Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Acta Obstétrica e Ginecológica Portuguesa
versão impressa ISSN 1646-5830
Acta Obstet Ginecol Port vol.10 no.4 Coimbra dez. 2016
CASO CLÍNICO/CASE REPORT
Giant placental chorioangioma and polyhydramnios
Grande corioangioma placentar e polihidrâmnios
Ana Paula Reis*, Catarina Paiva*, Tânia Lima**, Rosa Zulmira***, Ana Cunha***
Centro Hospitalar do Porto/Centro Materno Infantil do Norte, Porto
*Assistente Hospitalar de Ginecologia e Obstetrícia
**Interna de Ginecologia e Obstetrícia
***Assistente Hospitalar Graduada de Ginecologia e Obstetrícia
Endereço para correspondência | Dirección para correspondencia | Correspondence
ABSTRACT
Chorioangioma is the most common benign tumor of the placenta, occurring in 1% of all pregnancies. Small chorioangiomas tend to remain asymptomatic. Giant chorioangiomas have been associated with a number of severe fetal complications and high perinatal mortality. We report a case of a giant chorioangioma diagnosed in the third trimester of pregnancy. The size of tumor and the amniotic fluid index increased from the time of diagnosis to the end of pregnancy. A term labour was uncomplicated and a healthy newborn was delivered. Macroscopic and microscopic examination of the placenta was consistent with placental chorioangioma.
Keywords: Giant chorioangioma; Complications; Amniotic fluid index.
Background
The primary neoplastic disorders of the placenta include a large group of conditions that are classified in two different groups - trophoblastic and nontrophoblastic diseases. Chorioangioma is the most frequent benign nontrophoblastic tumor of the placenta. It is defined by the abnormal proliferation of vessels arising from chorionic tissue and has an estimated prevalence of 1%1-2.
The majority of them are single, small and intraplacental. By virtue of their size, chorioangiomas are very unlikely to be detected during gross pathological examination, unless the placenta is carefully sectioned. Small chorioangiomas tend to remain asymptomatic and rarely complicate the course of the pregnancy.3
Large or giant chorioangiomas, defined as measuring more than 4-5 cm in diameter, have an estimated prevalence varying from 1:9.000 to 1:50.000 pregnancies, and have been associated with a number of maternal and fetal complications. Obstetric complications include: polyhydramnios, premature labour, cervical incompetence, placental abruption, increased risk of caesarean section, malpresentation and postpartum haemorrhage. Fetal complications include haemolytic anaemia, thrombocytopenia, nonimmunologic fetal hydropsis, growth restriction, hepatosplenomegaly, cardiomegaly, congestive heart failure, umbilical vein thrombosis and intrauterine fetal and neonatal death3-7.
Doppler ultrasound examination is the gold standard in primary diagnosis of chorioangioma. Magnetic resonance imaging is used only in suspicious cases, while the computed tomography technique has a limited role in the diagnosis, mainly because of the high radiation risk and poor tissue differentiation8-10. Serum and/or amniotic fluid levels of alpha-fetoprotein (AFP) can be increased in chorioangiomas cases, but increased levels of AFP are not pathognomonic for this pathology11.
In view of the associated high perinatal morbidity rate (30-40%), a number of therapeutic interventions have been attempted, with limited success in most cases12-16. When polyhydramnios exists, amniodrainage is a useful tool as well as intrauterine transfusions in the presence of fetal anemia. In fact, these are the most common therapeutic procedures in giant chorioangiomas with favorable results. Other techniques have been used as injection of absolute alcohol, endoscopic laser coagulation and interstitial laser therapy17.
We present a case of polyhydramnios caused by a giant placental chorioangioma, with favourable outcome.
Case Report
The authors report a case of a 35-year-old Caucasian multiparous and healthy woman that was referred to our hospital for ultrasound evaluation due to a suspected placental mass at 31 weeks’ gestation. The pregnancy had been uneventful and previous fetal ultrasounds were reported as normal. The oral glucose tolerance test made at the 25th week of gestation was negative.
