Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Jornal Português de Gastrenterologia
versão impressa ISSN 0872-8178
J Port Gastrenterol. vol.19 no.3 Lisboa maio 2012
Esophageal melanocytosis
Melanocitose esofágica
Cláudia Cardosoa,∗, Ricardo Freirea, Élia Gamitoa, Carlos Quintanab, Isabelle Cremersa, Ana Paula Oliveiraa
a Serviço de Gastrenterologia, Centro Hospitalar de Setúbal, Setúbal, Portugal
b Serviço de Anatomia Patológica, Centro Hospitalar de Setúbal, Setúbal, Portugal
*Autor para correspondência
A 77-year-old woman was presented to our hospital with a six-month history of heartburn and chest pain. The upper gastrointestinal endoscopy revealed several dark flat irregularly delineated areas in the middle third of the esophagus (Fig. 1a and b). Histological examination of these lesions revealed an increased number of pigment-laden dendritic cells in the basal layer of the epithelium, with no celular atypia that stained positive with Masson-Fontana (Fig. 2), prompting the diagnosis of esophageal melanocytosis. This rare condition is characterized by melanocytic proliferation in the basal layer of esophageal squamous epithelium with an increased deposition of melanin. About 30 cases have been reported so far, the majority of which in Indian and Japanese populations.1,2 The etiology and pathogenesis remain uncertain, although it has been hypothesized that it may result from a chronic irritant stimulus, such as gastroesophageal reflux disease that causes mucosal damage and reactive keratinocytic and melanocytic hyperplasia. Overall, these lesions are more common in males and are located in the middle or lower third of esophagus. The possible association with primary esophageal melanoma awaits further investigation to determine whether there is a common pathogenesis or a coincidence of two rare entities in the same patient. Due to its rarity, no current recommendations regarding management and surveillance are available.3
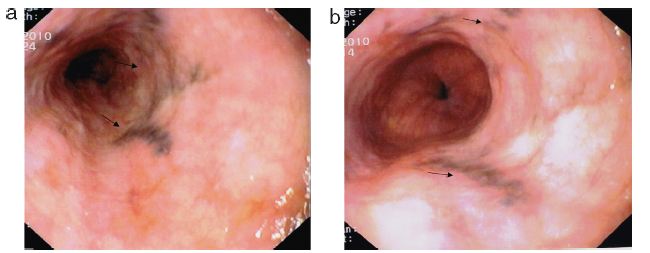
Figure 1 (a and b) Dark flat irregularly delineated areas in the middle third of the esophagus.

Figure 2 Pigment-laden dendritic cells in the basal layer of the epithelium that stained positive with Masson-Fontana.
References
1. Yamazaki K, Ohmori T, Kumagai Y. Ultrastructure of oesophageal melanocytosis. Virchows Arch A Pathol Anat Histopathol. 1991;418:515-22. [ Links ]
2. Sharma SS, Venkateswaran S, Chacko A. Melanosis of the esophagus. An endoscopic, histochemical and ultrastructural study. Gastroenterology. 1991;100:13-6. [ Links ]
3. Chang F, Deere H. Esophageal melanocytosis --- morphologic features and review of the literature. Arch Pathol Lab Med. 2006;130:552-7. [ Links ]
Conflicts of interest
The authors have no conflicts of interest to declare.
*Autor para correspondência
E-mail address: claudiamarcal@gmail.com (C. Cardoso).
Received 6 March 2011; accepted 23 June 2011













