Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Revista Portuguesa de Pneumologia
versão impressa ISSN 0873-2159
Rev Port Pneumol v.15 n.4 Lisboa ago. 2009
Occupational (?) constrictive bronchiolitis with normal physical, functional and image findings
Sandra Figueiredo1
António Morais2
Adriana Magalhães2
Conceição Souto Moura3
João Almeida2
Isabel Gomes2
Abstract
Constrictive bronchiolitis is characterized by alterations in the walls of membranous and respiratory bronchioles. These changes lead to concentric narrowing or complete obliteration of the airway lumen.
Suspicion of possible bronchiolar disorders may arise from clinical, funcional, and radiologic findings.
However, constrictive bronchiolitis may be present even with normal physical, functional and image findings, which turns the diagnosis difficult. A high index of suspicion is necessary to justify invasive tests that lead to pulmonary biopsy. In this report, we describe a patient with cough and dyspnoea, with normal physical, functional and image findings, whose work-up leaded to the diagnosis of constrictive bronchiolitis.
Key-words: Constrictive bronchiolitis; iron oxide.
Bronquiolite constritiva ocupacional (?) em doente com exame físico, radiológico e funcional normal
Resumo
A bronquiolite constritiva é caracterizada por alterações das paredes dos bronquíolos membranosos e respiratórios. Estas alterações incluem um espectro de alterações que podem variar, desde a inflamação à fibrose concêntrica progressiva, com obstrução completa do lúmen bronquiolar. O diagnóstico pode ser sugerido pela história clínica e por alterações radiológicas e funcionais. No entanto, o exame físico e os exames complementares de diagnóstico podem ser normais, o que dificulta o diagnóstico, sendo necessário um elevado índice de suspeita para se sujeitar o doente a exames invasivos, tal como a biópsia pulmonar cirúrgica. Os autores apresentam um caso clínico de uma doente com quadro arrastado de tosse e dispneia, com exame físico, funcional e imagiológico normais, cujo estudo exaustivo veio a revelar o diagnóstico de bronquiolite constritiva.
Palavras-chave: Bronquiolite constritiva, óxido de ferro.
Case report
The authors present a case report of a 26 years old Caucasian female that was referred to hospital with symptoms of cough and dyspnoea at the work place, which had been present for 2 years. She had no history of tobacco use or previous respiratory disease. She had worked with copy-machines for several years until 2 months before the first visit. Symptoms improved when she was away from the work place and, at the time of observation, she had no respiratory symptoms and presented a normal physical examination, including pulmonary and cardiac auscultation.
Laboratory studies, including blood tests, RAST and D-dimers, were within normal range. Lung function tests with spirometry, lung volumes and DLCO were normal. Arterial blood gases were also normal. A chest radiograph (Fig. 1) revealed no abnormalities.

Fig. 1 – Chest radiograph
Subsequently, a High Resolution Computerized Tomography (HRCT) of the chest was performed (Fig. 2A, B and C) which was normal, as well.
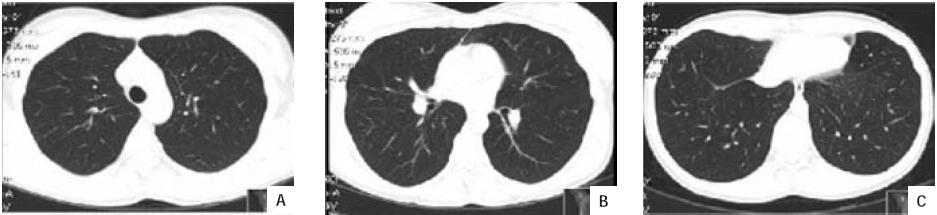
Fig. 2 – (A,B and C) High-resolution computed tomography of the chest
The patient returned to the work place for a fortnight just to perform a PEF curve with morning and evening measurements, but it did not suggest occupational asthma. A methacoline challenge was undertaken and was negative. She managed 517 metres during the 6-minute walk test with no significant drop in saturation (3%).
Ten months after the first visit, the patient was still away from work, without respiratory symptoms outside the context of common colds, and her physical examination was still normal, as well as pulmonary function tests and methacoline challenge. So as to exclude any involvement not detected by the previous tests, fiber optic bronchoscopy was then performed, with unremarkable endoscopic findings. However, the bronchoalveolar lavage done in the right middle lobe revealed a lymphocytosis (32,4%) with a normal CD4/CD8 ratio.
At this point, a lung specimen was needed and surgical lung biopsy was recommended to the patient. Histopathological assessment (Fig. 3) revealed Lesions of chronic cellular bronchiolitis, fibrosis and smooth muscle proliferation of the bronchiolar wall, suggestive of constrictive bronchiolitis... .
