Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Jornal Português de Gastrenterologia
versão impressa ISSN 0872-8178
J Port Gastrenterol. v.17 n.6 Lisboa nov. 2010
Sister Mary Joseph’s nodule
António Murinello1a, Ana Carvalho1b, João Freire2, A. Manuel Figueiredo1a, Marta Baptista1a, Helena Damásio1a, M. Jesus Murillo1b, Paulo Ribeiro1c, A. Raquel Martins1a
1Hospital de Curry Cabral, a)Unit of Internal Medicine 1; b)Unit of Histopathology; c)Unit of Gastroenterology; 2Instituto Português de Oncologia. Unit of Medical Oncology
Abstract
A religious nurse at Mayo Clinic, firstly noticed the relationship of umbilical metastatic nodes (Sister Mary Joseph’s nodule) with advanced inoperable intraabdominal malignancy (ovary, colon, stomach, pancreas, uterus), meaning an unfavourable prognosis. We present a patient with disseminated colonic neoplasm with umbilical metastasis, initially diagnosed as umbilical hernia. A review is performed of: umbilicus anatomy and its attachments containing remnants of fetal structures; its arterial, venous and lymphatic supply, helping to explain why umbilical metastasis occurs; sources of primary malignancy.
Clinical, radiological, cytological and histological aspects of the patient´s diagnosis are reviewed. Some patients may have better survival with aggressive surgery and adjunctive chemotherapy, but usually treatment is frequently palliative.
KEYWORDS: Sister Mary Joseph's nodule, colon cancer, umbilical metastasis.
Nódulo da Irmã Maria José
Resumo
Uma enfermeira religiosa (Clínica Mayo) descobriu a relação entre metástases umbilicais (nódulo da Irmã Maria José) e neoplasias malignas avançadas intra-abdominais, inoperáveis (ovário, cólon, estômago, pâncreas, útero). Os autores apresentam um doente com cancro do cólon disseminado e metástase umbilical, interpretada inicialmente como hérnia umbilical. Revêem-se: características anatómicas do umbigo, e sua relação com ligamentos do umbigo contendo estruturas embriológicas residuais; a sua rede vascular arterial, venosa e linfática, todos estes elementos importantes para a compreensão da forma de ocorrência de metástases umbilicais; neoplasias primitivas. Consideram-se aspectos do diagnóstico clínico, radiológico, citológico e histopatológico. Embora haja referências raras de melhor sobrevivência em alguns tumores, com terapêutica cirúrgica agressiva e quimioterapia adjuvante, o tratamento destes doentes é habitualmente tão só paliativo.
PALAVRAS CHAVE: Nódulo da Irmã Maria José, cancro do cólon, metástases umbilicais.
INTRODUCTION
Cutaneous metastases of malignant neoplasm are not common, occurring between 0.7 and 9 percent of autopsies1. Malignant metastases to the umbilicus, also known as Sister Mary Joseph’s nodule or node, and also called Sister Mary Joseph sign, are rare and represent only 10 percent of all secondary tumors to the skin. The first medical report of metastasis to the umbilicus due to visceral carcinomas was done by Walshe et al. in 1846. According to the Tanchov’s review of Walshe’s data, the author found only two cases of secondary umbilical involvement among 9118 cancer deaths that occurred in the period of 1830-18402. In 1864 Storer et al reported a complete case study of a metastatic umbilical nodule due to gastric adenocarcinoma. However, the association of umbilical tumor nodules and visceral carcinomas was firmly established only after the clinical observations of a religious nurse from the future Mayo Clinic.
Cutaneous metastasis are generally a sign of advanced malignant disease and portend a poor prognosis3-4. In several series there was an average survival of 10 months after the appearance of such lesion. It is usual to consider that the finding of a metastatic nodule at the umbilical site almost certainly establishes the inoperability of the patient. However, although uncommonly, the presence of a malignant umbilical tumor is not sufficient proof of the existence of widespread metastatic disease.
According to a review of the literature pre-dating modern radiological and pathologic methods, umbilical nodules could be due to a primary umbilical tumor in 38% of cases, endometriosis in 32% of individuals, and the remaining 30% are actually secondary deposits of tumors found in the gastrointestinal tract in 35% to 65% of patients (most often pancreatic tail and body, gastric or colon cancer), or in the genitourinary tract in 12% to 35% of cases (mostly ovarian but also uterine cancer).
