Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Psicologia, Saúde & Doenças
Print version ISSN 1645-0086
Psic., Saúde & Doenças vol.21 no.2 Lisboa Aug. 2020
https://doi.org/10.15309/20psd210222
Self-image in patients with acromegaly: a cross-sectional study in Brazil
Autoimagem em pacientes com acromegalia: um estudo transversal no Brasil
Michelle Cintra1, Andressa Jesus1, Elizza Barreto1, Irani Silva1, Lis Viana1, Luana Teixeira1, & Martha Castro2
1Department of Psychology, CEDEBA - Center of Diabetes and Endocrinology of the State of Bahia, Brazil, michelleqv@gmail.com, andressa.oliveira29@gmail.com, elizza_sb@hotmail.com, nysantos.010@hotmail.com, lisviana15@hotmail.com, luanacerqueirat@gmail.com
2Bahiana School of Medicine and Public Health. Federal University of Bahia, Brazil, marthamccastro@gmail.com
Endereço para correspondência | Dirección para correspondencia | Correspondence
ABSTRACT
Acromegaly is characterized by excess growth hormone (GH) in adults between 30 and 50 years. The disease presents clinical manifestations, such as growth of the extremities and facial asymmetry. The main objective of the study was to describe the psychosocial impacts of physical alterations of acromegaly on self - image. A cross-sectional retrospective study was carried out in a sample of 71 patients from the state of Bahia, using the Acromegaly Quality of Life Questionnaire. The focus group technique was also used, from which a content analysis explored psychosocial aspects. Most participants look different in the mirror. Most women, however, perceive themselves as ugly and look awful in their photographs, while more than half of the men perceive the look of the other on account of their physical appearance. There was a significant correlation between self-concept change and mood. The qualitative results indicated that physical changes are more uncomfortable than other manifestations, since they impact on areas of life such as emotional and work. It was evidenced the impact that the alteration in the self - image can bring to the social and psychological level in the life of the acromegalic.
Keywords: Acromegaly, self-image, psychosocial impact, focus group, clinical manifestations
RESUMO
A acromegalia é caracterizada pelo excesso do hormônio de crescimento (GH) em adultos entre 30 e 50 anos. A doença apresenta manifestações clínicas, como crescimento das extremidades e assimetria facial. O principal objetivo do estudo foi descrever os impactos psicossociais das alterações físicas da acromegalia na autoimagem. Foi realizado um estudo retrospectivo de corte transversal em uma amostra de 71 pacientes do estado da Bahia, utilizando o questionário AcroQol (Questionário de Qualidade de Vida em Acromegalia). Foi utilizada também a técnica de grupo focal, onde a partir de uma análise de conteúdo foram explorados aspectos psicossociais. Os participantes de ambos os gêneros, em sua maioria, se veem diferentes no espelho e percebem que há partes no corpo que são demasiado grandes por conta da patologia. Já boa parte das mulheres se percebem feias e se veem horrorosas nas fotografias, enquanto mais da metade dos homens percebem o olhar do outro por conta do seu aspecto físico. Os resultados qualitativos indicaram, como maior incômodo as mudanças físicas em relação a outras manifestações clínicas, pois impactam em áreas da vida como a emocional e laboral. Foi evidenciado o impacto que a alteração na autoimagem pode trazer a nível social, psicológico e emocional na vida do acromegálico.
Palavras-chave: Acromegalia, autoimagem, impacto psicossocial, grupo focal, manifestações clínicas
Acromegaly is a chronic, rare and insidious disease caused by increased secretion of growth hormone (GH) due to a benign tumor located in the pituitary gland, affecting adults between 30 and 50 years, with no gender distinction. This pathology presents higher rates of mortality and morbidity in relation to the healthy population (Abreu et al., 2016; Adelman, Liebert, Nachtigall, Lamerson, & Bakker, 2013; Varadhan, Reulen, Brown, & Clayton, 2016) due to the secondary damage it causes in other systems, such as cardiovascular, metabolic and possible cancer cases (Boguszewski & Ayuk, 2016, Matta et al., 2008; Melmed et al., 2013).
Treatment includes surgery for withdrawal or reduction of the tumor, radiation therapy and drug treatment with dopamine agonists and somatostatin analogues and antagonist receptors of GH (Adelman et al., 2013; Brazil, 2013; Matta et al., 2008). These treatments minimize the impact of physical changes due to acromegaly, since it reduces edema and joints inflammation, but does not reverse all changes, especially in the cases of late diagnosis (Matta et al., 2008; Webb, 2006).
It is noteworthy that typical facial and acral changes develop insidiously, but although they are visibly recognizable, they are not easily associated with the pathology by the patients as well as by their relatives and even by the health professionals. Thus, there is a delay between the time symptoms appear and when the diagnosis is made (Melmed, 2006; Molitch, 1992; Nabarro, 1987; Reid et al., 2010).
