Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Psicologia, Saúde & Doenças
versão impressa ISSN 1645-0086
Psic., Saúde & Doenças vol.15 no.3 Lisboa dez. 2014
https://doi.org/10.15309/14psd150312
Psychological status, eating behaviour, quality of life of portuguese obesity surgery candidates
Estado psicológico, alimentação, qualidade de vida de candidatos a cirurgia da obesidade
Isabel Silva 1, José Pais-Ribeiro 2, & Helena Cardoso3,4
1Human and Social Sciences Faculty, Universidade Fernando Pessoa, Porto, Portugal;
2Psychology and Educational Sciences Faculty, Porto University, Porto, Portugal;
3 Santo António Hospital – Porto Hospital Centre, Porto, Portugal;
4 ICBAS/UMIB, Porto University, Porto, Portugal
Endereço para Correspondência
ABSTRACT
The present study aimed to describe psychological status, and eating behaviour characteristics, as well as quality of life of obesity surgery candidates in a public Portuguese hospital. A cohort of 198 obesity surgery candidates, with a body mass index ranging between 35.47 and 80.65 (M=48.76; SD=8.40) was studied. Patients answered to a semi-structured interview, to Hospital Anxiety and Depression Scale, Self-Concept Clinical Inventory, and to MOS SF-36. Results show that a high percentage of patients present yo-yo phenomenon and report important consequences in psychological, social, familial, work, spare time and motor domains. Binge eating disorder, sweet/fat compulsion, continuous nibbling, eating rapidly, eating without feeling hungry, eating until feeling indisposed, the perception of not having control over what is eaten and feeling upset after eating an excessive amount of food are relatively frequent behaviours. Patients commonly present anxiety disorders and major depression (including suicidal ideation and suicidal attempts), diminished self-concept and poor quality of life.The present study shows that obesity is significantly associated to impaired psychological functioning in obesity surgery candidates, suggesting that it is crucial to consider this association in pre surgical psychological assessment and intervention in order to contribute to more positive surgery outcomes.
Key- words – Obesity, anxiety, depression, self-concept, eating behaviour, quality of life
RESUMO
O presente estudo teve como objetivos descrever o estado psicológico e as características do comportamento alimentar, bem como a qualidade de vida de candidates a cirurgia de obesidade num hospital público português. Foram estudados 198 candidatos a cirurgia de obesidade, com um índice de massa corporal compreendido entre 35,47 e 80,65 (M=48,76; DP=8,40). Os doentes responderam a uma entrevista semiestruturada, à Hospital Anxiety and Depression Scale, ao Inventário Clínico de Autoconceito, e ao MOS SF-36. Os resultados revelam existir uma elevada percentagem de doentes com fenómeno yo-yo e mostram que a obesidade tem consequências nos domínios psicológico, social, familiar, no emprego, tempos livres e a nível motor. A perturbação de ingestão compulsiva, compulsão por doces/gordura, petisco continuo, ingestão rápida, comer sem sentir fome, comer até se sentir indisposto, a perceção de não se ter controlo sobre o que se está a comer e o sentir-se perturbado por comer uma quantidade excessiva de comida são relativamente comuns. Os doentes frequentemente apresentam perturbações de ansiedade e depressão major (incluindo ideação suicida e tentativas de suicídio), baixo autoconceito e uma qualidade de vida pobre.O presente estudo revela que a obesidade está associada com problemas ao nível do funcionamento psicológico nos candidatos a cirurgia bariátrica, sugerindo que é importante considerar esta associação na avaliação e intervenção psicológica pré cirurgia de obesidade de forma a contribuir para resultados do tratamento cirúrgico mais positivos
Palavras-chave - Obesidade, ansiedade, depressão, auto-conceito, comportamento alimentar, qualidade de vida
The prevalence of obesity is increasing worldwide (Kaukua, 2004) and Portugal is not an exception concerning this problem (Carmo, et al., 2007), reason why one of the objectives of the Portuguese National Health Plan for 2012-2016 is precisely to diminish the percentage of overweight individuals in the population (Ministério da Saúde, 2012). Obesity constitutes a major public health problem, being associated to a greater non-communicable diseases risk and to mortality risk (World Health Organization, 2014), but also to impaired quality of life and to poor physical and mental well-being (Abilés, et al., 2010).
Patients and health professionals have been trying to improve the outcomes of non-surgical and surgical treatments for obesity, pursuing a significant and durable weight loss. Clinical experience and literature show that obesity surgery outcomes largely depend on patients ability to adapt their lifestyle to post-surgical self-care and they also suggest that, when patients report difficulty in implementing lifestyle changes, obesity surgery can be detrimental and can lead to negative results (Bauchowitz, et al., 2005) (as weight regaining, malnutrition, clinical depression, dissatisfaction with the health care system, dissatisfaction with surgery outcomes, poor quality of life and poor mental and physical well-being).