It is estimated that 1% to 3% of the abdominal-pelvic malignancies metastasize to the umbilicus. In addition, about 3-6% of cases are due to hematological malignancies, lung or breast cancers. Other uncommon primary tumors reported include gallbladder, liver, small bowel, appendix, fallopian tube, penis, kidney, and prostate. Very rare causes of umbilical metastases are abdominal desmoplastic round cell tumor, malignant peritoneal mesothelioma, and melanoma3,5. Before the study possibilities of the modern radiologic techniques, the primary origin of the tumor was unknown in 15% to 30% of the cases1. It is important to have the clinical notion that an apparently insignificant umbilical nodule, may be the only manifestation of an underlying advanced malignant disease and therefore clinicians should be aware of such nodule6.
Sister Mary Joseph’s nodule usually present as a painful lump on the anterior abdominal wall, with different morphologic character:
a) inflammatory erythematous thickening of the overlying skin resembling cellulitis; b) vascular appearance; c) fissures or ulceration; d) imitating incarcerated umbilical hernia7.
It has irregular margins and a hard fibrous consistency. The surface may be ulcerated and necrotic, and may have a bloody, or a serous, or a purulent, or mucoid discharge coming out of it. The colour range is also wide and has been described as white, bluishviolet, or brownish-red. It is occasionally pruritic. The size of the nodule usually ranges from 0.5 to 2 cm, although some protruding nodules may reach up to 10 cm in size8-9.
Sister Mary Joseph (1856-1939) was born in Salamanca, New York as Julia Dempsy. Her parents were Irish immigrants.
In 1878, at age of 22, she joined the Third Order Regular of Saint Francis of the Congregation of Lady of Lourdes, taking the name of Sister Mary Joseph10. This religion mission was involved in the operation of St. Mary’s Hospital (built in 1889). She entered Saint Mary’s Hospital in Rochester, Minnesota, U.S.A., and after a 6-months training, she started to work with Dr. William Mayo, in the surgical wards of what would later be world renowned Mayo Clinic. Three years later (1892) she became his surgical assistant and nursing superintendent.
Dr. Mayo relied a great deal on her assistance and wisdom. Once, when asked a technical question regarding what he would do in a certain clinical circumstance, he replied, “I would consult Sister Joseph and follow her advice”. She could anticipate every act of Dr. Mayo during surgery and because she had very small hands, she could reach areas inaccessible to Dr. Mayo. She often incised the integument herself, before Dr. Mayo started the operation. Moreover, she also ended the operation by closing the wound. She was able to predict malignant findings at laparotomy if she felt an umbilical mass while scrubbing the abdomen during aseptic preparation for surgery11. Dr. Mayo first reported the condition as “pants-button umbilicus” (without credit to Sister Mary Joseph) in a lecture to the Cincinnati Academy of Medicine in 1928. The eponymous term “Sister Mary Joseph’s nodule” was proposed by Sir Hamilton Bailey in 1949 to accredit Dr. Mayo’s brilliant assistant12. Because Sister Mary Joseph later removed Mary of her name, the sign has also been referred to as Sister Joseph’s nodule. Sister Mary worked until her death at the age of 82 of bronchopneumonia. Before she died according to some reports, she noticed the presence of the nodule within her umbilicus.
CLINICAL REPORT
A 56-year-old white male, a retired soccer player and trainer, who had a pacemaker implanted 10 years ago due to complete atrium-ventricular block, was admitted in our Unit in October 2008 for workup of a suspected malignancy. The patient claimed that for the past two years his stools were alternately solid and diarrheic, and had intermittent hematochezia. There was no medical consultation done during that time. During the previous year he noticed a slowing progressive enlargement of the umbilical area, sometimes with inflamed appearance and rarely with oozing, that was considered to be due to herniation.
Three months prior to admission, the patient experienced anorexia and 10% weight loss. A month prior to admission he was having low back pains and just before admission the patient complained of early satiety and a mild left testicular pain. He denied fever or constipation.