Holdaway and Rojasoorya (1999), in their studies, found that this delay varies from 6.6 to 10.2 years, obtaining an average of 8 years between the perception of symptoms and the diagnosis of the disease. In this sense, the diagnosis and early treatment of comorbidities avoids long-term complications (Melmed et al., 2013) and irreversible damage (Lavrentaki, Paluzzi, Wass, & Karavitaki, 2017; Matta et al., 2008).
Thus, even if the patient reaches control of the disease, some changes already become permanent, with impacts on appearance being the most affected aspect (Matta et al., 2008). Among the clinical manifestations, it may be noticed excessive acral growth, soft tissue swelling, arthralgia, maxillary prognathism, mild hyperglycemia, headache, sleep apnea, hypertension, erectile dysfunction, menstrual disorders, among others (Melmed, 2006; Molitch, 1992). Orofacial changes also occur, such as protrusion of the eyebrows, enlargement of the nose and ears, thickening of the lips, skin wrinkles and nasolabial folds, mandibular prognathism, resulting in dental malocclusion and increased interdental spacing (Nabarro, 1987; Naves, Mercado, Duarte, Vilar, & Vilar, 2016; Melmed & Kleinberg, 2003; Molitch, 1992).
Regarding facial changes, in a study with one hundred and twenty patients of both sexes, between 5 and 10 years of acromegaly biochemical remission, it was verified that the greatest concern with physical appearance, especially with the face, is twice as common among women than men (Roerink et al., 2015).
Cutaneous manifestations are also identified, as the example brought by Zanini, Oshiro, Paschoal, Paschoal, and Timoner (2004), as increased sweating, often causing bromidrosis, that is, unpleasant smell in the regions that sweat, thickening of the hand palms and soles of the feet, increased sebaceous secretion, excessive hair growth and later tendency to its rarefaction, nails with increased thickness, hyperpigmentation of the skin due to the increase of the melanotrophic hormone, especially in photo exposed areas, besides the fact that, when touched, the skin of people with acromegaly has a sticky, moist and swollen appearance (Vilar, Vilar, Lyra, Lyra, & Naves, 2017).
Furthermore, it is necessary to emphasize that the pathology leads to systemic complications and impairments in quality of life (Webb, 2006), which can lead to neuropsychological alterations, such as impairments in cognition, anxiety and depression symptoms, interruption of interpersonal relationships, emotional changes, personality alterations due to diminished self-esteem, as well as distortion of self-image (Fava, Sonino, & Morphy, 1993; Katznelson et al., 2014; Yedinak & Fleseriu, 2014).
The impacts on perceived self-image in patients with acromegaly are associated with the described physical changes, which are observed as a result of the pathology diagnosis. Schilder (1999) states that self-image is the mental representation of the body, thus, diseases that compromise parts of the body can cause changes in the subject's self-image, which, according to Hannickel, Zago, Barbeira and Sawada (2002) is a central aspect of every person’s self-esteem, therefore the attitudes and emotions before it constructs an essential body concept for an adequate social life. Thus, self-esteem is people's sense of self-image, and how them interprets it (Jesus, Santos, & Brandão, 2015).
According to Erthal (1986) the concept of self-image is not only permeated by the physical aspect, but also includes other variables unique to the process of identity, thus, the image that a person has of itself takes into consideration two aspects: what the person thinks of itself and what it would like to be.
Since all people are bound to their own body in some way, the notion of body is essential for the consolidation of the individual’s identity. However, this notion is being modified throughout life taking into account all the perceptions and experiences of the person, thus occurring a mental reorganization of their body image and the way it is observed by others, since self-image is constructed from the interaction of the subjects in their social context, being a result of established relationships with others and with oneself (Souza, Mata, & Antão, 2013).
Silva, Castro, and Chem (2012) also point out that socio-cultural issues influence the development of dissatisfaction, distortion, depreciation and preoccupation with the body, which causes the individual's emotional experience towards their self-image to be subjective, just as demonstrated by Kakeshita and Almeida (2006), who also claim that the person's satisfaction with their body size or specific body parts is individual and multifactorial.
This aspect, therefore, will determine the satisfaction or not to the alterations of image due to the pathology, thus, implying in the person’s coping possibilities in relation to the permanent changes caused by acromegaly.
The reaction to the altered image will depend on the coping strategies that are developed by the subject, as well as on the origin of the change, the importance of the new image in its future and the types and possibilities of support that it will receive. In this way, the individual's adaptability to the new body image will depend on the flexibility degree of its personality (Price, 1990).
Because of these changes, Schilder (1999) suggests that the person's social context may shift to looking at him or her differently, so depending on the emotional meaning that these transformations have for the individual, can cause, mainly, variations in their patterns of self-acceptance, in their cultural development and in their social relations. Thus, self-esteem is directly influenced by self-image and the development of a negative self-image distortion will lead to self-esteem relegation (Jesus, Santos, & Brandão, 2015).
Body changes are expected in the aging process of the human being without distinction of gender. However, Mori and Coelho (2004) point out the impact of female self-image from the biological maturation process, which imposes physical and psychic changes to the female body.
