Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Acta Obstétrica e Ginecológica Portuguesa
versão impressa ISSN 1646-5830
Acta Obstet Ginecol Port vol.11 no.4 Coimbra out. 2017
CASE REPORT/CASO CLÍNICO
Synchronous trifocal invasive breast carcinoma - a case report
Carcinoma de mama invasivo trifocal síncrono - um caso clínico
Mariana Souto Miranda*, Ângela Melo**, Rita Sousa***, Luis Sá****
Instituto Português de Oncologia, Coimbra
*Interna do Internato Complementar de Ginecologia do Hospital Prof Doutor Fernando Fonseca
**Interna do Internato Complementar de Ginecologia do Hospital São Teotónio
***Assistente Hospitalar do Serviço de Ginecologia do IPO de Coimbra
****Director de Serviço de Ginecologia do IPO de Coimbra
Endereço para correspondência | Dirección para correspondencia | Correspondence
ABSTRACT
We report the case of a 50-year-old female diagnosed with bilateral breast carcinoma. The patient was submitted to bilateral mastectomy with sentinel LN biopsy and immediate breast reconstruction. The histopathology diagnosed a trifocal bilateral breast carcinoma. The incidence of bilateral breast carcinoma is increasing. There are no clear treatment guidelines for BBC.
Keywords: Bilateral breast cancer, synchronous; Trifocal.
Introduction
Breast cancer (BC) is the most frequently diagnosed malignancy and the leading cause of cancer death in women. Bilateral BC (BBC) is a rare presentation, representing 2-5% of all breast malignancies1. This is the case of a 50-year-old female with bilateral trifocal invasive BC.
Case Report
A 50-year-old female presented with two small lumps on both breasts with a 12month evolution. First menses at age 10, two pregnancies (first at age 27) and breastfed for two weeks. She used combined oral contraception for 20 years. No relevant medical history or family history of BC. She smokes 20 cigarettes a day.
On clinical examination, two small solid breast lumps were palpated - in the upper inner quadrant of the right breast and in the lower inner quadrant of the left breast. A right axillary lymph-node (LN) was detected. General physical and systemic examinations were normal.
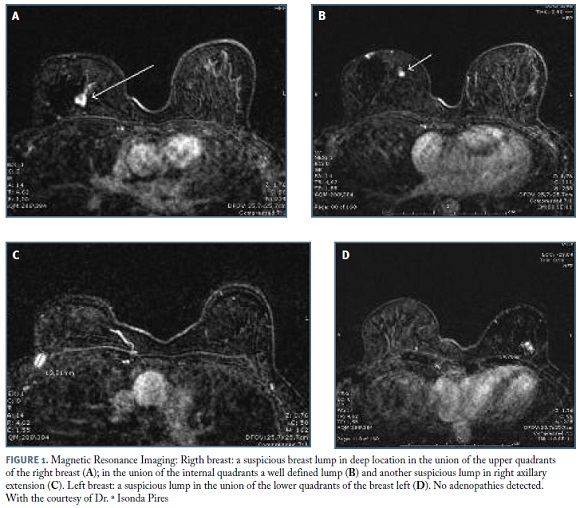
Mammography and ultrasonography revealed three lumps - one with 13mm in the union of the upper quadrants of the right breast, other in right axillary extension with 15mm and the third in the union of the lower quadrants of the left breast with 7mm. Ultrasonography directed microbiopsies revealed an invasive lobular carcinoma in the upper quadrant of the right breast, Grade1 (G1), with estrogens receptor status (ER)-100%, progesterone receptor status (PR)-8%, no HER-2 overexpression and Ki-67 expression of 14%. On the axillary extension was an invasive BC, not otherwise specified (NOS), G1, with ER-100%, PR-100%, no HER-2 overexpression and Ki-67 expression of 13%. On the left breast the histology was invasive BC, NOS, G1, with ER-100%, PR-0%, no HER-2 overexpression and Ki-67 expression of 5%. Axillary LN cytology, through ultrasound guided fine needle aspiration, was negative for malignancy.
Complementary exams revealed serum levels of carcinoembryonic antigen raised - 7,41 ng/mL and normal cancer antigen 15-3. Compute tomography scan (CT), magnetic resonance imaging (MRI) and skeletal scintigram showed no distant metastization.
The tumors were classified in T2N0 in the right breast and T0N0 in the left breast (Figure 1). The patient was submitted to bilateral skin-sparing mastectomy with sentinel LN biopsy and immediate breast reconstruction with prosthetic implants. The post operative period was uneventful, with good recovery.
Histopathology of the right breast confirmed an invasive lobular carcinoma, G1 with associated lobular carcinoma in situ and an invasive BC, NOS, G1- pathologic stage pT1bpN0 (sn). On the left breast, an invasive BC, NOS, G1 with an associated low grade ductal carcinoma in situ with solid pattern of 1,1cm - pathologic stage pT1cpN0 (sn). On the right breast, the distance from the tumor of the upper quadrants to the margin was under 0,01mm, and postoperative radiotherapy was decided.
The patient did external beam radiotherapy into the right breast area (50 Gy in 25 fractions over 5 weeks) and is currently on adjuvant hormonal therapy with tamoxifen.
This patient underwent appropriate genetic counseling and testing for hereditary breast cancer which was negative.
Patient is on follow-up, without clinical or imaging signs of recurrence after 2 year.
