Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Jornal Português de Gastrenterologia
versão impressa ISSN 0872-8178
J Port Gastrenterol. vol.20 no.1 Lisboa jan. 2013
https://doi.org/10.1016/j.jpg.2012.07.016
Multiple, large pyogenic liver abscesses treated conservatively: A case-report and review of the literature
Múltiplos abcessos hepáticos proxémicos volumosos tratados de forma conservadora: relato de um caso e revisão da literatura
Christos E. Lampropoulosa,∗, Ioanna Papaioannoua, Zoi Antonioub, Kyriaki Ermidoua, Efi Papadimab, Nikos Spiliopoulosa, Manolis Choustoulakisc, Grigoris Apostolidisa, Konstantina Alexopouloua, Panagiotis Herasa
a Department of Internal Medicine, General Hospital of Nafplio, Greece
b Department of Radiology, General Hospital of Nafplio, Greece
c Department of Surgery, General Hospital of Nafplio, Greece
*Corresponding author.
ABSTRACT
Pyogenic liver abscesses are a rare cause of admission. Treatment consists of combined antibiotics regimen and surgical intervention. An unusual case of a patient with multiple, large, pyogenic abscesses of the left lobe treated conservatively is described below.
Keywords Liver abscess; Amebic abscess; Laboratory diagnosis; Treatment
RESUMO
Os abcessos hepáticos piogénicos são uma causa rara de admissão. O tratamento consiste num regime combinado de antibióticos e intervenc¸ão cirúrgica. Um caso invulgar de um doente com vários abcessos piogénicos volumosos no lobo esquerdo tratados conservadoramente descrito abaixo.
Palavras-Chave Abcesso hepático; Abcesso amebiano; Diagnóstico laboratorials; Tratamento
Introduction
Pyogenic liver abscesses are a rare cause of admission, with 3.59 cases per 100,000 people. They usually appear as an acute disease with fever, right upper-quadrant pain and jaundice. Blood cultures are positive in 52% of the cases and the most common pathogens are Streptococcus species and Escherichia coli while in Asia the most common pathogen is Klebsiella. Treatment consists of combined antibiotics regimen and surgical intervention (aspiration, drainage or resection) except solitary or small abscesses which are treated with antibiotics only.
An unusual case of a patient with multiple, large, pyogenic abscesses of the left lobe treated conservatively is described below, with her consent.
Case report
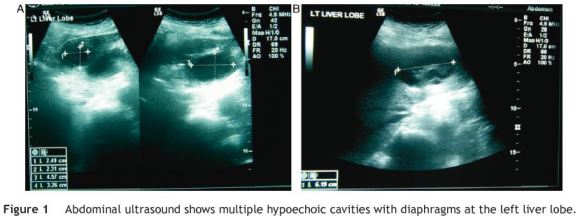
An 85-year-old lady presented with fever (up to 39 ◦C) and rigors, dyspnea and abdominal pain the last 24 h. Her medical history included dementia and hypertension under treatment as well as cholecystectomy 35 years ago with ERCP one year later because of cholangitis. The only clinical finding was tenderness of the right hypochondrium. Laboratory investigation showed: WBC: 17,800/_L, Ht: 37.7%, Hb: 12.0 g/dL, ESR: 100/1 h, glucose: 184 mg/dL, urea: 71 mg/dL, creatinine: 2.2 mg/dL, SGOT: 73 IU/L, SGPT: 58 IU/L, proteins: 6.5 g/dL, albumin: 2.6 g/dL, CRP: 16.3 mg/dL (normal value < 0.5) and metabolic acidosis with compensatory respiratory alkalosis from gas analysis. The rest of laboratory findings (ALP, _GT, LDH, bilirubin, CPK, amylase and electrolytes) were normal. Chest X-ray revealed small bilateral pleural effusions (exudates after aspiration) and heart ultrasound showed small pericardial effusion. An abdomen ultrasound showed multiple hypoechoic cavities with diaphragms at the left lobe (the largest were 6.2, 5.6 and 4.6 cm respectively, Fig. 1). Abdominal computerized tomography (CT) showed multiple hypodense cavities of left liver lobe (the largest was 7 cm) with irregular, thick, ill-defined borders, presence of air in the intrahepatic bile ducts and faint, thin wall enhancement after intravenous contrast administration (Fig. 2). Patient was suffering from multiple liver abscesses with sepsis (SIRS with organs dysfunction: temperature > 38 ◦C, WBC> 12,000/_L, respiratory rate > 20 breaths/min and heart rate > 90 beats/min due to infection with acute renal failure, pleural and pericardial effusions). The patient was repeatedly advised by surgeons to undergo a surgical intervention (fine needle aspiration or resection), but she denied any kind of operation. A combined drug regimen was immediately started (IV ciprofloxacin 400 mg×2 with metronidazole 500 mg×3). After one week, ciprofloxacin was substituted by ampicillin/ sulbactam (12 g/day) and amikasin (1 g/day) as there was no improvement. Blood cultures were negative. Fever was sustained up to 38 ◦C the first two weeks with gradual remission the next five days. The patient was discharged afebrile five days later with per os treatment (ciprofloxacin 1 g/day and metronidazole 1.5 g/day) for two weeks. Her blood tests were normal apart from Ht (28.3%) and Hb (9.4 g/dL) and the effusions (both pleural and pericardial) were absorbed.
