Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Jornal Português de Gastrenterologia
versão impressa ISSN 0872-8178
J Port Gastrenterol. vol.20 no.5 Lisboa set. 2013
https://doi.org/10.1016/j.jpg.2013.03.004
ENDOSCOPIC SPOT
Lower gastrointestinal bleeding: An unusual cause
Hemorragia Digestiva Baixa: uma causa rara
Joana Machado∗, Paula Ministro, Eugénia Cancela, Américo Silva
Serviço de Gastrenterologia, Centro Hospitalar Tondela-Viseu EPE, Viseu, Portugal
* Corresponding author
An 83-year-old Caucasian male presented in the emergency room with active lower gastrointestinal bleeding with few hours of evolution and diffuse abdominal pain with 3 days of duration. The patient mentioned significant weight loss during the previous year (20 kg). He denied previous or concomitant gastrointestinal symptoms. At admission he was hemodynamically stable. Laboratory findings showed hemoglobin level of 12.1 g/L, without other abnormalities. Abdominal examination was unremarkable and rectal digital examination showed bright red blood on the finger glove.
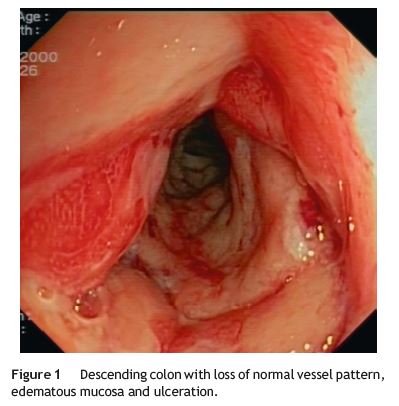
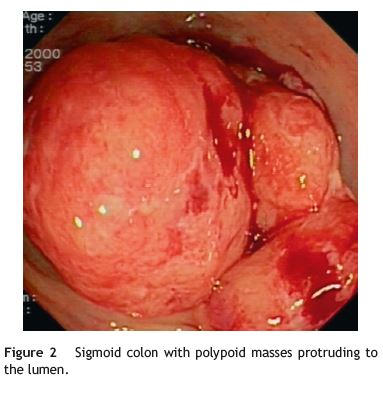
A left colonoscopy was performed and revealed loss of normal vascular pattern, descending colon with granular mucosa and some ulcers (Fig. 1), sigmoid colon and rectum presented multiple bulky polypoid masses protruding to the lumen, with superficial erosions and bleeding (Fig. 2). Biopsies were acquired for histological evaluation.
An abdominal CT-scan was performed and revealed heterogeneous splenomegaly and multiple mesenteric, para-aortic and intercavo-aortic adenopathies.
Histological examination disclosed atypical lymphoid cells with irregular nuclei without conspicuous nucleoli and scant cytoplasm, some mitotic figures and apoptotic bodies (Fig. 3A). Immunohistochemical analysis: positive staining for CD20 (Fig. 3B) and CD5 (Fig. 3C).
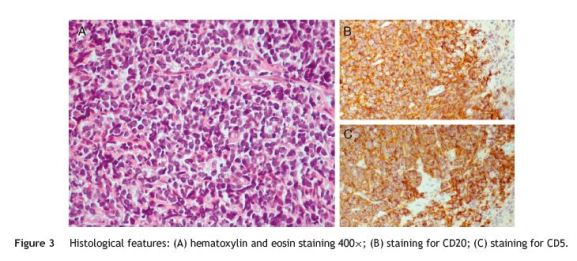
Bone marrow involvement was also confirmed. The diagnosis of mantle cell lymphoma (MCL) was established (stage IV).
The patient died some weeks later with an infectious complication before chemotherapy was initiated.
MCL is an aggressive B cell neoplasm of small to médium sized lymphocytes with over expression of cyclin D1 caused by translocation (11;14). Immunophenotyping is commonly used, the majority of MCL co-express CD20, CD5 and cyclin D1 and are usually negative for CD10 and Bcl6.1,2
MCL represents about 4% of all lymphomas in the US and 7-9% in Europe.1 MCL arises in older adults (median age of presentation 60-65 years) and has a male predominance.1-3
The presence of multiple lymphomatous polyps along the gastrointestinal (GI) tract was first described in 1961 as clinicopathological entity, Multiple Lymphomatous Polyposis (MLP), and subsequently was found to represent involvement of the GI tract by MCL. Whether MLP as GI tract MCL is a diferente entity from the involvement of GI tract in peripheral MCL is not clear.4
The reported frequency of GI tract involvement in patients with MCL is probably underestimated because, in most studies, endoscopic evaluation was only performed in patients with GI symptoms. A study that aimed to determine the frequency of GI involvement and its clinical significance in MCL found that only 26% of patients presented with GI symptoms at the time of diagnosis. In the same study, MCL was present histologically in the lower GI tract of 53 of 60 patients (88%) and in the upper GI tract of 28 of 58 patients (43%). Microscopic evidence of disease was found in a significant number of patients with macroscopically normal endoscopic evaluation.5 Colonoscopy and upper GI endoscopy, as part of staging investigations in MCL, rarely changes clinical management, therefore, routine Endoscopy and colonoscopy cannot be recommended for all patients at baseline.3,5
Patients with MCL generally have stage III/IV disease at presentation and despite treatment the overall prognosis remains poor.1,2
References
1. Vose JM. Mantle cell lymphoma: 2012 update on diagnosis, risk-stratification, and clinical management. Am J Hematol. 2012;87:604-9. [ Links ]
2. Swerdlow SH, Campo E, Seto M, Muller-Hermelink HK. Mantle cell lymphoma. In: Swerdlow SH, Campo E, Harris NL, Jaffe ES, Pileri SA, Stein H, Thiele J, Vardiman JW, editors. WHO classification of tumours of haematopoietic and lymphoid tissues. 4th ed. Lyon: International Agency for Research on Cancer; 2008. p. 229-32. [ Links ]
3. McKay P, Leach M, Jackson R, Cook G, Rule S. Guidelines for the investigation and management of mantle cell lymphoma. Br J Haematol. 2012;159:405-26. [ Links ]
4. Ruskoné-Fourmestraux A, Audouin J. Primary gastrointestinal tract mantle cell lymphoma as multiple lymphomatous polyposis. Best Pract Res Clin Gastroenterol. 2010;24:35-42. [ Links ]
5. Romaguera JE, Medeiros LJ, Hagemeister FB, Fayad LE, Rodriguez MA, Pro B, et al. Frequency of gastrointestinal involvement and its clinical significance in mantle cell lymphoma. Cancer. 2003;97:586-91. [ Links ]
Ethical disclosures
Protection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of data. The authors declare that they have followed the protocols of their work center on the publication of patient data and that all the patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consent. The authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interest
The authors have no conflicts of interest to declare.
*Corresponding author
E-mail address: jlvmachado@hotmail.com (J. Machado).
Received 19 December 2012; accepted 22 March 2013