Research reveals that depression (current and lifetime) (Legenbauer, Petrak, Zeaan, & Herpetz, 2011) and food addiction (Burmeister, Hinman, Koball, Hoffmann, & Carels, 2013) predict less weight loss. It is possible that poor eating habits continue after surgery (Orth, Madan, Taddeucci, Coday, & Tichansky, 2008), and very often patients forget certain preoperatively known facts (Madam & Tichansky, 2005), what seems to justify the investment in a more sustainable educational intervention. Furthermore, pre and post operative psychological treatment revealed to improve patients compliance and success in obesity surgery, by treating psychopathology and/or helping patients adjustment to dietary and exercise requirement (Friedman, Applegate, & Grant, 2007; Pessina, Andreoli, & Vassalo, 2001; Van Hout et al., 2003). So, we can conjecture that psychological balance and the adoption of healthier eating habits previously to surgery can contribute to better obesity surgery outcomes. The association between psychological health and the success of obesity surgery reinforces the importance of psychological assessment of obesity surgery candidates (Sauerland, et al., 2005), as well as of post-surgical monitoring of patients in order to identify those who would benefit from additional therapy in order to improve weight-loss outcome (Legenbauer, et al., 2011).
In order to implement efficient psychological interventions with candidates to obesity surgery, it is important to characterize this population psychologically and to analyse if there are differences between genders and age groups that justify the conception of differentiated pre-surgical intervention programmes. Thus, the present study intends to describe psychological status, and eating behaviour characteristics, as well as quality of life of patients who are waiting to be submitted to obesity surgery in a public Portuguese hospital. Moreover, it also intends to analyse if there are significantly statistical differences between distinct age groups and gender concerning the variables targeted in this study.
METHODS
Participants
It was studied a cohort of 198 candidates to obesity surgery, 84.8% females (n=168), aged between 15 and 65 years old (M=38.86; SD=11.47), with a school-level ranging between zero and 22 years (M=7.34; SD=4.34), with a BMI ranging between 35.47 and 80.65 (M=48.76; SD=8.40). All the patients were accompanied by the interdisciplinary health care team. When entering the programme to prepare obesity surgery, patients presented a BMI >40 or BMI>35 with specific morbidity associated. Nonetheless, in this programme all the patients are stimulated to lose weight before surgery, in order to diminish surgical risk. Moreover, all the patients have made previous attempts to lose weight under medical supervision, condition necessary to be accepted to obesity surgery programme.
Material
In order to perform psychological evaluation, we use a semi-structured clinical interview and a set of psychological instruments: Hospital Anxiety and Depression Scale (HADS), Self-Concept Clinical Inventory (ICAC), and MOS SF-36.
The semi-structured clinical interview developed for the present study assesses the following domains: socio-demographic characteristics (gender, age, school-level, marital status, and work status), history of previous attempts to lose weight (previous treatments, yo-yo phenomenon, and obesity repercussions in patient life), eating behaviour characteristics and eating disorders and presence of compensatory behaviours, psychiatric history.
HADS: This questionnaire consists of two subscales, one measuring anxiety (with seven items) and one measuring depression (with seven items), which are scored separately. Each item was answered by the patient on a 4-point (0 – 3) response category, so the possible scores ranged from 0 to 21 for anxiety and 0 to 21 for depression. The HADS manual indicates the following cut-off points for anxiety and depression levels: score between 0 and 7 is normal, between 8 and 10 mild, between 11 and 14 moderate and between 15 and 21 severe. Furthermore, HADS proved to present good psychometric qualities (Pais-Ribeiro, et al., 2007).
ICAC: This questionnaire, specifically conceived for Portuguese population, intends to assess global self-concept (20 items), but it also assesses 4 specific subscales – social acceptance/rejection, self-efficacy, psychological maturity and impulsivity-activity. Each item was answered on a 5-point (1 – 5) response category. Higher scores correspond to better self-concept. ICAC proved to present reasonable psychometric qualities, namely reasonable validity and reliability (Serra, 1986). The ICAC normative values for general population, considering gender and age differences, presented by the author were considered to classified patients self-concept in the present study.
MOS SF-36: SF-36 is a general health status measure that contains 36 items, which assess eight subscales (The Medical Outcomes Study, 1993) - physical functioning, role-physical, bodily pain, general health perception, vitality, social functioning, role-emotional, and mental health –, which are organized in 2 domains – physical domain and mental domain. Each of the subscales is scored from zero to 100, with a high score being associated with a high level of quality of life in that domain. SF-36 Portuguese version proved to present good psychometric qualities. Normative values for Portuguese population presented by Ribeiro (2005) were considered to analyse quality of life of the participants in the present study.
