Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Jornal Português de Gastrenterologia
versão impressa ISSN 0872-8178
J Port Gastrenterol. vol.20 no.5 Lisboa set. 2013
https://doi.org/10.1016/j.jpg.2012.12.010
IMAGES IN GASTROENTEROLOGY AND HEPATOLOGY
Colonic migration of a percutaneous endoscopic gastrostomy with jejunal extension
Migração de Gastrostomia Endoscópica Percutânea com prolongamento jejunal para o colon
João Santos-Antunes∗, Amadeu C.R. Nunes, Filipe Vilas-Boas, Regina Gonçalves, Susana Lopes, Guilherme Macedo
Gastrenterology Department, Centro Hospital S. João, Porto, Portugal
* Corresponding author
Case description
A 67 years-old man, with a medical history of Parkinsons disease, was under Duodopa, Abbott (levodopa 20 mg/mL and carbidopa 5 mg/mL intestinal gel) through a percutaneous endoscopic gastrostomy with jejunal extension (PEG-J) placed in 2010, with excellent response to treatment. An X-ray was performed in early 2011 for other reasons and showed appropriate location of the jejunal extension.
He was referred to the gastroenterology clinic in January 2012 because of rectal bleeding. He also noticed that Duodopa was recently loosing efficacy, and symptoms of Parkinsons disease were recurring. No other symptoms were referred, namely pain, diarrhoea, weight loss or stoma discharge.
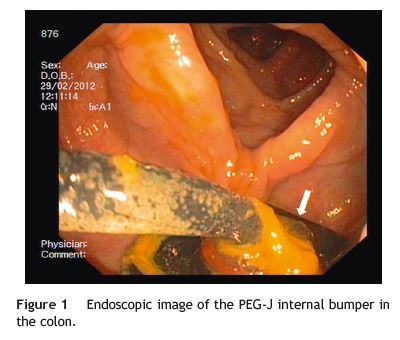
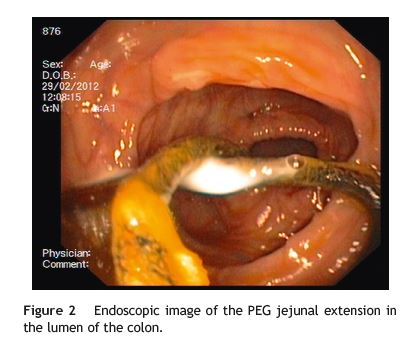
We performed a colonoscopy that showed a polypoid mass in the sigmoid (adenocarcinoma on histological examination) and a tube in transverse and ascending colon (Figs 1 and 2).
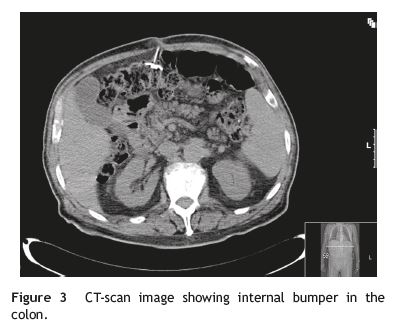
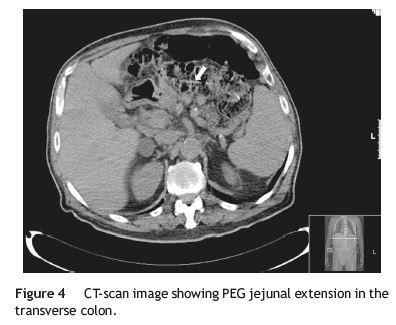
A CT-scan was performed for staging, which demonstrated that the entire extension of PEG-J was in the colon (Figs 3 and 4), and that the anterior gastric body Wall was thinner than normal. On esophagogastroduodenoscopy (EGD), a depression was found in the corresponding location.
The patient underwent a left hemicolectomy, and PEG-J was surgically removed from the colon.
Discussion
Comparing to a regular PEG, direct jejunal feeding is more indicated in patients with chronic aspiration of gastric contents, in those needing concomitant gastric decompression or for administration of drugs that must be directly delivered to duodenum or jejunum to achieve a more precise and controlled absorption. In this setting, PEG-J is more often performed than direct percutaneous endoscopic jejunostomy, despite the risk of tube dysfunction or dislocation in the former technique.1,2
Migration of a PEG to the colon is an infrequent but described long-term complication.3,4 The underlying cause can be related to iatrogenic puncture of the colon when the initial procedure for PEG insertion is performed. Then, the excessive tension that is applied on the gastrostomy tube can induce the migration of the bumper from the stomach to the colon trough the iatrogenic gastrocolic fistula. The presence of post-surgical adhesions, a high-riding transverse colon and stomach over-distension during EGD for PEG placement are known predisposing risk factors.5 However, this is the first report of a complete colonic migration of a PEG-J: the internal bumper migrated to the colon and its jejunal extension was completely pulled behind probably due to peristaltic movements.
These patients with colocutaneous fistula may have no symptoms, as observed in our case. In the other hand, they can present subacute diarrhoea, cramping, odorous faecal leakage from the stoma or undigested food in the tube when there is a concomitant residual gastrocolic fistula.3,5 Treatment can be conservative in most patients and consists of endoscopic removal of the PEG, with spontaneous closure of the colocutaneous fistula within days. In patients with peritonitis, laparotomy must be considered. Concerning our patient, surgical removal was performed due to the appropriate management of the adenocarcinoma of the colon.
References
1. DiSario JA. Endoscopic approaches to enteral nutritional support. Best Pract Res Clin Gastroenterol. 2006;20:605-30. [ Links ]
2. Zopf Y, Rabe C, Bruckmoser T, Maiss J, Hahn EG, Schwab D. Percutaneous endoscopic jejunostomy and jejunal extension tube through percutaneous endoscopic gastrostomy: a retrospective analysis of success, complications and outcome. Digestion. 2009;79:92-7. [ Links ]
3. Lenzen H, Weismüller T, Bredt M, Bahr M. Gastrointestinal: PEG feeding tube migration into the colon; a late manifestation. J Gastroenterol Hepatol. 2012;27:1254. [ Links ]
4. Liu SY, Ng SS, Yip HC, Teoh AY, Chiu PW, Ng EK. Migration of a percutaneous endoscopic gastrostomy tube into the transverse colon: a forgotten cause of refractory diarrhea. Endoscopy. 2010;42 Suppl 2:E324-5. [ Links ]
5. Friedmann R, Feldman H, Sonnenblick M. Misplacement of percutaneously inserted gastrostomy tube into the colon: report of 6 cases and review of the literature. JPEN. 2007;31:469-76. [ Links ]
Ethical disclosures
Protection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of data. The authors declare that no patient data appear in this article.
Right to privacy and informed consent. The authors declare that no patient data appear in this article.
Conflicts of interest
The authors have no conflicts of interest to declare.
*Corresponding author
E-mail address: joao.claudio.antunes@gmail.com (J. Santos-Antunes).
Received 30 October 2012; accepted 5 December 2012