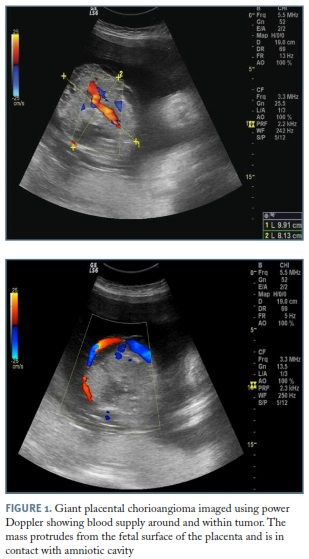
The ultrasound revealed a well-defined, round-shaped, echogenic and heterogeneous placental mass measuring 7x6.6 cm arising from the chorionic plate. Color Doppler ultrasound showed a highly vascularised mass, with blood flow within and around the tumor, leading to a presumed diagnosis of placental chorioangioma. The placenta was located in the posterior uterine wall. The estimated fetal weight was calculated at the 14th percentile for gestational age. Doppler blood flow studies of the middle cerebral artery, umbilical artery, and ductus venosus were normal. The amniotic fluid index (AFI) was within normal range.
Follow-up ultrasound scans for fetal growth, mass size and Doppler studies were conducted every 2 weeks. During this period, the fetus maintain its growth around 14th percentile. The placental tumor size increased gradually, measuring 11.6x10 cm at 36 weeks’ gestation (Figure 1). The volume of amniotic fluid increased gradually and AFI was 30 cm. Surveillance occurred at outpatient care until 37 weeks. As the patient was assimpatomatic, no intervention was performed to treat polyhydramnios and no steroids were administered to induce lung maturation.
After uncomplicated and spontaneous vaginal delivery at the 37th week of gestation, the placenta was delivered completely. A healthy female 2610 g baby was born with an Apgar score of 9 and 10, respectively, at 1 and 5 minutes. Two days after delivery, mother and infant both well were discharged from the Hospital.
The placenta weighted 1111 g (above P90 for gestational age) and measured 26x22x3.7 cm. In macroscopic assessment of the placenta, a single well-circumscribed and compact mass measuring 12x8x7.5 cm was found on chorionic plate, with red colour and elastic consistency, surrounded by oedematous and multicistic placental parenchyma (Figure 2). Microscopically, hemangiomatous proliferation was seen. Histologic exam was consistent with placental chorioangioma.
Discussion
Chorioangioma is the most common benign tumor of the placenta, occurring in 1% of all pregnancies1-2. Ultrasonography with colour Doppler is the gold standard in the diagnosis of placental chorioangioma8-10. In the presented case, the tumor was diagnosed at 31 weeks’ gestation. It might not be diagnosed earlier due to its small size or the tumor was not found at all. A well-circumscribed rounded, echogenic lesion near the chorionic surface and protruding into the amniotic cavity is a common characteristic and documenting increased blood flow by colour Doppler can assist in distinguishing these lesions from other placental masses such as placental teratoma, degenerating fibroid and placental hematoma.
Management of chorioangioma is usually conservative. No specific treatment is needed in asymptomatic cases. However a careful monitoring with serial ultrasound examinations is needed to predict early complications3-5. In our case, follow-up ultrasound scans for fetal growth, mass size and Doppler studies were conducted every 2 weeks. The placental tumor size increased gradually, as well as, the AFI.
The mechanism of polyhydramnios formation in cases of placental chorioangioma is not completely understood and several theories have been postulated to explain this phenomenon. Increased intravascular pressure caused by obstruction of the blood flow by the tumor near the umbilical cord insertion may increase transudation into the amniotic cavity, which is in intimate contact with the tumor. The large surface area of the enlarged vessels of the chorioangioma may also predispose to the increase transudation. Polyhydramnios can also be explained by the partial placental insufficiency caused by shunting of the fetal blood into the vessels of the chorioangioma. The increase of AFI can be linked to increased urine production, associated with fetal hyperdynamic circulation related to shunting of blood or fetal anaemia18. In our case, the existence of polyhydramnios without a concomitant increase in middle cerebral artery peak systolic velocity (fetal anaemia), support the placental transudate hypothesis.
Giant chorioangiomas are rare, associated with a high prevalence of pregnancy complications and a poor perinatal outcome3-7. If complications develop late in pregnancy, delivery should be considered, depending on fetal maturity and the available neonatal support. However, pregnancies with the most severe fetal complications often occur late in second trimester. The use of amniodrainage and intrauterine blood transfusion are well established and applied when polyhydramnios or fetal anaemia complicate a pregnancy with placental chorioangioma. Interventions to block the vascular supply to the tumor such as endoscopic laser coagulation and injection of absolute alcohol are commonly used13-16.
However, despite the giant size in this case (12x8x7.5 cm) and the increased AFI, there were no significant complications and amniodrainage was not performed.