Beauty is meant for the women as a cultural duty, being her responsibility to reach it, so the more the world of contemporary images are explored, the more it is evident that women feel more than men the effects of this process, once the Brazilian culture exhibits the woman in order to highlight their archetypes of cultural beauty (Marcuzzo, Pich, & Dittrich, 2011). Thus, there is a conflict between the ideal of beauty prescribed by society and the somatotype of most of the population (Heinberg, 1996).
In this sense, several aspects can help in the process of self-image formation, such as gender, age and the media. Silva, Castro and Chem (2012) point out that the sociocultural theories of body image disorders bring a relation of the expectations and experiences of body ideals, as well as the negative influence of the mass media, which reinforce the need to be within the beauty and weight standards.
Added to this aspect, the body alterations caused by acromegaly are interrelated with the psychological suffering of women in relation to the middle age and the aesthetic demands of the socio-cultural context. Psychological symptoms, in turn, can be observed in people with significant losses or changes in the body, such as difficulties in intimate and interpersonal relationships, decreased social relations, isolation and feeling of embarrassment Silva, Castro, and Chem (2012) as it is verified social avoidance behaviors in patients after the diagnosis of acromegaly.
Thus, Price (1990) points that it is common for the subject to deny and neglect his or her altered body image. However, some people can share their feelings with friends and family, developing positive coping strategies.
This research is relevant because it can broaden the view of health professionals in face of acromegaly, going beyond signs and symptoms when realizing the dimension of the psychological and emotional implications that can affect several areas of patients' lives and their way of relate with the world. Another relevant aspect is the fact that there are still few studies related to acromegaly on the pathology effect on self-image. Thus, this study intends to contribute to the broadening of the discussions on the subject, aiming to describe the psychological impacts of acromegaly on self-image.
Method
The present study is described as retrospective cross-sectional, with a qualiquantitative approach.
Participants
Seventy-one patients with acromegaly from the state of Bahia, Brazil, of both genders, aged over 18 years, being treated at the CEDEBA’s (Center of Diabetes and Endocrinology of the State of Bahia, Brazil) neuroendocrinology outpatient clinic, were recruited. The diagnoses of the participants were confirmed by laboratory and imaging exams and posted on medical records of the referral clinic. Patients with inability to answer the questionnaire used in this study were excluded from the sample.
Materials
The AcroQol (Acromegaly Quality of Life Questionnaire) questionnaire was used to measure the quality of life in people with acromegaly. The questionnaires were applied in the waiting rooms of the clinic or during the anamnesis of the psychology service from April 2014 to July 2017.
This instrument was created for use in clinical trials and routine monitoring of patients with such diagnosis, being self-administered and composed of 22 items, which assess physical and psychological aspects and the impact of the disease on social relations (Badia, Webb, Prieto, & Lara, 2004).
Passos (2014) points that each item of AcroQol is answered with a score ranging from 1 to 5, which 1 corresponds to the worst quality of life and 5 to the best quality of life (Likert scale). According to the question, the respondent evaluates their quality of life according to the degree of frequency (always, most of the time, sometimes, rarely, never) or the degree of agreement with the items (completely agree, moderately agree, neither agree nor disagree, moderately disagree and completely disagree).
As a complementary data collection instrument, the group interview was also used, in which the focus group (FG) technique was applied by the psychologist of the researchers team, who has experience in the conduction of groups in the health area. In addition to optimizing the time and avoiding the fatigue of the interviewee, this technique favors the researcher observation about the social interaction of the participants in the discussion of the research theme.
Procedure
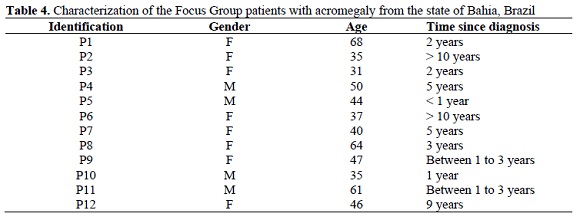
The patients invited to participate in the focus group are part of the psychoeducational group carried out at the Neuroendocrinology Outpatient Clinic of CEDEBA, from March to July 2017. Three sessions of the focus group were performed, with the participation of 12 patients in the total, being important to emphasize that 60% of these patients attended all three meetings.
At all sessions, the objectives of the focus group and the research were explained to the patients, emphasizing the importance of the collaboration through the answers. At the first meeting, a dynamic was performed where the patients saw themselves at the mirror and assessed how satisfied they were when they saw their images in the mirror and how they wanted to have a different body shape, aiming at the reflection about their self-image and relating it to the acromegaly. At the second session, the patients were asked to bring photos that showed their physical changes caused by acromegaly, through the construction of a small poster, which brought the most significant changes to them in the photos. As for the third and last session, an activity was performed to cut and paste pictures of magazines that represented how each patient was seeing himself at that moment of his life, focusing on self-image after the diagnosis of acromegaly.
