Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Jornal Português de Gastrenterologia
versão impressa ISSN 0872-8178
J Port Gastrenterol. vol.21 no.1 Lisboa fev. 2014
https://doi.org/10.1016/j.jpg.2013.10.003
CLINICAL CASE
Endoscopic management of a delayed diagnosed foreign body esophageal perforation
Abordagem endoscópica de uma perfuração esofágica por corpo estranho com 5 dias de evolução
Eduardo Rodrigues-Pinto∗, Pedro Pereira, Guilherme Macedo
Gastroenterology Department, Centro Hospitalar São João, Porto, Portugal
*Corresponding author
ABSTRACT
Foreign body-induced perforation is responsible for 16.7% of esophageal perforations and may be associated with respiratory failure, sepsis or hemorrhage if delayed diagnosis and treatment. The mortality rate of esophageal perforations hovers close to 20%, especially if treatment is delayed more than 24 h. Esophageal perforation management remains controversial and treatment decisions should be individualized depending on the etiology of perforation, degree of mediastinopleural contamination, underlying esophageal disease, and overall health status of the patient. We report a case of successful endoscopic management in a delayed diagnosis of an esophageal perforation presenting with an associated peri-esophageal abscess.
Keywords: Esophageal perforation; Foreign bodies; Endoscopy
RESUMO
Perfuração por corpo estranho é responsável por 16,7% de perfurações esofágicas, podendo ser complicada por insuficiência respiratória, sépsis ou hemorragia, principalmente se houver atraso no diagnóstico e/ou tratamento. A taxa de mortalidade das perfurações esofágicas ronda os 20%, sobretudo quando o intervalo de tempo até ao tratamento ultrapassa as 24 h. A abordagem da perfuração esofágica é um tema controverso e as decisões terapêuticas devem ser individualizadas, dependendo da etiologia da perfuração, do grau de infeção mediastínico/pleural, da patologia esofágica de base e do estado geral do doente. Descrevemos um caso clínico de uma abordagem endoscópica de uma perfuração esofágica por corpo estranho com 5 dias de evolução, com abcesso peri-esofágico associado.
Palavras-chave: Perfuração esofágica; Corpo estranho; Endoscopia
Introduction
Foreign body ingestion and food bolus impaction occur commonly,1,2 however, most ingested foreign bodies that reach the stomach pass safely through the intestinal tract. Foreign body-induced esophageal perforation is responsible for 16.7% of esophageal perforations and it has been regarded as the most serious injury of the digestive tract,3 particularly if not diagnosed and treated promptly, being associated with respiratory failure, sepsis or hemorrhage.4 The mortality rate of esophageal perforations hovers close to 20%, especially in cases in which treatment is delayed for more than 24 h.5 Esophageal perforation management remains controversial and treatment decisions should be individualized depending on the duration of impaction, type of foreign body, size and perforation.6 Surgical primary repair is often the preferred approach, however, there may be a role for interventional endoscopy including the use of stents.7,8 Treatments performed before the development of mediastinitis are lifesaving in esophageal perforation patients.9
We report a case of successful endoscopic management in a delayed diagnosis of an esophageal perforation presenting with an associated peri-esophageal abscess.