Discussion
Due to improved life expectancy after BC treatment and routine use of contra-lateral breast mammography in newly diagnosed BC, the incidence of BBC is increasing2. The tumor in the contralateral breast can be synchronous (within 6 months of the primary tumor) or metachronous (afterwards)2. In our case, although symptoms started 12 months earlier, all tumors were diagnosed simultaneously. A tumor in contralateral breast may be a second primary tumor or metastasis from the first tumor. Despite the existence of methods such as cDNA microarray, the criteria for the diagnosis of second primary BC proposed by Chaudary et al.3 in 1984 demonstration of in situ disease in the contralateral tumor, both carcinomas with different histological types and different grades have been the most widely accepted method to distinguish second primary lesion from metastatic lesion4. Without widespread systemic metastases, contralateral BC are generally separate primary tumors, as defined in this report. Concordance rates of ER and PR status and Her2 expression between two tumors are usually higher than 80%. RS Saad et al.5 and Imyanitov et al.6 demonstrated that BBC can be clonally independent events, despite having similar characteristics. In our case, different histology suggested different primary tumors.
The etiology is not clearly defined but there are known risk factors for BBC. Women with a diagnosed BC have 2-6 greater relative risk of developing contralateral BC1. Lobular histology is a recognized risk factor for BBC2 in our case, the right breast had a lobular carcinoma but a different histology was diagnosed in the left breast. Bilaterality is more commonly seen in cases with Her2 overexpression. In one study, Her2 overexpression was found in 71% against 35% in unilateral cancers7. In another, Her2 was overexpressed in 44% of all bilateral tumor tissues, regardless of the first and second tumors, higher than the HER2 positivity rate of 26% in unilateral BC4- this case showed no HER2 overexpression. Other risk factors include family history, genetic predisposition, younger age at diagnosis and nulliparity. Age was considered the most important predictor for contralateral BC the earlier a woman develops a first BC, the higher the risk of developing a contralateral tumor8. Because of her bilateral breast cancer at a young age, she met the National Comprehensive Cancer Network (NCCN) criteria for BRCA1/2 mutation testing. Key criteria for hereditary cancer risk evaluation are breast cancer diagnosed before the age of 50, triple-negative breast cancer diagnosed before 60, two or more primary breast cancers, invasive ovarian or fallopian tube cancer, or peritoneal cancer, male breast cancer, Ashkenazi Jewish ethnicity.
There are no clear treatment guidelines for BBC, the optimal surgical management is not well defined. The majority of patients undergo bilateral mastectomy. Breast conservation is rarely chosen due to stress from the diagnosis8. For patients who undergo breast-conserving surgery, the follow-up and risk of recurrence as well as the need for bilateral breast irradiation are all factors in decision making. MRI is recommended when breast conservation is planned, to rule out multifocality or multicentricity, more common in BBC2. Adjuvant therapy is based on the higher risk tumor.
Survival in BBC is equivalent or moderately lower than unilateral BC2 but synchronous tumors have poorer survival than metachronous8. Multifocality is not amongst prognostic factors in international BC guidelines, but recent studies associate BC multifocality with higher general mortality rates and lower survival9.
Conclusion
We report the case of a woman with three different tumors simultaneously. Histology, grade, hormone receptor status, Her2 and Ki67 expression were different. These and the presence of associated in situ component exclude metastatic origin of these tumors. One tumor was clinically unapparent and detected during the diagnosis of the others, supporting the importance of complete imaging screening at primary diagnosis.
REFERENCES
1. Kumar V, Kappikeri S., Kriplani, A. Bilateral synchronous carcinoma breast - a rare case presentation. SpringerPlus 2015; 4:193. [ Links ]
2. Padmanabhan N., Subramanyan A., Radhakrishna, S. Synchronous Bilateral Breast Cancers. J Clin Diagn Res. 2015 Sep; 9(9): XC05-XC08.
3. Chaudary MA, Millis RR, Hoskins EOL, Halder M, Bulbrook RD. Bilateral breast cancer: A prospective study of disease incidence. Br J Surg 1984;71:711-714. [ Links ]
4. Gong SJ, Rha SY, Jeung HC, Roh JK, Yang WI, Chung HC. Bilateral breast cancer: differential diagnosis using histological and biological parameters. Jpn J Clin Oncol. 2007 Jul;37(7):487-492. [ Links ]
5. Saad RS, Denning KL, Finkelstein SD, Liu Y, Pereira TC, Lin X, Silverman JF. Diagnostic and prognostic utility of molecular markers in synchronous bilateral breast carcinoma. Mod Pathol. 2008;21(10):1200-1207. [ Links ]
6. Imyanitov EN, Suspitsin EN, Grigoriev MY, Togo AV, Kuligina ESh, Belogubova EV, et al. Concordance of allelic imbalance profiles in synchronous and metachronous bilateral breast carcinomas. Int J Cancer. 2002;100(5):557-564. [ Links ]
7. Safal M, Lower EE, Hasselgren PO, Hungness ES, Gazder P, Aron B, et al. Bilateral synchronous breast cancer and HER-2/neu overexpression. Breast Cancer Res Treat. 2002;72(3):195-201. [ Links ]
8. Elrasheid A. H. Kheirelseid, Hanzali Jumustafa, Nicola Miller, Catherine Curran, Karl Sweeney, et al. Bilateral breast cancer: analysis of incidence, outcome, survival and disease characteristics. Breast Cancer Research and Treatment. Springer Verlag, 2010, 126 (1), 131-140.
9. Boros M, Voidazan S, Moldovan C, Georgescu R, Toganel C, Moncea D et al. Clinical implications of multifocality as a prognostic factor in breast carcinoma a multivariate analysis study comprising 460 cases. Int J Clin Exp Med. 2015 Jun 15;8(6):9839-9846. [ Links ]
Endereço para correspondência | Dirección para correspondencia | Correspondence
Mariana Souto Miranda
E-mail: marianasoutomiranda@gmail.com
Recebido em: 15/11/2016
Aceite para publicação: 25/12/2016