Procedure
The Ethical Committee of the institution approved all procedures of this study. It was studied a convenience group of participants who presented all selection criteria: to be candidate to obesity surgery, to be accompanied by the interdisciplinary obesity surgery team and to accept to participate in the study giving their informed consent. Patients were invited to participate in the present study when they went to the hospital to routine psychological consultation. Patients answered to the questionnaires in the context of a personal interview, after their informed consent.
For data analysis, the following statistical procedures were performed: descriptive analysis (frequency, mean, standard-deviation) was used to evaluate characteristics of the study participants; it was also used t Student test; Qui-Square test; Pearson correlation; and One-Way Anova.
RESULTS
Concerning the history of previous attempts to lose weight, results show that the generality of patients made prior efforts to lose weight - using diet (95.4%), physical exercise programs (55.1%) and/or medication (which intended to indirectly regulate appetite, like oral medication to regulate insulin levels and anti-depressive medication to regulate humour) (83.7%) - before becoming candidates to obesity surgery. These efforts were, in the majority of the cases, done under health professionals supervision, namely under primary care doctors and nutritionists supervision in health centres.
Male and female patients do not significantly differ concerning methods previously adopted to lose weight in what concerns to diet (p>.05) and medication (p>.05). However, in what concerns to physical exercise, X2(1,196)=4.76; p<.05, men revealed to have adopted it more frequently to lose weight than women (73.3% and 51.8%, respectively).
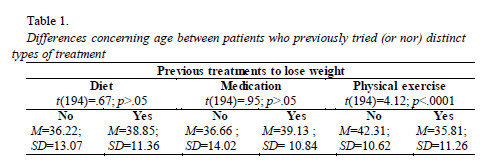
There are no significant differences concerning age between patients who previously attempt to lose weight through diet, and medication, and those who did not tried to lose weight adopting these methods. Nevertheless, patients who previously tried to lose weigh through physical exercise revealed to be younger than those who never tried this treatment method (Table 1).
A higher percentage of patients also have confronted themselves with the failure of these attempts, what can be confirmed by the percentage of patients reporting yo-yo phenomenon – 78.1% (n=150). Patients who do not report yo-yo phenomenon justify the absence of this phenomenon saying that they never were capable of losing excess of weight (21.9%, n=42). Patients reporting yo-yo phenomenon do not differ concerning age, t(190)=.09; p>.05, neither concerning gender, ?2(1,192)=.19; p>.05, from those who do not report this phenomenon.
With respect to obesity negative repercussions in patients lives, patients identified several domains that they feel as being affected by obesity (Table 2). The domains more frequently identified are psychological and motor domains, as well as the abandonment of activities that were pleasant to them (e.g. go to the beach or swimming-pool, to play with their children). Women report more frequently that obesity has negative repercussion in their lives than men in the following domains: psychological, social, spare time activities, and abandonment of pleasant activities. But there are no significant differences between genders concerning familial, work, and motor repercussions (Table 2).
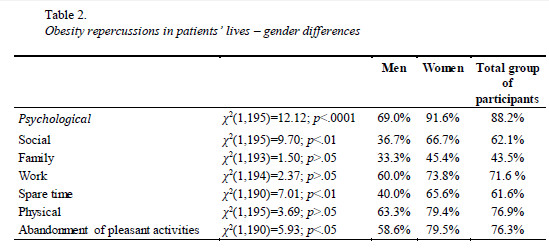
There are no significant differences (p>.05) concerning age between patients who have the perception that obesity has negative repercussions in their lives in the following domains: psychological, social, family, work, spare time, and pleasant activities abandonment. Nevertheless, patients who identify motor repercussions tend to be older, t(193)=2.08; p<.05, than those who do not feel that this is a negative consequence of obesity in their lives (M=39.67; SD=11.34 and M=35.67; SD=11.38, respectively).
Results show that binge eating, sweet and/or fat compulsion, eating rapidly, feeling that they are not able to control the ingestion of food and feeling guilty and disturbed because of this are relatively frequent behaviours in this group of participants. Compensatory behaviours (vomiting, fasting, excessive physical exercise and laxative/diuretic use) are not behaviours commonly adopted by the patients who were studied. Concerning gender, there are no significant differences between the two groups regarding the perception of eating an excessive amount of food, losing control over what is eaten, to eat rapidly, to eat until feeling indisposed, to eat not feeling hungry, to eat alone because they feel ashamed, and regarding compensatory behaviours – vomiting, laxative/diuretic substances use, fasting, excessive physical exercise. Nonetheless, women more frequently report feeling upset after eating an excessive amount of food than men (Table 3).