On physical examination, the patient appeared in good nutritional state. There was no pallor, jaundice, cyanosis or peripheral edema. No lymphadenopathy was detected. The exam of the neck was normal, and the lung and heart exam also did not reveal abnormalities. In the abdomen there was an oozing ulcerated nodular lesion measuring 6.5 cm x 5.5 cm (suspected to be a Sister Mary Joseph’s nodule) observed at the umbilical region (Fig. 1). The nodule has an irregular surface, was hard and slightly tender on palpation, and there was no hepatomegaly and no splenomegaly on abdominal palpation.
Rectal exam revealed a soft, enlarged prostate.

Fig. 1. Sister Mary Joseph’s nodule: oozing ulcerated nodular tumor lesion of the umbilicus.
A day before admission the patient underwent a CT scan of the thorax, abdomen and pelvis which demonstrated generalized lymphadenopathy with involvement of the supra-clavicular, axillary, mediastinial, lumbar-aortic, celiac, mesenteric, inguinal and retrocrural territories; secondary micronodular pulmonary deposits; infiltration of the great omentum, moderately voluminous non-pure ascites; nodular lesion of the left adrenal; slightly diffusely heterogenic liver. The CT scan findings on the liver did not favor liver neoplasm infiltration. The umbilical area was interpreted as an empty umbilical hernia, but on review we diagnosed a nodular umbilical tumor (Fig. 2).
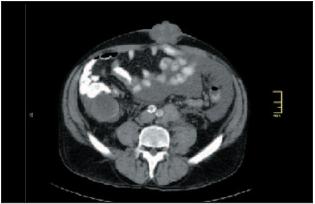
Fig. 2. CT scan of the abdomen: nodular tumor lesion within a hernia of the umbilicus.
Relevant laboratory tests at admission showed: normal CBC, normal levels of serum albumin, PSA, glucose, BUN and creatinine, normal thyroid function tests, normal serum protein electrophoresis; slightly low serum transferrin level; slightly elevated serum levels of [1]-GT and of LDH; elevated levels of CEA: 137.7 ng/ml (N < 5.0), CA 19.9 219.3 U/ml (N < 37.0), hCG 30.6 mUI/ml (N < 2.7), and very high levels of fetoprotein 10.878 ng/ml (N < 10.0) . A testicular ultrasound showed no mass, only a small bilateral hydrocele and a small left varicocele. A CT scan of the lumbar spine did not reveal any spinal metastasis. Cytology of a left supra-clavicular lymphadenopathy (Fig 3A) and of the umbilical nodule (Fig. 3B) showed secondary deposits of an adenocarcinoma. Colonoscopy was done and revealed (at 30 cm level) the presence of: 1) an ulcerated exophytic mass 40 mm wide (Fig. 4), which histology demonstrated a moderately differentiated adenocarcinoma (Fig. 5). 2) Two polyps that were removed by polypectomy revealing a tubulovillous adenoma and a tubular adenoma, both with low-grade dysplasia on histopathologic exam. The patient was transferred to the Medical Oncology Unit of the Portuguese Institute of Oncology in Lisbon (IPOL).
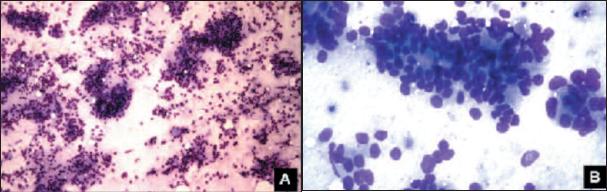
Fig. 3. Cytology: epithelial cells with obvious glandular arrangement consistent with secondary adenocarcinoma: A) Lymphadenopathy – Giemsa 100x; B) Umbilical nodule – Giemsa 400x.

Fig. 4. Colonoscopy: Exophytic tumor growth at 30 cm.
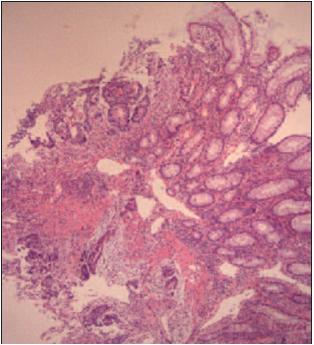
Fig. 5. Colon biopsy: HE 40x – Moderately differentiated adenocarcinoma
A diagnosis of stage IV colon cancer was made. Since the patient was symptomatic, he was started on chemotherapy. The pacemaker posed a relative contraindication to the placement of a central venous line for 5-fluoruracil infusion, so he was instead given a combination treatment of capecitabine and oxiplatin.