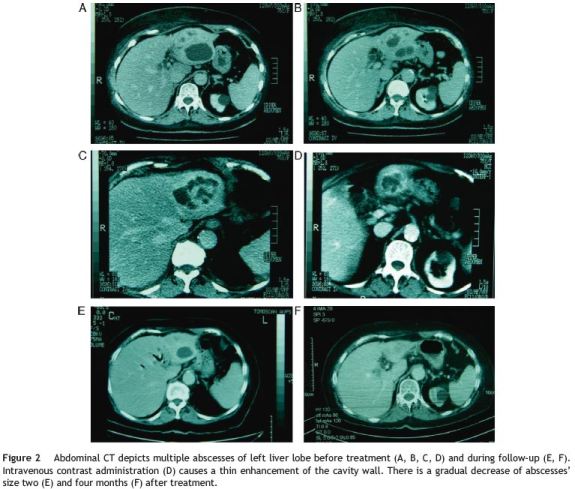
Although the patient had a previous history of biliary disease, no underlying pathology was identified as cholangitis was not apparent (normal bilirubin), no malignancy or any other intra-abdominal inflammation was detected and no recent surgery was performed on the patient, suggesting a probable cryptogenic disease. Antibodies against echinococcus and Entamoeba histolytica were twice negative (indirect fluorescent antibody test, IFAT) with four weeks interval (to avoid any initial false-negative results). Although symptoms and imaging suggested pyogenic abscesses, serology was twice repeated to exclude other abscesses etiology as there are neither diagnostic (but only highly suggestive) clinical nor radiological criteria for their differentiation. In addition, negative blood cultures and the patients refusal for surgical intervention complicated differential diagnosis. Serial ultrasounds and CT scans every two months revealed gradual reduction of abscesses size (less than 2 cm in the last examination, Fig. 2).
Discussion
Liver abscesses are more commonly pyogenic or amoebic. Pyogenic abscesses may be caused mainly by ascending biliary (gallstones, cholangitis and malignancies) or portal tract sepsis (diverticulitis, inflammatory bowel disease, intra-abdominal inflammation and malignancies) and in lesser degree by superinfection of cysts or necrotic tissue, trauma or hematogenous dissemination. Nevertheless, in many cases (up to 25% of patients) no underlying cause is found and the disease is defined as cryptogenic. The most common pathogens are Streptococcus species (29.5%), E. coli (18.1%), Staphylococcus species (10.5%) and Klebsiella (9.2%)1. E. coli is the most organism in abscesses of biliary or portal origin while Gram-positive cocci account for most cases of hematogenous or cryptogenic disease. Abscesses are usually present in elderly patients with history of diabetes and they are multiple in many cases. Jaundice, low albumin and pulmonary complications (pleural effusions) are common. In ultrasound they may appear as a cavity with thick or irregular borders and hypoechoic or hyperechoic content. They may be unilocular or with internal septa. In CT scan the fibrous tissue around the abscess is often a centimeter or thicker and gradually merges into the liver parenchyma. A common finding is the presence of air in the cavity. After intravenous contrast administration there is a faint, thin, rim enhancement and perilesional edema. Conservative treatment alone usually fails as mortality fluctuates between 45% and 95%, unless abscesses are solitary or small enough. Treatment should include antibiotics administration (usually cephalosporins or quinolones plus metronidazole and/or aminoglycosides) and simultaneous surgical intervention (aspiration and drainage seem equally effective and have substituted surgical resection except for serious cases with multiple abscesses and/or sepsis).2 Combined treatment shows encouraging results as overall mortality for multiple abscesses fluctuates from 0% to 22% in different series.3,4 Indications for surgical intervention are: age > 55 years, size≥5 cm, involvement of left or both lobes and duration of symptoms more than 7 days.5,6 Mortality is increased among elderly patients and those with co-morbidities, such as cirrhosis, chronic renal failure or malignancy.