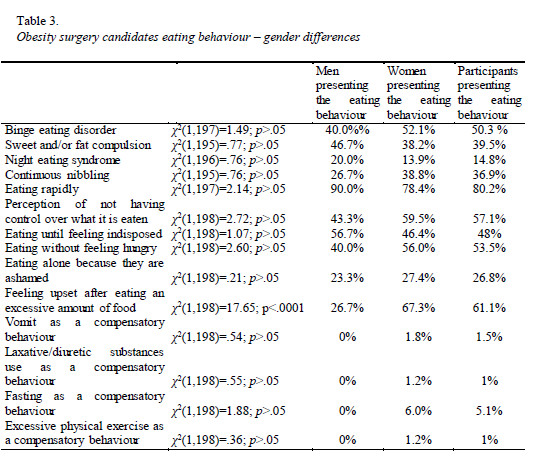
Patients who report eating an excessive amount of food are significantly younger (M=36.84; SD=10.28) than those who do not report this behaviour (M=41.78; SD=12.52), t(193)=2.90; p<.01 But, patients reporting to lose control over what they eat, to eat rapidly, to eat until feeling indisposed, to eat when they do not feel hungry, to eat alone because they feel ashamed, to feel upset after eating an excessive amount of food, to use vomit, laxative/diuretic substances, fasting, and excessive physical exercise, as compensatory behaviours do not significantly differ concerning age from those who do not report these behaviours (p>.05).
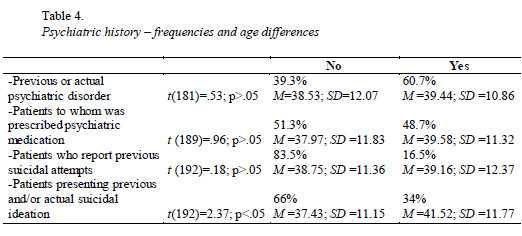
With reference to mental health, results show that the majority of patients studied report actual or previous psychiatric disorder (lifetime prevalence). A considerable percentage of patients revealed to be receiving or to have received previously support in psychology, psychiatry and/or neurology consultations, and to have been prescribed psychiatric medication by psychiatrists or general practice physicians. Some of the candidates to obesity surgery report previous or actual suicidal ideation and previous suicidal attempts. There are no significant differences concerning age between patients presenting previous or actual psychiatric disorders, patients to whom was prescribed psychiatric medication, and patients who report previous suicidal attempts and those who do not present these problems. Nevertheless, patients presenting previous and/or actual suicidal ideation reveal to be older than those without this ideation (Table 4).
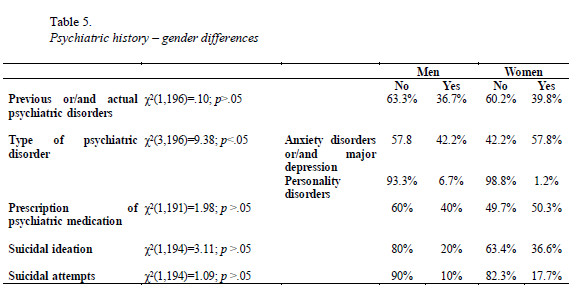
Results show that there are no significant differences between men and women regarding the presence of previous or/and actual psychiatric disorders, however there are significant differences concerning the type of disorder presented. Women present more frequently anxiety disorders and/or major depression, while men present more frequently personality disorders. Both genders do no significantly differ concerning prescription of psychiatric medication, suicidal ideation and suicidal attempts (Table 5).
Age revealed not to be significantly related to anxiety level, r(198)=.03; p>.05, nor to depression level, r(198)=.03; p>.05. When the cut-off points for anxiety, F=.74; p>.05, and for depression, F=.21; p>.05 are considered, results also show that there are no significant differences concerning age between patients classified according the distinct depression symptoms severity.
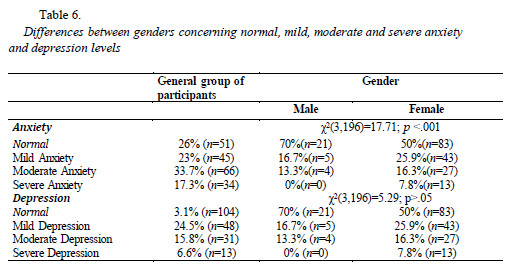
Data analysis shows that there are no significant differences concerning depression between genders (p>.05). However, when considered the cut-off points for anxiety, results suggest the existence of significant differences between women and men. Women present more frequently mild, moderate and severe anxiety levels than men. Contrarily, men more frequently report normal anxiety levels (Table 6).