Case report
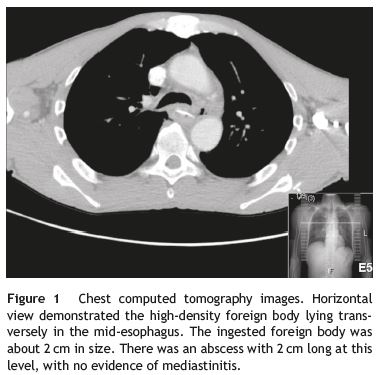
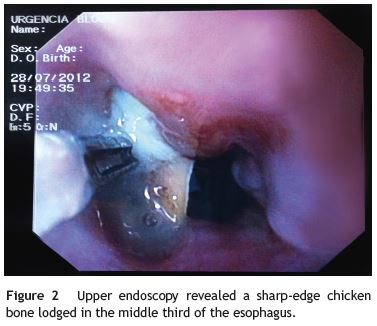
A 57 year-old man was referred to the emergency room due to suspicion of a foreign body impaction. The patient complaints were substernal chest pain, with solid food dyspaghia, fever, progressive prostration and pointed out that he had eaten chicken 5 days before. Blood chemistry revealed leukocytosis and increased C-reactive protein (147 mg/L) and there were no reported abnormalities at the chest X-ray. Computed tomography scan of the chest and neck revealed foreign body in the mid-esophagus, 18 cm below epiglottis upper edge, between left pulmonar artery and aortic arch, with suggestive signs of perforation at this level and a small (2 cm) peri-esophageal abscess (Fig. 1). There was no evidence of pneumothorax or soft tissue emphysema. After discussing with the surgeons, upper endoscopy under general anesthesia was performed, with patient consent, in the presence of a surgical team. Na across located sharp-edged chicken bone (4 cm long) was identified in the mid-esophagus, with bilateral perforation of submucosa and muscular layers with the surrounding área being ulcerated bilaterally. The chicken bone was gently removed with a mouse tooth forceps (Fig. 2) after identification of the shallower end, with immediately drainage of the abscess onto the esophageal lumen. A 2 cm long midesophageal perforation was visualized. Given the lack of pulmonary symptoms and no evidence of mediastinitis, the team decided on nonsurgical management. To allow further drainage, without blocking with a stent, a nasogastric tube was placed under direct visualization. The patient was started on broad-spectrum antibiotherapy, protón pump inhibitors and total parenteral nutrition. The control esophagogram (Fig. 3) and computed tomography scan, performed in the day after, revealed a small-contained leak, with no evidence of mediastinic extravasation and no regional signs of infection. The patient was kept on total parenteral nutrition for 8 days, started enteral nutrition on the eighth day and progressed to oral feeding on the twelfth day. The two-week control esophagogram revealed no signs of leakage. Patient improved steadily, with normalization of blood chemistry parameters of infection (C-reactive protein 3 mg/L at discharge), with no in-hospital complications and no complaints of difficulty in swallowing. He was discharged on proton pump inhibitors.

Discussion
Although the primary treatment for esophageal perforation is surgical, endoscopic therapies may play a role and be appropriate in individualized cases. Treatment depends on the etiology, site, and size of perforation, the time elapsed between perforation and diagnosis, underlying esophageal disease and the overall health status of the patient. Criteria for non-surgical treatment include perforation that is confined to the mediastinum, drainage of the cavity back into the esophagus, clinical stability, and minimal clinical signs of sepsis.10,11 Perforation of the cervical esophagus can be managed conservatively in most cases, as well as, perforations of the intrathoracic esophagus that are confined to the mediastinum12; however, perforations of the lower two thirds of the esophagus that affect the pleura, pericardium, or peritoneum require rapid surgical intervention. Choosing an endoscopic therapy for an esophageal perforation requires differentiating between acute and chronic cases. Currently, endoscopic clips are the only devices available for closure of perforations, as suturing and stapling devices are not yet available for clinical use. Endoclips may be adequate for linear or regular perforations up to 2 cm in size,13 however, irregular perforations or deep-penetrating lacerations of the esophageal wall may be better treated with overthe- scope clipping system, once it ensures the full-thickness approximation of the edges.14 Stents should be considered in the closure of acute esophageal perforations immediately after its detection, in the closure of longstanding perforations in patients who are not candidates for surgery, in perforations larger than 2 cm, in defects with everted edges and in patients with a leak occurring in the setting of a malignant lesion.15 Endoscopic sealants may be an option in esophageal fistulas, depending on the size of the fistula and the absence of active infection around the site of the leak, cancer, or obstruction distal to the site of the leak.16 For large esophageal defects with extravisceral collection that could be endoscopically explored, vacuum-assisted closure may be an option.17 This method allows regular visualization of the leak and infected cavity and promotes tissue granulation to obtain a secondary-intention closure of the fistula.
In our case, nonsurgical management was chosen, based on the fact that patients general condition was not impaired and progressive sepsis was not apparent. The primary goal of treatment in esophageal perforations should be the sealing of the wall defect as soon as possible. Despite encouraging results achieved with the use of several devices,13-17 in our case, due to the existence of an abscess, we chose not to use any stent, once it could compromise complete drainage and promote progressive sepsis. This way, after gently removing the chicken bone, we decided to place a nasogastric tube under direct visualization in order to allow a faster healing and introduction of enteral feeding.
The optimal approach to esophageal perforation remains controversial, and there must be an individual assessment. Nonsurgical management can be applied in carefully selected cases and can be a safe method for specific esophageal perforations.