It is important to emphasize that this research is part of a main project entitled “Rare Diseases: Comprehensive Care, Evaluation and Social Support”, approved by the Ethics and Research Committee of the Bahiana School of Medicine and Public Health (EBMSP) in May 2016, under the number of the CAAE: 56840516.4.0000.5544. All study participants signed the Free and Informed Consent Term (TCLE) according to Brazilian Resolution 466/12 for research involving human subjects.
Data analysis
Seventy-one observations were required to obtain a statistical power of 80% to evaluate the differences in scores between men and women in the AcroQol self-image subscale, with alpha level of 5%.
Descriptive analysis and statistical tests were performed in the Statistical Package for Social Sciences (SPSS v23.0). The results were presented in tables with descriptive measures (mean, maximum, minimum, standard deviation and standard error, suitable for quantitative variables) and frequencies (absolute and relative) for qualitative variables. Normal distribution analysis was performed for the quantitative variables of continuous distribution using the Kolmogorov-Smirnov test. Univariate analysis was performed using the Chi-square test and the Student t-Test for comparison between the gender groups and the self-image subscale scores. The level of significance was set at 5% (p <0.05).
To describe the psychosocial impacts of acromegaly on self-image, a subscale was considered, that is, a partial score resulting from the sum of questions regarding the evaluation of self-image aspects. Thus, although the 22 questions of AcroQol were applied in the sample, for the quantitative analysis of this study 6 items that investigate aspects of self-image were selected: “I feel ugly”, “I look awful in photographs”, “I avoid going out with friends because of my appearance” “I look different in the mirror”, “People stare at me because of my appearance”, and “There are some parts of my body that are too big”. In addition to these, an item of AcroQol was also explored concerning depressive symptoms: “I feel depressed after diagnosis” and may be correlated with those mentioned above.
In order to associate the interference of discomfort with body image and depressive symptoms of acromegalic patients, a correlation was also made between the change in self-concept after diagnosis (feeling "ugly" and feeling "horrible" in photographs) and mood (I feel "depressed after diagnosis").
Of these 7 items, only 2 (“I avoid going out very much with my friends because of my appearance” and “I feel depressed after diagnosis”) were answered on a frequency scale, while the others are answered in a degree of agreement scale for the item.
The data obtained in the focus group were analyzed based on the technique of content analysis, which verifies what was said, seeking to classify this content into categories that will help understand what is behind the respondents' discourse (Silva & Fossa, 2015). Content analysis has gained popularity from Bardin (1977), which emphasizes the importance of accuracy for the use of this technique in order to overcome uncertainties and find out what is being questioned.
There are some steps in the content analysis of the collected data, Bardin (1977) sets them into three phases: 1) pre-analysis, 2) exploration of the material and 3) treatment of results, inference and interpretation. According to this author, in the first phase, a general reading of the data is performed, while for the second one the information is codified, formulating the categories for analysis. Subsequently, it is made a cutout of the material in comparable paragraphs with the same semantic content, thus establishing categories with differentiated themes, transposing the raw data to organized data. After grouping the paragraphs into common categories and in a progressive way, the last phase described by the author enters, in which the data interpretation is performed, thus performing the qualitative analysis of the contents of the transcribed speech.
The participants speech was transcribed using the Microsoft Word® program, where the information categorization, choice of speeches and content analysis were performed. The qualitative analysis of the collected data was included in the study to enable the access to an amplified perception of the patient with acromegaly on his/her self-image.
Results
Quantitative results
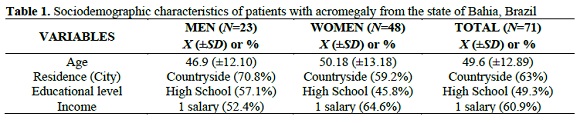
It was noticed that the sample, both men and women, presented a similar sociodemographic profile, as shown in Table 1. Thus, it is important to emphasize that due to the age group (mean age 49.6 years), the participants may already be suffering from impacts on self-image, which may be overlapped in the aging process itself, corroborating with Mori and Coelho (2004). Accordingly, the impact on the self-image provoked by acromegaly constitutes one more factor to be added to the self-perception questions of the subject, modulating its acceptance patterns.
Regarding the family income, also illustrated in Table 1, most of the sample receives up to 1 minimum salary, which implies a probable difficulty in aesthetic procedures access. It can be understood that this is not a confounding variable, since no patient implied perform plastic surgery or any other aesthetic procedure due to acromegaly. In this sense, these patients may have to live with the physical changes caused by the disease, which may impact their self-image and self-esteem.