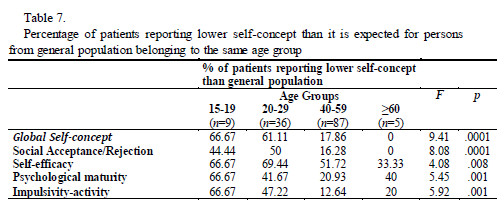
Data analysis revealed that self-concept in obesity surgery candidates is diminished, when we consider the values presented by the general population adjusted to the distinct age groups. Globally, we can observe that the younger groups (15-19 years old and 20-29 years old) report significantly lower global self-concept as well as lower self-concept concerning the specific domains assessed- social acceptance/rejection, self-efficacy, psychological maturity and impulsivity-activity. Additionally, self-efficacy showed to be one of the self-concept domains to which the health care team shall be attentive independently of the age of the patient (Table 7).
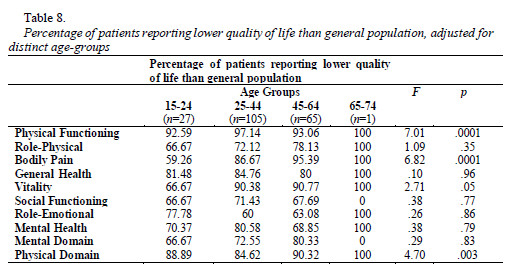
Results suggest that there are no significantly differences between genders concerning global self-concept, social acceptance/rejection, self-efficacy, psychological maturity, neither concerning impulsivity-activity (p>.05). We also analysed quality of life data and concluded that mental and physical domains are both presenting poorer results compared to general population (adjusted for distinct age-groups), namely concerning physical functioning, role-physical, bodily pain, general health, vitality, social functioning, role-emotional and mental health. Moreover, younger patients (15-24 years old) report better quality of life in physical functioning, bodily pain and vitality than older patients (Table 8).
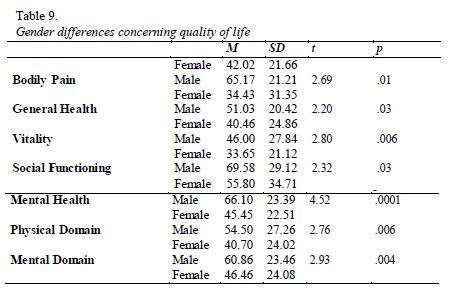
Data analysis suggests the existence of significant differences between genders concerning quality of life. Patients of both genders report poor quality of life in physical and mental domains globally considered, being the physical domain the one in which quality of life is lower. Women also present lower quality of life than men in the following dimensions: bodily pain, general health, vitality, social functioning and mental health (Table 9).
Finally, data analysis revealed that there is no statistically significant correlation between patients BMI and anxiety, depression, self-concept (even when specific domains are considered), and the majority of quality of life dimensions (p>.05). Nevertheless, we verified that the higher BMI is, the worst quality of life concerning physical functioning, r(186)=-.31; p<.0001, and pain, r(187)=-.24; p<.01, is reported.
When we considered separately patients with a BMI between 35 and 39.9 (obesity grade II) with co-morbidity, and patients with a BMI =40 (obesity grade III), we did not find statistically significant differences concerning anxiety, depression, self-concept and quality of life (p>.05).
DISCUSSION
Literature show us that pre and post operative psychological treatment implemented in order to treat psychopathology and to help patients adjustment to a healthy life style proved to contribute to higher patients compliance, as well as to higher success after bariatric surgery (Madam & Tichansky, 2005; Pessina, Andreoli, & Vassalo, C., 2001; van Hout, et al., 2003).
In the present study we intended to characterize psychologically candidates to obesity surgery and to analyse if age and gender differences validate the need to conceive differentiated pre-surgical intervention programmes.
Results from the present study allowed us to draw a psychological portrait of candidates to obesity surgery in a Portuguese public hospital. The first significant characteristic showed to be the route of failure covered by these patients – the majority of them have made prior and ineffective efforts to lose weight, mainly attempts using diet and medication, but also with physical exercise. This failure is confirmed by the high percentage of patients of both genders reporting yo-yo phenomenon. Moreover, we can conclude that it is important to sensitise female and older patients to the importance of adopting a healthy life style before and after surgery concerning physical exercise, as these are the groups who less frequently tried to lose weight adopting this type of weight lost treatment. This seems to be an essential field to be targeted by psychological intervention as physical exercise adherence showed to be a significant behavioural predictor of weight loss (Welch, Wesolowski, Piepul, Romanelli, & Garb, 2008).