References
1. Ginsberg GG. Management of ingested foreign objects and food bolus impactions. Gastrointest Endosc. 1995;41:33-8. [ Links ]
2. ASGE Standards of Practice Committee, Ikenberry SO, Jue TL, Anderson MA, Appalaneni V, Banerjee S, et al. Management of ingested foreign bodies and food impactions. Gastrointest Endosc. 2011;73:1085-91. [ Links ]
3. Tsalis K, Blouhos K, Kapetanos D, Kontakiotis T, Lazaridis C. Conservative management for an esophageal perforation in a patient presented with delayed diagnosis: a case report review of the literature. Cases J. 2009;15:6784. [ Links ]
4. Kanowitz A, Markovchick V. Oesophageal and diaphragmatic trauma. In: Rosen P, editor. Emergency medicine: concepts and clinical practice. 4th ed. St. Louis: Mosby; 1998. p. 546-8. [ Links ]
5. Eroglu A, Can Kurkcuogu I, Karaoganogu N, Tekinbas C, Yimaz O, Basog M. Esophageal perforation: the importance of early diagnosis and primary repair. Dis Esophagus. 2004;17:91-4. [ Links ]
6. Sung SH, Jeon SW, Son HS, Kim SK, Jung MK, Cho CM, et al. Factors predictive of risk for complications in patients with oesophageal foreign bodies. Dig Liver Dis. 2011;43:632-5. [ Links ]
7. Chirica M, Champault A, Dray X, Sulpice L, Munoz-Bongrand N, Sarfati E, et al. Esophageal perforations. J Visc Surg. 2010;147:e117-28. [ Links ]
8. van Heel NC, Haringsma J, Spaander MC, Bruno MJ, Kuipers EJ. Short-term esophageal stenting in the management of benign perforations. Am J Gastroenterol. 2010;105:1515-20. [ Links ]
9. Arslan E, Sanl M, Islk AF, Tuncozgur B, Ulusan A, Elbeyli L. Treatment for esophageal perforations: analysis of 11 cases. Ulus Travma Acil Cerrahi Derg. 2011;17:516-20.
10. Huber-Lang M, Henne-Bruns D, Schmitz B, Wuerl P. Esophageal perforation: principles of diagnosis and surgical management. Surg Today. 2006;36:332-40. [ Links ]
11. Tsalis K, Vasiliadis K, Tsachalis T, Christoforidis E, Blouhos K, Betsis D. Management of Boerhaaves syndrome: report of three cases. J Gastrointestin Liver Dis. 2008;17:81-5. [ Links ]
12. Tsalis K, Blouhos K, Kapetanos D, Kontakiotis T, Lazaridis C. Conservative management for an esophageal perforation in a patient presented with delayed diagnosis: a case report. Cases J. 2009;22:164. [ Links ]
13. Fujishiro M, Yahagi N, Kakushima N, Kodashima S, Muraki Y, Ono S, et al. Successful nonsurgical management of perforation complicating endoscopic submucosal dissection of gastrointestinal epithelial neoplasms. Endoscopy. 2006;38:1001-6. [ Links ]
14. Kirschniak A, Kratt T, Stuker D, Braun A, Schurr MO, Konigsrainer A. A new endoscopic over-the-scope clip system for treatment of lesions and bleeding in the GI tract: first clinical experiences. Gastrointest Endosc. 2007;66:162-7. [ Links ]
15. Dumonceau JM, Deviere J, Cappello M, Van Gossum A, Cremer M. Endoscopic treatment of Boerhaaves syndrome. Gastrointest Endosc. 1996;44:477-9. [ Links ]
16. Tringali A, Daniel FB, Familiari P. Endoscopic treatment of a recalcitrant esophageal fistula with new tools: stents Surgisis, and nitinol staples. Gastrointest Endosc. 2010;72:647-50. [ Links ]
17. Wedemeyer J, Schneider A, Manns MP, Jackobs S. Endoscopic vacuum-assisted closure of upper intestinal anastomotic leaks. Gastrointest Endosc. 2008;67:708-11. [ Links ]
*Corresponding author
E-mail address: edu.gil.pinto@gmail.com (E. Rodrigues-Pinto).
Ethical disclosures
Protection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of data. The authors declare that they have followed the protocols of their work center on the publication of patient data and that all the patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consent. The authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interest
The authors have no conflicts of interest to declare.
Received 29 April 2013; accepted 28 October 2013