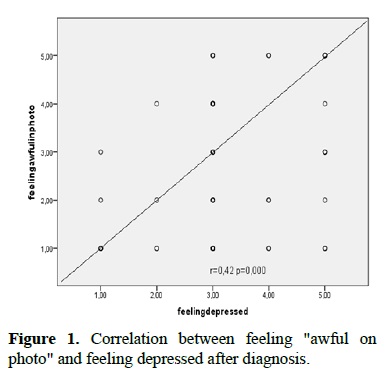
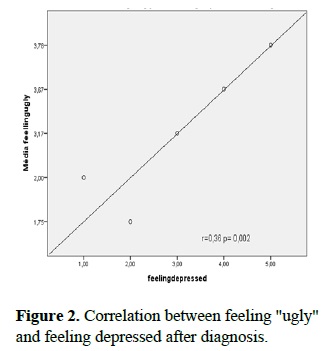
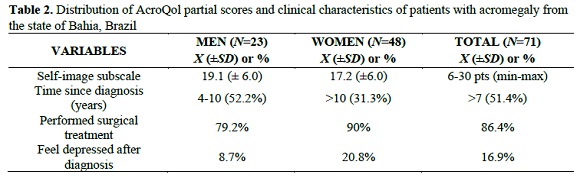
The scores for the self-image subscale (Figures 1 and 2) shows that the participants in this study presented above-average results, regarding the possibility of minimum and maximum scores in AcroQol. This data may have an association with the mean value for the “feeling depressed after diagnosis” variable, which presented a low percentage.
There was also a significant correlation between the change in self-concept after diagnosis (feeling "ugly" or feeling "awful" in photographs) and humor (feeling depressed after diagnosis). The correlations ranged from weak (Figure 2) to moderate (Figura 1), showing that facial changes and discomfort with self-image bring psychosocial impacts to acromegalics.
Although specific inventories have not been used in this study to evaluate depressive symptoms, this data is clinically relevant, not necessarily indicating that the respondents are not in a depressive state, but that they do not associate this psychic state with the diagnosis of acromegaly.
In addition, it was observed that in the global and mean distribution of the partial scores of the inventory there was not much variation between the means of men and women, which did not allow an accurate exploration of the psychosocial impacts, making it necessary to describe the variables that compose this subscale and its repercussions on the respondents.
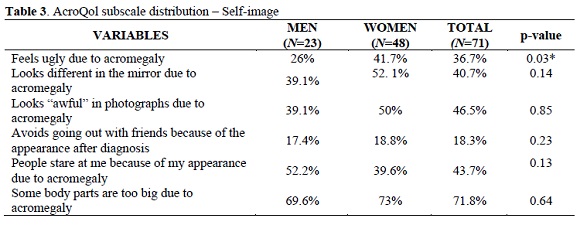
Thus, a categorization of the items of the self-image subscale was performed, which were divided into: self-image perception; satisfaction with self-image; and social repercussions of the physical changes caused by acromegaly.
In the “self-image perception” dimension, the variables involved are “I look different in the mirror because of acromegaly” and “There are some parts of my body that are too big because of acromegaly” (Table 3). Regarding the first statement, the respondents of both genders, for the most part, are totally in agreement, being 39.1% men and 52.1% women. As for the second statement, the majority of female respondents (73%) fully agree that there are parts in their bodies that are bigger due to the development of the disease, as it occurs in the male gender, with a percentage of 69.6%.
Regarding the “satisfaction with self-image” dimension, the variables involved are “I feel ugly due to acromegaly” and “I look awful in photographs because of acromegaly” (Table 3). In the first statement, 47.8% of the male respondents say they are not in agreement with the sentence, while 41.7% of the female patients think otherwise, in complete agreement with the statement. For the second statement, the respondents of the feminine gender follow the same line of thought of the previous question, obtaining 50% of complete agreement with the statement. On the other hand, almost half of the male patients are between “moderately agree” (21.7%) and “disagree” (26.1%), however, it is important to note that another 30.4% of male participants claims to be in full agreement.
The last dimension, “social repercussions of the physical changes caused by acromegaly”, has as its variables the affirmations “I avoid going out with my friends because of my appearance due to acromegaly” and "People stare at me because of my appearance due to acromegaly” (Table 3). Regarding the first statement, male patients (78.3%) said they did not limit their outings with friends because of physical changes, as did most of the female respondents (60.4%). Regarding the second statement, more than half of the men (52.2%) say they are in complete agreement with the statement, however, a relevant percentage (30.4%) of the same gender says they are not in agreement and do not notice the stare of other people at them because of their appearance due to acromegaly. The women, on the other hand, presented divided answers on this statement, since 39.6% are in complete agreement and 35.4% say they are not in agreement with the statement.
From these data, it was possible to notice that men appear to have given more attention to the physical and visible changes in their appearance, such as the perception of bigger parts in their body due to acromegaly, in addition to feeling more stared due to the physical aspect than women. This inference goes against what was stated by Roerink et al. (2015) about women being more concerned with physical appearance than men, especially regarding facial changes.
As for the women, they seem to take a greater impact on their self-esteem than men, since much of the sample of this gender feels ugly after diagnosis and looking awful in the mirror, echoing the self-acceptance patterns demonstrated by Marcuzzo, Pich, and Dittrich (2012) since beauty is meant for the woman as a cultural duty, and it is her responsibility to achieve it, reverberating on her self-image, self-esteem, and self-concept.
It is also evidenced that both men and women do not limit their go outs with friends due to their physical appearance after the diagnosis of acromegaly, which suggests that the social life of the respondents seems to have been little impacted.