Another issue that is essential to have in mind is that obesity does not simply have a significant negative impact in patients physical health, but also in the subjective domain – the majority of the candidates to obesity surgery report important consequences in psychological, social, familial, work, spare time and motor domains of their lives and they affirm that they are giving up of doing what they love to do because of their weight. These negative obesity consequences showed to globally affect the generality of candidates, but particularly women, who seemed to be more affected in psychological, social and spare time domains, and older patients, who more frequently report motor difficulties.
Eating behaviour of obesity surgery candidates also deserves special attention in pre surgical psychological intervention programmes conception. Binge eating disorder, sweet/fat compulsion, and continuous nibbling should be addressed in these programmes, as well as behaviours as eating rapidly, eating without feeling hungry, eating until feeling indisposed, the perception of not having control over what it is eaten and feeling upset after eating an excessive amount of food. These eating behaviours can have important consequences in weight gaining and mood disorders before obesity surgery, but they also can have significant implications in surgery outcomes, namely in the development of post-surgical eating avoidance disorder. Research shows that many patients who binge ate prior to surgery report continued feelings of loss of control when eating small amounts of food after bariatric surgery and present poorer surgical outcomes (Niego, Kofman, Weiss, & Geliebter, 2007). Clinical experience also shows that Portuguese patients with obesity diagnosis, even after losing a significant percentage of excess of weight, feel guilty when they eat and that they assess the amount of food eaten as excessive even when objectively it is not. It is possible that the differences between genders and age groups do not justify the construction of differentiated intervention programmes concerning eating behaviour, and that eating behaviour can be addressed equally for the two genres.
The present study also suggests that it is important to value mental health in pre-surgical psychological assessment and intervention – binge eating disorder, anxiety disorders and major depression are commonly presented by these patients, and suicidal ideation and suicidal attempts affect a significant number of obesity surgery candidates. Research suggests that there is a higher level of general psychopathology among patients accepted for surgical treatments compared to those allocated to non-surgical weight loss treatments (Lapidoth, Ghaderi, & Norring, 2008), as well as that psychiatric disorders are prevalent among bariatric surgery patients and that those disorders are associated with greater obesity and lower functional health status (Kalarchian et al., 2007). Mühlhans, Horbach and Zwaan (2009), studying psychopathology in bariatric surgery candidates, concluded that, in Germany, about half of these patients presented an Axis I disorder previously to surgery. Age and gender differences found do not seem to justify differentiated intervention programmes regarding this, as psychological symptoms are very frequent in all the groups studied. Although research shows us that depression symptoms tend to improve rapidly after obesity surgery (Leombruni, et al., 2007), the severity of the symptoms presented, as well as the real risk of suicidal attempt, justifies a prompt pre-surgical psychological assessment and intervention.
The present study, similarly to previous studies (Mahoney, 2008), shows that candidates to obesity surgery report levels of anxiety and depression higher than normal. Results suggest that we should have these levels into account when conceiving intervention programmes, but also that we should be particularly attentive to anxiety levels, principally in what concerns to women. Many have been the studies which try to explore if psychopathology is a cause or a consequence of obesity. However, according to Hach et al. (2007), most of studies that have shown a relationship between obesityand mental health problems were based on selected clinical populations(potential help-seeking bias), fact that can lead us to a very partial understanding of this complex relation.
Self-concept revealed to be diminished in obesity surgery candidates from both genders comparing to general population, particularly in the younger age groups (15-19 and 20-29 years old patients). Thus, pre-surgical psychological intervention should also address this psychological variable. We believe that particularly self-efficacy perception should be addressed in psychological pre-surgical intervention, as this psychological variable can have important consequences in treatment adherence before and after the surgery.
In general, patients report poor quality of life in all the quality of life areas assessed – physical functioning, role-physical, bodily pain, general health, vitality, social functioning, role-emotional, mental health - as well as poor quality of life in what concerns to physical and mental domains. There is no direct relation between quality of life and patients BMI. Moreover, women reported worst quality of life in physical and mental domains than men.
Physical, social and psychological problems have a significant impact on the quality of life of patients with obesity diagnosis and they should play a leading role in deciding on surgical treatment for obesity (Sauerland, et al., 2005). Research reveals that obesity surgery is generally associated with improved psychological functioning and quality of life for most individuals, but it also suggests that preoperative distress can be a potentially important psychosocial predictor of success of obesity surgery (Vallis & Michael, 1993). Nevertheless studies as those presented by Tolonen, Victorzon e Mäkelä (2004), Rea et al. (2007) and van Hout, Fortuin, Pelle, Blokland-Koomen e van Heck (2009) revealed that after 12 months, patients general quality of life start to diminish again, although it seems to continue to exist better results than before surgery. It is necessary to develop longitudinal studies long enough to truly understand what happens throughout the years after surgery, but, for the present, we can hypothesize that obesity surgery is not a guarantee of an excellent quality of life for patients suffering from this chronic condition and health care teams should not contribute to the development of patients false expectations.