He was submitted to four cycles of therapy.
For the increasing lumbar pain, a bone scan was performed which showed heterogenous fixation on the lumbar vertebrae. A repeat CT scan of the lumbar spine was also done, revealing a pathological fracture of the 2nd lumbar (L2) vertebral body.
There was an osteolytic lesion with a soft tissue component that merged with the large retroperitoneal lymphadenopathies.
Palliative radiotherapy was given (30 Gy in 10 fractions), including L2 and nearby lymphadenopathies. In March 2009 the patient was brought to the emergency room of the IPOL with pain, nausea and vomiting. Chemotherapy was stopped, considering the side effects and the disease progression, supportive treatment was given and analgesic medication was switched to transdermal opioids. Two weeks later he was admitted on IPOL with delirium, dehydration and pneumonia. He died the next day.
DISCUSSION
To better understand the occurrence of umbilicus metastasis it is important to remember certain aspects of the umbilical anatomy13: a) the sheath of both rectus abdominis muscles which is formed by the fusion of the aponeuroses of the external oblique, internal oblique and transversus abdominis muscle; b) the linea alba formed by the midline fusion of the sheaths of both rectus muscles, extending from the xiphoid process to the symphysis pubis; c) the umbilicus consists of a puckered scar through the linea alba at the former attachment of the umbilical cord. The umbilical ring is a scar invaginated on the abdominal wall between the transversalis fascia and peritoneum ring; d) the fascia transversalis lying deep to the linea alba and just superficial to the peritoneum. The umbilical ring is in fact a scar invaginated on the abdominal wall between the fascia transversalis and peritoneum; e) the fascia umbilicalis is a thickening of the fascia transversalis, which support the floor of the umbilicus.
There are several ligaments, or peritoneal folds, consistently found in adults that connect with the umbilicus and that contain remnants of the obliterated fetal structures such as: a) the median umbilical ligament, or urachus, is the obliterated allantois, which formerly connected the umbilicus to the bladder; b) the medial umbilical ligaments represent the obliterated umbilical arteries; c) the ligamentum teres, the most inferior part of the falciform ligament, contains the obliterated umbilical vein; d) an additional ligament connecting the umbilicus to the ileum is sometimes present and represents an obliterated remnant of the vitelline duct, which connect the yolk sac to the midgut13.
The vascular supply to the anterior abdominal wall including the periumbilical region includes: a) the main arteries – the inferior epigastric and deep circumflex iliac (branches of the external iliac artery) and the superior epigastric (a branch of the internal thoracic artery); b) venous drainage – into a network of veins radiating from the umbilicus to the axillary vein above via the lateral thoracic vein and the femoral vein below via the superficial epigastric vein. Small paraumbilical veins connect with the portal system along the ligamentum teres; c) the superficial lymphatic drainage of the periumbilical region connects with the axillary nodes above and the inguinal nodes below. Deep lymphatic drainage is via the internal thoracic, external iliac and abdominal paraaortic nodes13.
Metastasis to the umbilicus can occur in several ways: 1) contiguous spread of peritoneal cancer to the anterior surface of the abdominal cavity, probably the most frequent method7; 2) hematogenous spread through the arterial and venous systems (connections of the umbilical veins with the portal system and with the caval vein system; 3) lymphatic spread via the four sets of lymphatic pass from the umbilical region where there are connections with axillary, inguinal and periaortic lymph nodes; 4) direct extension along the ligaments of embryonic origin (round ligament of the liver, the urachus, the vittelointestinal duct remnant, and the obliterated vitelline artery), that connect with the umbilicus and contain remnants of the obliterated fetal structures7,13.
All the connections with multiple embryonic remnants and the extensive vascular and lymphatic communications, and the proximity of the umbilical scar to the anterior peritoneal surface, help to understand the source of metastasis to the umbilicus mostly from the abdomen and pelvis, but also from the thorax14. Therefore, theoretically, all types of cancer may disseminate to the umbilical region, but the most prevalent primary sites are from intra-abdominal origin.