Amoebic abscesses usually present as solitary lesions of the right lobe. Patients are younger, more acutely ill than with pyogenic abscesses and from high-prevalence areas. Serum antibodies may be negative in acute disease (but positive after 7-10 days) or false-positive if the patient had amebiasis in the past. In ultrasound they appear as round or oval lesions with hypoechoic content, thin wall and well-defined margins, in contrast to thick and ill-defined borders of pyogenic abscesses. In CT scan they appear as well-circumscribed lesions, encapsulated by thick Wall with intermediate density between abscess and adjacente parenchyma. Intravenous contrast administration depicts a characteristic thick enhancement (isodense or slightly hyperdense relative to hepatic parenchyma) with a peripheral zone of edema.7,8 The central abscess cavity may show multiple septa. Extrahepatic extension is relatively common and involvement of pleural cavity, pericardium and adjacent viscera has been reported. They respond promptly to metronidazole alone. Indications for drainage are: size≥8 cm, left lobe involvement, no response to antibiotics within 48-72 h or when liver failure is present, in pregnancy and when pleuro-pulmonary complications exist.9,10
Our patient had most of the typical features of pyogenic abscesses. She was elderly with no record of diarrheas, she had multiple cavities of left lobe exclusively, she did not respond promptly to therapeutic regimen for amebiasis and she had bilateral pleural and pericardial effusions. Abscesses were multi-located with irregular wall and illdefined margins. Contrast administration showed a thin, rim enhancement of abscesses walls, opposite of the thick, isodense one with peripheral edema that someone should expect for amoebic abscesses. Additionally, serum serology for E. histolytica was twice negative. Detection of antibodies using IFAT is probably the most reliable, rapid and easily reproducible test for diagnosis of amebic liver abscesses with 93.6% sensitivity and 96.7%, making it more sensitive even than ELISA test. It is also able to differentiate between past (treated) and present disease. A negative test therefore indicates that a patient never had invasive amebiasis.11 Additionally, an abdomen CT scan five years ago showed no focal abnormalities of left lobe excluding any possibility for superinfection of a previous cyst. This patient had all the indications for surgical intervention. Despite her refusal she managed to exceed all hopes and overcome this, almost lethal, situation with conservative treatment only.
References
1. Meddings L, Myers RP, Hubbard J, Shaheen AA, Laupland KB, Dixon E, et al. A population-based study of pyogenic liver abscesses in the United States: incidence, mortality and temporal trends. Am J Gastroenterol. 2010;105:117-24. [ Links ]
2. Liu CH, Gervais DA, Hahn PF, Arellano RS, Uppot RN, Mueller PR. Percutaneous hepatic abscess drainage: do multiple abscesses or multiloculated abscesses preclude drainage or affect outcome? J Vasc Interv Radiol. 2009;20:1059-65. [ Links ]
3. Chou FF, Sheen-Chen SM, Chen YS, Chen MC. Single and multiple pyogenic liver abscesses: clinical course, etiology and results of treatment. World J Surg. 1997;21:384-8. [ Links ]
4. Giorgio A, de Stefano G, Di Sarno A, Liorre G, Ferraioli G. Percutaneous needle aspiration of multiple pyogenic abscesses of the liver: 13-year single-center experience. AJR. 2006;187:1585-90. [ Links ]
5. Cerwenka H. Pyogenic liver abscess: differences in etiology and treatment in Southeast Asia and Central Europe. World J Gastroenterol. 2010;16:2458-62. [ Links ]
6. Khan R, Hamid S, Abid S, Jafri W, Abbas Z, Islam M, et al. Predictive factors for early aspiration in liver abscess. World J Gastroenterol. 2008;14:2089-93. [ Links ]
7. Radin DR, Ralls PW, Colletti PM, Halls JM. CT of amebic liver abscess. AJR. 1988;150:1297-301. [ Links ]
8. Mortelé KJ, Segatto E, Ros PR. The infected liver: radiologic---pathologic correlation. RG. 2004;24:937-55. [ Links ]
9. Salles JM, Moraes LA, Salles MC. Hepatic amebiasis. BJID. 2003;7:96-110. [ Links ]
10. Sharma N, Sharma A, Varma S, Lal A, Singh V. Amoebic liver abscess in the medical emergency of a North Indian hospital. BMC Res Notes. 2010;3:21-4. [ Links ]
11. Fotedar R, Stark D, Beebe N, Marriott D, Ellis J, Harkness. Laboratory diagnostic techniques for Entamoeba species. Clin Microbiol Rev. 2007;20:511-32. [ Links ]
Conflicts of interest
The authors have no conflicts of interest to declare.
*Corresponding author.
E-mail address: christosnina@hotmail.com (C.E. Lampropoulos).
Received 5 October 2011; accepted 5 October 2011