We believe that the primary objective of submitting obesity surgery candidates to psychological assessment is not to exclude them of this treatment option, neither to create obstacles to surgical treatment, but to contribute to the identification of risk factors for positive treatment outcomes, as well as to the implementation of psychological intervention programmes which can be put into practice in the context of individual or group sessions and that intend to promote higher well-being previously to surgery, and to promote surgical treatment efficacy and positive outcomes.
The majority of participants studied in this research were women. This reflects the fact women more often enrol in public hospitals consultations for weight lost treatment. Nevertheless, this can constitute a limitation in what concerns to gender differences analysis in the present study.
REFERENCES
Abilés, V., Rodríguez-Ruiz, S., Abilés, J., Mellado, C., García, A., Cruz, A.P., & Fernández-Santaella, M.C. (2010). Psychological characteristics of morbidly obese candidates for bariatric surgery. Obesity Surgery, 20, 161-167. doi: 10.1007/s11695-008-9726-1 [ Links ]
Bauchowitz, A.U., Gonder-Frederick, A., Olbrisch, M.E., Azarbad, L., Ryee, M.-Y., Woodson, M., Schirmer, B. (2005). Psychosocial evaluation of bariatric surgery candidates: A survey of present practices. Psychosomatic Medicine, 67, 825-32. [ Links ]
Burmeister, J.M., Hinman, N., Koball, A., Hoffmann, D.A., & Carels, R.A. (2013). Food addiction in adults seeking weight loss treatment. Implications for psychosocial health and weight loss. Appetite, 60, 103-110. doi: 10.1016/j.appet.2012.09.013 [ Links ]
Carmo, I., Santos, O., Camolas, J., Carreira, M., Medina, L., Reis, L., Galvão-Teles, A. (2007). Overweight and obesity in Portugal: National prevalence in 2003-2005. Obesity Reviews, 9, 11-19. doi: 10.1111/j.1467-789X.2007.00422.x [ Links ]
Friedman, K.E., Applegate, K., & Grant, J. (2007). Who is adherent with preoperative psychological treatment recommendations among weight loss surgery candidates? Surgery for Obesity and Related Diseases, 3, 376-382. doi: 10.1016/j.soard.2007.01.008 [ Links ]
Hach, I., Ruhl, U.E., Klose, M., Klotsche, J., Kirch, W., & Jacobi, F. (2007).Obesity and the risk for mental disorders in a representative German adult sample. The European Journal of Public Health, 17, 297-305. doi: 10.1093/eurpub/ckl227 [ Links ]
Kalarchian, M.A., Marcus, M.D., Levine, M.D., Courcoulas, A.P., Pilkonis, P.A., Ringham, R.M., ... Rofey, D.L. (2007). Psychiatric disorders among bariatric surgery candidates: Relationship to obesity and functional health status. American Journal of Psychiatry, 164, 328-334.doi:10.1176/appi.ajp.164.2.328 [ Links ]
Kaukua, J. (2004). Health-related quality of life in clinical weight loss studies. Unpublished thesis, Medical Faculty of the University of Helsinki, Helsinki.
Lapidoth, J.M., Ghaderi, A., & Norring, C. (2008). A comparison of eating disorders among patients receiving surgical vs non-surgical weight-loss treatments. Obesity Surgery, 18, 715-720. doi: 10.1007/s11695-007-9250-8 [ Links ]
Legenbauer, T., Petrak, F., Zeaan, M., & Herpetz, S. (2011). Influence of depressive and eating disorders on short- and long-term course of weight after surgical and nonsurgical weight loss treatment. Comprehensive Psychuiatry, 52, 301-311. doi: 10.1016/j.comppsych.2010.06.012 [ Links ]
Leombruni, P., Pierò, A., Dosio, D., Novelli, A., Abbate-daga, G., Morino, M., Fassino, S. (2007). Psychological predictors of outcome in vertical banded gastroplasty: A 6 months prospective pilot study. Obesity Surgery, 17, 941-948. doi: 10.1007/s11695-007-9173-4 [ Links ]
Madam, A.K., & Tichansky, D.S. (2005). Patients postoperatively forgot aspects of preoperative patient education. Obesity Surgery, 15, 1066-1069. doi: 10.1381/0960892054621198 [ Links ]
Mahoney, D. (2008). Psychological gender differences in bariatric surgery candidates.Obesity Surgery, 18, 607-610. doi: 10.1007/s11695-007-9245-5 [ Links ]