Qualitative results
The sample of the focus group consisted of 12 patients with acromegaly from the Neuroendocrinology outpatient clinic of CEDEBA, mostly females and with varying age and diagnostic time, as shown in Table 4. It is important to mention that the patient’s names were altered by identification numbers, in this way, the data were kept confidential and only the researchers had access to full information.
The qualitative results obtained during the group sessions were transcribed and separated into 3 categories: coping strategies; perception of the person about physical changes; and psychosocial aspects. The results will be illustrated with transcripts of participants' speeches, which had their identities preserved.
Coping Strategies
According to Folkman (2012) coping can be defined as behavioral and cognitive strategies that a person adopts to deal with adverse situations, which are, after the diagnosis of acromegaly the individual makes an effort to act in the situation that originated the stress and to live with the existing pathology, and so developing new abilities of self-care.
It was noticed that some patients revealed to use psychological resources to deal with the changes caused by acromegaly, within this category, some of the patients’ speeches called attention, such as:
“They call me ugly, but I do not care because I got Jesus in my heart” (P2).
“Why should I be ashamed of my appearance? Shame is stealing. I must face the reality of life. That’s my appearance now” (P4).
It is noticed through such statements that patients use spirituality and resilience as strategies for coping with the disease and related social issues. In addition, it may be highlighted that many of the participants reported that the exchange of experiences with other patients, made possible through the group, was a strengthening factor in relation to manage the disease.
Perception of the individual about the physical changes
The physical changes are characteristic of acromegaly, being perceived by patients as the most common symptom and being reported in the literature as the factor that bothers them the most. The subject, when noticing the disfiguring physical changes provoked by the pathology, confronts it with their self-image prior to diagnosis.
Therefore, it is noticed that in this sample, during the focus group sessions, patients with the most recent diagnosis seem to be paralyzed and fixated on the immediate effect of the acromegaly body changes signs. Only after a certain time, patients feel capable of reconstructing their identity and self-concept, as can be seen from the following statements:
“I had to change the size of my wedding ring” (P7).
“The change in my face was the one that bothered me the most” (P5).
“My nose was thin, beautiful. Beautiful smile, small teeth” (P5).
“Before I was perfect and full of disposition” (P11).
It is worth mentioning that patient P5 has a recent diagnosis, less than 1 year (Table 4), and is in the phase of finding the symptoms, seeking adaptation and reconstruction of his/her self-concept, to later develop coping strategies.
Psychosocial aspects (psychological aspects, discrimination)
Because it is a rare disease, acromegaly is not popularly known and its repercussions go beyond body changes, such as joint pains. However, these symptoms are not visible and can therefore be devalued by the social circle of these individuals, such as family and employers.
On the other hand, according to what was raised in the focus group, the physical changes are soon noticed by the patients' social circle, generating comments and discrimination situations. These issues impact on the social, professional and personal lives of patients, as illustrated below:
“They asked me: Is that you? You were so beautiful, are you sick?” (P8).
“When I get upstate, they call me ugly” (P9).
“I loved my body (…) now I am like this and I see a lot of prejudice” (P2).
“You will go down into the sea and you will not rise anymore” (P4 - Occupation: former fisherman. Sentence said to the patient by his colleagues because of his feet size).
“I’ve got a little depressed and didn’t feel like going out until I had the surgery” (P8).
“Acromegaly is a burden” (P3).
Another important data to be discussed is the report of one of the patients, during the application of AcroQol, from her resignation to the physical changes and clinical complications of acromegaly. She told that she needed to wear high-heels, but could not because of the growth of her feet and joint pain. She also reported the appearance of dark spots on her skin (hyperpigmentation) and excessive sweating, which were related in her work environment to poor hygiene. In addition to these situations, the patient also needed to absent herself from work once a month for application of injectable medication. Thus, there have been considerable impairments in the quality of life of the patient and in her social and work relations due to the disease symptoms.
Discussion
From all that was exposed throughout this study, it was perceived that acromegaly can go beyond physical symptoms, such as pain, facial, acral and cutaneous changes, affecting the patients' quality of life, the way in which they perceive their body, in its beliefs, in its strategies to cope with the limitations caused by pathology, as well as the series of impacts that the alteration in the self-image can bring to social, psychological and emotional levels in the life of the individual.
Therefore, it is considered important to determine an interdisciplinary approach in treatment, since acromegaly causes significant psychological impacts on the perception of self-image and other health aspects. This approach should include family and community support, thus, strengthening the social support of patients.
It was noticed that the facial characteristics obtained greater importance in relation to the self-image, these data emphasize the importance of approaching an interdisciplinary care, in order to support the subject in this aspect during the process and treatment. The team can, whenever possible, propose interventions to avoid the evolution of great psychic impairments and enable the creation of coping strategies. It is important to emphasize that the team should not ignore the impact of self-image in patients with acromegaly.
Furthermore, it stands out the importance of psychological counseling not only individual but also group care, since patients can exchange experiences about getting sick, understand more about the pathology and re-signify the new facial and body identity imposed by the clinical condition.