REFERENCES
1. Miliaras D, Anagnostou E, Papoulidis I, Miliara X. Non-trophoblastic tumor of the placenta with combined histologic features of chorioangioma and leiomyoma. Placenta 2011; 32:102-104. [ Links ]
2. Fox H. Sebire NJ: Non-trophoblastic tumors of the placenta. In Pathology of the Placenta, 3rd edition. Philadelphia: Saunders Elsevier; 2007:401-430. [ Links ]
3. Zanardini C, Papageorghiou A, Bhide A, Thilaganathan B. Giant placental chorioangioma: natural history and pregnancy outcome. Ultrasound Obstet Gynecol 2010; 35:332-336. [ Links ]
4. Sepulveda W, Alcalde JL, Schnapp C, Bravo M: Perinatal outcome after prenatal diagnosis of placental chorioangioma. Obstet Gynecol 2003; 102:1028-1033. [ Links ]
5. Bashiri A, Furman B, Erez O, Wiznitzer A, Holcberg G, Mazor M. Twelve cases of placental chorioangioma. Pregnancy outcome and clinical significance. Arch Gynecol Obstet 2002; 266:53-55. [ Links ]
6. Galimberti A, Jain S: Placental chorioangioma as a cause of maternal hydrops syndrome. J Obstet Gynaecol 2000; 20:91. [ Links ]
7. Sivasli E, Tekşam O, Haliloğlu M, Güçer S, Orhan D, Gürgey A, Tekinalp G. Hydrops fetalis associated with chorioangioma and thrombosis of umbilical vein. Turk J Pediatr 2009; 51:515-518.
8. Elsayes KM, Trout AT, Friedkin AM, Lui PS, Bude RO, Platt JF, Menias CO. Imaging of the placenta: a multimodality pictorial review. Radiographics. 2009; 29:1371-1391. [ Links ]
9. Sepulveda W, Aviles G, Carstens E, Corral E, Perz N. Prenatal diagnosis of solid placental masses; the values of color flow imaging. Ultrasound Obstet Gynecol 2000; 16:554-558. [ Links ]
10. Durin L, Barjot P, Herlicoviez M. Placental chorioangioma, value of ultrasonography: report of two cases. J Radiol 2002; 83:739-741. [ Links ]
11. Androutsopoulos G, Gkogkos P, Decavalas G. Mild-trimester maternal serum HCG and alpha fetal protein levels: clinical significance and prediction of adverse pregnancy outcome. Int J Endocrinol Metab. 2013; 11: 102-106. [ Links ]
12. Batukan C, Holzgreve W, Danzer E, Bruder E, Hösli I, Tercanli S. Large placental chorioangioma as a cause of sudden intrauterine fetal death. A case report. Fetal Diagn Ther 2001; 16:394-397. [ Links ]
13. Bhide A, Prefumo F, Sairam S, Carvalho JS, Thilaganathan BT. Ultrasound-guided interstitial laser therapy for the treatment of placental chorioangioma. Obstet Gynecol 2003; 102:1189-1191. [ Links ]
14. Sepulveda W, Wong A, Herrera L, Dezerega V, Devoto JC. Endoscopic laser coagulation of feeding vessels in large placental chorioangiomas: report of three cases and review of invasive treatment options. Prenat Diagn 2009; 29: 201-206. [ Links ]
15. Deren O, Ozyuncu O, Onderoglu LS, Durukan T. Alcohol injection for the intrauterine treatment of chorioangioma in a pregnancy with transfusion resistant fetal anemia: a case report. Fetal Diagn Ther 2007; 22:203-205. [ Links ]
16. Ercan CM, Coksuer H, Karasahin KE, Alanbay I, Baser I. Combined approach in a large placental chorioangioma case with intratumoral alcohol injection, cordocentesis, IU transfusion, and amnioreduction. Fetal Pediatr Pathol. 2012; 31:374-378. [ Links ]
17. Garcia-Diaz L, Carreto P, Costa-Pereira S, Antiñolo G. Prenatal management and perinatal outcome in giant placental chorioangioma complicated with hydrops fetalis, fetal anemia and maternal mirror syndrome. BMC Pregnancy and Childbirth 2012; 12:72-76. [ Links ]
18. Kirkpatrick AD, Podberesky DJ, Gray AE, McDermott JH. Placental Chorioangioma. RadioGraphics 2007; 27:1187-1190. [ Links ]
Endereço para correspondência | Dirección para correspondencia | Correspondence
Ana Paula Reis
Centro Hospitalar do Porto (CHP)
Espinho, Portugal
E-mail: anapreis1982@gmail.com
The authors declare no conflict of interest.
Recebido em: 21/12/2015
Aceite para publicação: 6/3/2016