Ministério da Saúde (2012). Plano Nacional de Saúde 2012-2016. Lisboa: Direcção Geral da Saúde, Ministério da Saúde. [ Links ]
Mühlhans, B., Horbach, T., & Zwaan, M. (2009). Psychiatric disorders in bariatric surgery candidates: A review of the literature and results of a German prebariatric surgery sample. General Hospital Psychiatry, 31, 414-421. doi: 10.1016/j.genhosppsych.2009.05.004 [ Links ]
Niego, S.H., Kofman, M.D., Weiss, J.J., & Geliebter, A. (2007). Binge eating in the bariatric surgery population: A review of the literature. International Journal of Eating Disorders, 40, 349-359. doi: 10.1002/eat.20376 [ Links ]
Orth, W.S., Madan, A.K., Taddeucci, R.J., Coday, M., & Tichansky, D.S. (2008). Support group meeting attendance is associated with better weight loss. Obesity Surgery, 18, 391-394. doi: 10.1007/s11695-008-9444-8 [ Links ]
Pais-Ribeiro, J., Silva, I., Ferreira, T., Martins, A., Meneses, R., & Baltar, M. (2007). Validation study of a Portuguese version of the Hospital Anxiety and Depression Scale. Psychology, Health & Medicine, 12, 225-235. doi:10.1080/13548500500524088 [ Links ]
Pessina, A., Andreoli, M., & Vassallo, C. (2001). Adaptability and compliance of the obese patient to restrictive gastric surgery in the short term. Obesity Surgery, 11, 459-463. doi: 10.1381/096089201321209332 [ Links ]
Rea, J.D., Yarbrough, D.E., Leeth, R.R., Leath, T.D., & Clements, R.H. (2007). Influence of complications and extent of weight loss on quality of life after laparoscopic Roux-en-Y gastric bypass. Surgical Endoscopy, 21, 1095-1100. doi: 10.1007/s00464-007-9257-1 [ Links ]
Ribeiro, J.L.P. (2005). O importante é a saúde: Estudo de adaptação de uma técnica de avaliação do estado de saúde- SF-36. Portugal: Fundação Merck Sharp & Dohme. [ Links ]
Sauerland, S., Angrisani, L., Belachew, M., Chevallier, J.M., Favretti, F., Finer, N., Neugebauer, E.A. (2005). Obesity surgery. Evidence-based guidelines of the European Association for Endoscopic Surgery (E.A.E.S.). Surgical Endoscopy, 19, 200-221. doi: 10.1007/s00464-004-9194-1 [ Links ]
Serra, A.V. (1986). O Inventário Clínico de Auto-Conceito. Psiquiatria Clínica, 7,67-84. [ Links ]
The Medical Outcomes Trust. (1993). How to score the SF-36 health survey. Boston: The Medical Outcomes Trust. [ Links ]
Tolonen, P., Victorzon, M., & Mäkelä, J. (2004). Impact of laparoscopic adjustable gastric banding for morbid obesity on disease-specific and health-related quality of life. Obesity Surgery, 14, 788-795. doi: 10.1381/0960892041590755 [ Links ]
Vallis, T.M., & Michael, A.R. (1993). The role of psychological factors in bariatric surgery for morbid obesity: Identification of psychological predictors of success. Obesity Surgery, 3, 346-359. doi: 10.1381/096089293765559025 [ Links ]
van Hout, G., Fortuin, F.A., Pelle, A.J.M., Blokland-Koomen, M.L., & van Heck, G.L. (2009). Health-related quality of life following vertical banded gastroplasty. Surgical Endoscopy, 23, 550-556. doi: 10.1007/s00464-008-9860-9 [ Links ]
van Hout, G.C.M., Leibbrandt, A.J., Jakimowicz, J.J., Smulders, J.F., Schoon, E.J., van Spreeuwl, J.P., van Heck, G.L. (2003). Bariatric surgery and bariatric psychology: General overview and the Dutch approach. Obesity Surgery, 13, 926-931. doi: 10.1381/096089203322618795 [ Links ]
Welch, G., Wesolowski, C., Piepul, B., Kuhn, J., Romanelli, J., & Garb, J. (2008). Physical activity predicts weight loss following gastric bypass surgery: Findings from a support group survey. Obesity Surgery, 18, 517-524. doi: 10.1007/s11695-007-9269-x [ Links ]
World Health Organization (2014). Obesity and overweight. Fact Sheet nº311. Retrieved from http://www.who.int/mediacentre/factsheets/fs311/en/ [ Links ]
Endereço para Correspondência
Universidade Fernando Pessoa. Praça 9 de Abril, 349, 4249-004 Porto. Tel. 967003099. Brasil. E-mail: isabels@ufp.edu.pt
Recebido em 5 de Agosto de 2014/ Aceite em 25 de Setembro de 2014