In time, it is known that subjective or self-reported questionnaires may not be sensitive to more subtle psychiatric disorders, so a limitation of this study is due to the fact that specific inventories have not been used to evaluate depression and anxiety symptoms, using only to the AcroQol self-report scale to evaluate these items in the sample.
REFERENCES
Abreu, A., Tovar, A., Castellanos, R., Valenzuela, A., Giraldo, C., Pinedo, A., ... Bronstein, M. (2016). Challenges in the diagnosis and management of acromegaly: a focus on comorbidities. Pituitary, 19, 448-457. DOI: 10.1007/s11102-016-0725-2. [ Links ]
Adelman, D., Liebert, K., Nachtigall, L., Lamerson, M., & Bakker, B. (2013). Acromegaly: The disease, its impact on patients, and managing the burden of long-term treatment. International Journal General Medicine, 6, 31-38. DOI: 10.2147/IJGM.S38594. [ Links ]
Badia, X., Webb, S., Prieto, L., & Lara, N. (2004). Acromegaly quality of life questionnaire (AcroQoL). Health and Quality of Life Outcomes, 2(13), 1-6. DOI: 10.1186/1477-7525-2-13. [ Links ]
Bardin, L. (1977). Análise de conteúdo. Lisboa: Edições 70. [ Links ]
Boguszewski, C. & Ayuk, J. (2016). Acromegaly and cancer: An old debate revisited. European Journal of Endocrinology, 175(4), 147-156. DOI: 10.1530/EJE-16-0178. [ Links ]
Brasil, Ministério da Saúde. (2013). Portaria nº 199, de 25 de fevereiro de 2013. Aprova o Protocolo Clínico e Diretrizes Terapêuticas da Acromegalia. Diário Oficial da União, Brasília. [ Links ]
Erthal, T.(1986). A autoimagem: possibilidade e limitações da mudança. Arquivos Brasileiros de Psicologia, 38(1), 39-46. [ Links ]
Fava, G., Sonino, N., & Morphy, M. (1993). Psychosomatic view of endocrine disorders. Psychother Psychosom, 59(1), 20-33. DOI: 10.1159/000288641. [ Links ]
Folkman, S. (2012). Stress, Health, and Coping: Synthesis, Commentary, and Future Directions. The Oxford Handbook of Stress, Health, and Coping, 1-16. DOI: 10.1093/oxfordhb/9780195375343.013.0022.
Hannickel, S., Zago, M., Barbeira, C., & Sawada, N.(2002). O comportamento dos laringectomizados frente à imagem corporal. Revista Brasileira de Cancerologia, 48(3),333-339. [ Links ]
Heinberg, L. (1996). Theories of body image disturbance: perceptual, developmental and sociocultural factor. In: J. K. Thompson (Ed.), Body image, eating disorders, and obesity: an integrative guide for assessment and treatment (pp. 27-48).Washington, USA: American Psychological Association. [ Links ]
Holdaway, I. & Rajasoorya, C. (1999). Epidemiology of acromegaly. Pituitary, 2(1), 29-41.DOI: 10.1023/a:1009965803750. [ Links ]
Jesus, P., Santos, I., & Brandão, E.(2015). A autoimagem e a autoestima das pessoas com transtornos de pele: Uma revisão integrativa da literatura baseada no modelo de Callista Roy. Aquichan, 15(1), 75-89. DOI: 10.5294/aqui.2015.15.1.8. [ Links ]
Kakeshita, I. & Almeida, S. (2006). Relação entre índice de massa corporal e a percepção da autoimagem em universitários. Revista de Saúde Pública, 40(3), 497-504. DOI: 10.1590/S0034-89102006000300019. [ Links ]
Katznelson, L., Laws, E., Melmed S., Molitch, M., Murad, M., Utz, A., & Wass, J.(2014). Acromegaly: an endocrine society clinical practice guideline. The Journal of Clinical Endocrinology & Metabolism, 99(11), 3933-3951. DOI: 10.1210/jc.2014-2700. [ Links ]
Lavrentaki, A., Paluzzi, A., Wass, J., & Karavitaki, N. (2017). Epidemiology of acromegaly: review of population studies. Pituitary, 20(1), 4-9. DOI: 10.1007/s11102-016-0754-x. [ Links ]
Marcuzzo, M., Pich, S., & Dittrich, M. (2012).A construção da imagem corporal de obesos e a sua relação com os imperativos contemporâneos de embelezamento corporal. Interface, 16(43), 943-956. DOI: 10.1590/S1414-32832012005000041. [ Links ]
Matta, M., Couture, E., Cazals, L., Vezzosi, D., Bennet, A., & Caron, P. (2008). Impaired quality of life of patients with acromegaly: Control of GH/IGF-I excess improves psychological subscale appearance. European Journal of Endocrinology. 158, 305-310. DOI: 10.1530/EJE-07-0697. [ Links ]