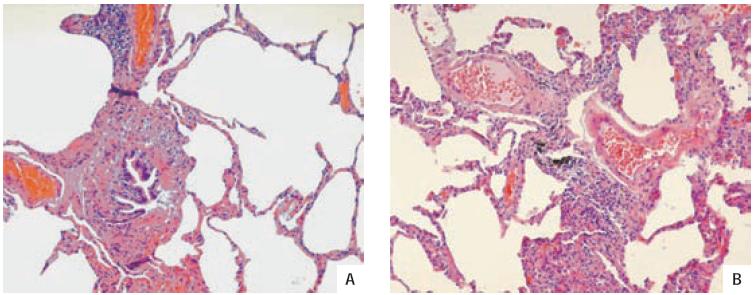
Fig.3 – (A) Concentric fibrosis surronding the bronchiole lumen (HE 400x); (B) The bronchiole is infiltrated by chronic inflammatory cells (HE 400x)
Treatment with oral deflazacort was started and maintained for 6 weeks, but it was discontinued since the patient was clinically stable and possible benefits would not balance long-term side-effects. She has been medicated with an inhaled corticosteroid since then.
The powder composition of the copy-machine was evaluated and it included iron oxide, which has been associated with bronchiolitis. No other suggestive agent was reported by the patient in her environment, including of protein origin. She has been kept away from copy-machines ever since and she has been clinically and functionally stable for a 22 months follow-up period.
Discussion
Mineral dust exposure is classically associated with restrictive lung disease. However mineral dusts can also produce abnormalities in the small airways with airway obstruction1,2.
The deposition of inhaled dust around small airways appears to lead to a repair mechanism with an inflammatory response that may induce bronchiolar and alveolar epithelium injury1-4. This process may result in complete recovery or may be characterized by proliferation of granulation tissue with concentric narrowing or complete obliteration of the airway lumen, which, in constrictive bronchiolitis, occurs at the level of membranous and respiratory bronchioles. Among those subjects exposed to mineral dusts, individual susceptibility to this bronchiolar lesion may determine by individual ability to clear these particles from the airways1.
Iron oxide has been implicated in the etiopathogeny of constrictive bronchiolitis and it was present in the toner composition of the copy-machines, at the patients work place. Although direct implication can not be assured, it is possible that it triggered the inflammatory response for the initiation of the lesions in this case.
Clinical manifestations of constrictive bronchiolitis depend upon the type, extent or severity of the lung injury and tend to progress with time, with increasing dyspnoea, wheezing and cough, but sputum production can also be present. This woman was symptomatic only at the work place.
Radiographic abnormalities may be absent or include progressive increase in lung volume on serial radiographs or marked heterogeneity of lung density in HRCT scan. In this case, HRCT in expiration was not performed previously to pulmonary biopsy, and it could have shown a mosaic pattern suggestive of heterogeneity. However, to perform this exam in this patient, a high index of suspicion would also be needed and, even with a positive finding, it would not preclude invasive diagnostic procedures.
The interest of perfusion and ventilation isotope lung scans has been mentioned in some forms of bronchiolitis5, but findings are expressive when patients have significant functional impairment. In fact, in bronchiolitis, pulmonary function tests typically present an obstructive defect with hyperinflation that was not present in this patient.
In our opinion, the remarkable feature in this case is that constrictive bronchiolitis was present when different non-invasive tests for evaluation of small airway disease were normal, which turned the diagnosis difficult, and a high index of suspicion was necessary to justify the invasive procedures that lead to lung biopsy.
Bibliography
1. Ryu JH, Myers JL, Swessen SJ. Bronchiolar disorders. Am J Respir Crit Care Med 2003; 168: 1277 -1292. [ Links ]
2. Ryu JH. Classification and approach to bronchiolar diseases. Curr Opin Pulm Med 2006; 12(2):145 -151.
3. Schlesinger C, Meyer CA, Veeraraghavan S, Koss MN. Constrictive (obliterative) bronchiolitis: diagnosis, etiology and a critical review of the literature. Ann Diagn Pathol 1998; 2(5):321 -334.
4. Visscher DW, Myers JL. Bronchiolitis. The pathologists perspective. Proc Am Thorac Soc 2006; 3: 41-47.
5. Hasegawa Y, Imaizumi K, Sekido Y, Iinuma Y, Kawabe T, Hashimoto N, Shimokata K. Perfusion and ventilation isotope lung scans in constrictive bronchiolitis obliterans. Respiration 2002; 69:550 -555.
1 Internato Médico. Serviço de Pneumologia
2 Assistente Hospitalar Graduado. Serviço de Pneumologia
3 Assistente Hospitalar Graduado. Serviço de Anatomia Patológica
Hospital de São João (EPE), Porto
Recebido para publicação/received for publication: 08.10.14
Aceite para publicação/accepted for publication: 09.02.05













