Rees J, McGarry K, Hinshaw K. Caesarean section at maternal request-the differing views of patients and healthcare professionals: a questionnaire based study. Eur J Obstet Gynecol Reprod Biol. 2015;192:54-60. [ Links ]
4. Yeniel AO, Petri E. Pregnancy, childbirth, and sexual function: perceptions and facts. Int Urogynecol J. 2014;25(1):5-14. [ Links ]
5. Adanikin AI, Awoleke JO, Adeyiolu A, Alao O, Adanikin PO. Resumption of intercourse after childbirth in southwest Nigeria. Eur J Contracept Reprod Health Care. 2015;20(4):241-248. [ Links ]
6. Alum AC, Kizza IB, Osingada CP, Katende G, Kaye DK. Factors associated with early resumption of sexual intercourse among postnatal women in Uganda. Reprod Health. 2015;12:107. [ Links ]
7. Barbara G, Pifarotti P, Facchin F, Cortinovis I, Dridi D, Ronchetti C, Calzolari L, Vercellini P. Impact of Mode of Delivery on Female Postpartum Sexual Functioning: Spontaneous Vaginal Delivery and Operative Vaginal Delivery vs. Cesarean Section. J Sex Med. 2016;13(3):393-401. [ Links ]
8. Eid MA, Sayed A, Abdel-Rehim R, Mostafa T. Impact of the mode of delivery on female sexual function after childbirth. Int J Impot Res. 2015;27(3):118-120. [ Links ]
9. Faisal-Cury A, Menezes PR, Quayle J, Matijasevich A, Diniz SG. The relationship between mode of delivery and sexual health outcomes after childbirth. J Sex Med. 2015;12(5):1212-1220. [ Links ]
10. Kabakian-Khasholian T, Ataya A, Shayboub R, El-Kak F. Mode of delivery and pain during intercourse in the postpartum period: findings from a developing country. Sex Reprod Healthc. 2015;6(1):44-47. [ Links ]
11. Khajehei M, Doherty M, Tilley PJ, Sauer K. Prevalence and risk factors of sexual dysfunction in postpartum Australian women. J Sex Med. 2015;12(6):1415-1426. [ Links ]
12. Lurie S, Aizenberg M, Sulema V, Boaz M, Kovo M, Golan A, Sadan O. Sexual function after childbirth by the mode of delivery: a prospective study. Arch Gynecol Obstet. 2013;288(4):785-792. [ Links ]
13. McDonald EA, Brown SJ. Does method of birth make a difference to when women resume sex after childbirth? BJOG. 2013;120(7):823-830. [ Links ]
14. Yee LM, Kaimal AJ, Nakagawa S, Houston K, Kuppermann M. Predictors of postpartum sexual activity and function in a diverse population of women. J Midwifery Womens Health. 2013;58(6):654-661. [ Links ]
15. Rosen R, Brown C, Heiman J, Leiblum S, Meston C, Shabsigh R, Ferguson D, D'Agostino R Jr. The Female Sexual Function Index (FSFI): a multidimensional self-report instrument for the assessment of female sexual function. J Sex Marital Ther. 2000;26 (2):191-208. [ Links ]
16. Learman LA, Huang AJ, Nakagawa S, Gregorich SE, Kuppermann M. Development and validation of a sexual functioning measure for use in diverse women's health outcome studies. Am J Obstet Gynecol. 2008;198(6):710.e1-8; [ Links ] discussion 710.e8-9.
17. Vaughn MJ, Baier MEM. Reliability and validity of the relationship assessment scale. Journal of Family Therapy.1999; 27: 137-147. [ Links ]
18. Hendrick SS.A generic measure of relationship satisfaction. Journal of Marriage and Family.1988; 50: 93-98. [ Links ]
19 Leeman LM, Rogers RG. Sex after childbirth: postpartum sexual function. Obstet Gynecol. 2012;119(3):647-655.
20. Yıldız H. The relation between prepregnancy sexuality and sexual function during pregnancy and the postpartum period: a prospective study. J Sex Marital Ther. 2015;41(1):49-59.
21. Leal I, Lourenço S, Oliveira RV, Carvalheira A, Maroco J. The impact of childbirth on female sexuality. PSYCHOLOGY, COMMUNITY & HEALTH. 2012;1 (1):127-139 [ Links ]
22. Akincigil A, Munch S, Niemczyk KC. Predictors of maternal depression in the first year postpartum: marital status and mediating role of relationship quality. Soc Work Health Care. 2010;49(3):227-244. [ Links ]
23. Woolhouse H, McDonald E, Brown S. Women's experiences of sex and intimacy after childbirth: making the adjustment to motherhood. J Psychosom Obstet Gynaecol. 2012;33(4):185-190. [ Links ]
24. Hipp LE, Kane Low L, van Anders SM. Exploring women's postpartum sexuality: social, psychological, relational, and birth-related contextual factors. J Sex Med. 2012;9(9):2330-41. [ Links ]
25. O'Malley D, Higgins A, Smith V. Postpartum sexual health: a principle-based concept analysis. J Adv Nurs. 2015;71(10):2247-2257. [ Links ]
Endereço para correspondência | Dirección para correspondencia | Correspondence
Maria do Céu Ferreira
Hospital de Braga
Portugal
E-mail: ceu@live.com.pt
Recebido em: 26/05/2017
Aceite para publicação: 11/07/2017