Melmed, S. (2006). Acromegaly. New England Journal of Medicine, 355(24) 2558-2573. DOI: 10.1056/NEJMra062453. [ Links ]
Melmed, S., Casanueva, F., Klibanski, A., Bronstein, M., Chanson, P., Lamberts, S. W.,…Giustina, A. (2013) A consensus on the diagnosis and treatment of acromegaly complications. Pituitary, 16, 294-302. DOI: 10.1007/s11102-012-0420-x. [ Links ]
Melmed, S. & Kleinberg, D. (2003). Anterior pituitary. In P. Larsen, H. Kronemberg, S. Melmed, & K. Polonsky, Williams textbook of endocrinology (pp.177-280). Philadelphia: Saunders Elsevier. [ Links ]
Molitch, M. (1992). Clinical manifestations of acromegaly. Endocrinology and metabolism clinics of North America, 21(3) 597-614. [ Links ]
Mori, M. & Coelho, V. (2004). Mulheres de corpo e alma: aspectos biopsicossociais da meia-idade feminina. Psicologia Reflexão e Crítica, 17(2), 177-187. DOI: 10.1590/S0102-79722004000200006. [ Links ]
Nabarro, J. (1987). Acromegaly. Clinical Endocrinology, 26(4), 481-512. [ Links ]
Naves, L., Mercado, M., Duarte, F., Vilar, B., & Vilar, L. (2016). Acromegaly - an overview. In L. Vilar (Ed.) Endocrinologia Clinica (Clinical endocrinology) (pp. 56-70). Rio de Janeiro: Guanabara Koogan. [ Links ]
Passos, K.(2014). Avaliação do perfil psicopatológico e da qualidade de vida em pacientes acromegálicos (Dissertação de Mestrado), Universidade de Brasília, Brasília. [ Links ]
Price, B. (1990). Body Image: Nursing concepts and care. Great Britain: Prentice Hall. [ Links ]
Reid, T., Post, K., Bruce, J., Kanibir, M. N., Reyes-Vidal, C., & Freda, P. (2010). Features at diagnosis of 324 patients with acromegaly did not change from 1981 to 2006: acromegaly remains under-recognized and under-diagnosed. Clinical Endocrinology, 72(2), 203-208. [ Links ]
Roerink, S., Wagenmakers,M., Wessels J., Sterenborg, R., Smit, J., Hermus, A., & Netea-Maier, R. (2015). Persistent self-consciousness about facial appearance, measured with the Derriford appearance scale 59, in patients after long-term biochemical remission of acromegaly. Pituitary, 18(3), 366-375. DOI: 10.1007/s11102-014-0583-8. [ Links ]
Schilder, P. (1999). A imagem do corpo: as energias construtivas da psique. São Paulo: Paulo Martins. [ Links ]
Silva, A. & Fossá, M. (2015). Análise de conteúdo: exemplo de aplicação da técnica para análise de dados qualitativos. Qualitas Revista Eletrônica, 16(1), 1-14. DOI: 10.18391/qualitas.v16i1.2113. [ Links ]
Silva, M., Castro, E.,& Chem, C. (2012). Qualidade de vida e autoimagem de pacientes com câncer de cabeça e pescoço. Universitas Psychologica, 11(1), 13-23. [ Links ]
Souza, M., Mata, M.,& Antão, C. (2013). Adolescentes: Percepção da autoimagem. Primeira Jornada de Enfermagem da Escola Superior de Saúde do Instituto Politécnico de Bragança, 49 - 58. [ Links ]
Varadhan, L., Reulen, R., Brown, M., & Clayton, R. (2016). The role of cumulative growth hormone exposure in determining mortality and morbidity in acromegaly: a single centre study. Pituitary, 19(3), 251-261. DOI: 10.1007/s11102-015-0700-3. [ Links ]
Vilar, L., Vilar, C., Lyra, R., Lyra, R., Naves, L. (2017). Acromegaly: clinical features at diagnosis, Pituitary, 20(1), 22-32. DOI: 10.1007/s11102-016-0772-8. [ Links ]
Webb, S. (2006). Quality of Life in Acromegaly. Neuroendocrinology, 83, 224-229. DOI: 10.1159/000095532. [ Links ]
Yedinak, C., & Fleseriu, M. (2014). Self-perception of cognitive function among patients with active acromegaly, controlled acromegaly, and non-functional pituitary adenoma: a pilot study. Endocrine, 46(3), 585-593. DOI: 10.1007/s12020-013-0106-9. [ Links ]
Zanini, M., Oshiro, R., Paschoal, L., Paschoal, F., & Timoner, F. (2004). Aspectos dermatológicos da acromegalia. Anais Brasileiros de Dermatologia, 79(4), 491-494. DOI: 10.1590/s0365-05962004000400010. [ Links ]
Endereço para correspondência | Dirección para correspondencia | Correspondence
Rua Almirante Ernesto de Melo Jr., 106, Pituba, SalvadorBA, Brazil. CEP 41.810-750. Tel.: +55 (71) 99967-1300. Email: michelleqv@gmail.com.
Recebido em 28 de Fevereiro de 2018/ Aceite em 07 de Maio de 2020