Patients with Sister Mary Joseph’s nodule may complain of a number of clinical symptoms consistent with intra-abdominal cancer, including epigastric pain, abdominal distention, weight loss, nausea and ascites. The signs of umbilical nodules metastasis are generally evident on physical examination, but they are sometimes overlooked in obese patients. A radiologist can be the first to diagnose an umbilical nodule, owing to the large number of cross-sectional imaging studies performed in patients suspected to suffer from malignancy. Whatever the source of umbilical metastasis, the Sister Mary Joseph’s nodule may occur as a dermal, subcutaneous or peritoneal deposit, and this can be easily demonstrated in ultrasound and in contrasted computerized tomography13.
Differential diagnosis of umbilical metastasis of tumors should include umbilical hernia, cutaneous endometriosis, benign tumors such as foreign body granuloma, melanocytic
nevi, papilloma, cutaneous epithelial inclusion cysts, keloid, myxoma, and primary umbilical malignancy, including melanoma, squamous and basal cell carcinoma, and sarcoma.
After excluding umbilical hernia, the diagnosis of umbilical nodules should be obtained by fine needle aspiration for cytological examination which is easy to perform, if necessary with ultrasound guidance15. A skin biopsy for histopathological examination can best define the type of the tumor. The hematoxylin-eosin stain may differentiate primary and metastatic tumors. Moreover, immunohistochemical analysis may define the cellular origin in 72% of cases of unknown primary tumor. The use of electron microscopy and cytogenetic analysis may enhance the diagnostic sensitivity and specificity of the diagnosis. These methods enable the clinician to obtain a correct diagnosis of the situation without exposing the patient to time-consuming, invasive, expensive and useless diagnostic procedures.
With this information the physician can best decide what will be the best way to search for the primary tumor.
As Sister Mary Joseph’s nodule usually means the presence of widespread metastasis, the treatment of these patients commonly is only palliative. However, some authors postulate that depending somewhat of the type of tumor and of it primary origin, some patients can have better survival when treated aggressively with both surgery and adjunctive therapy1. Nevertheless the appropriateness of such therapy is determined by the clinical state of the patient. Despite the advanced stage of the disease in our patient, his good performance index was in favour of trying to improve palliation and perhaps obtain a longer survival time with chemotherapy. Unfortunately the disease was shown to be unresponsive to the chemotherapeutic regimen used, and the patient condition rapidly deteriorated, not allowing further treatments.
REFERENCES
1. Gabriele R, Borghese M, Conte M, et al. Sister Mary Joseph’s nodule as a first sign of cancer of the caecum. Report of a case. Dis Colon Rectum 2004;7:115-117.
2. Shetty MR. Metastatic tumors of the umbilicus: a review 1830-1989. J Surg Oncol 1990;45:56-58. [ Links ]
3. Sariya D, Ruth K, Adams-McDonnell R, et al. Clinicopathologic correlation of cutaneous metastases. Experience from a Cancer Center. Arch Dermatol 2007;143:613-620.
4. Crescentini F, Deutsch F, Sobrado CW, et al. Umbilical mass as the sole presenting symptom of pancreatic cancer: a case report. Rev Hosp Clin Fac Med S. Paulo 2004;59:198-202.
5. Abdulqawi R, Ahmad S, Ashawesh K. A rare cause of Sister Mary Joseph’s nodule. Swiss Med Wkly 2007;137:559-560.
6. Aich RK, Karim R, Chakraborty B, et al. Sister Mary Joseph´s nodule. Indian J Med & Pediatr Oncol 2008;29:40-43.
7. Powell FC, Cooper AJ, Massa MC, et al. Sister Mary Joseph’s nodule: a clinical and histological study. J Am Acad Dermatol 1984;10:610-615.
8. Raymond PL. The umbiliquitous umbilicus. What it can reveal about intra abdominal disease. Postgrad Medicine 1990;87:175-176, 179-181.
9. Urbano FL. Sister Joseph’s nodule – Review of Clinical Signs, Hosp Physician 2001;44:33-36.
10. Hill M, O’Leary JP. Vignettes in medical history. Sister Mary Joseph and her node. Am Surg 1996;62:328-329.
11. Limmathurotsakul D, Rerknimitr P, Korkij W, et al. Metastatic mucinous cystic adenocarcinoma of the pancreas presenting as Sister Mary Joseph’s nodule. JOP. J Pancreas 2007;8:344-349.
12. Bailey H. Demonstrations of Physical Signs in Clinical Surgery. 11th ed. Baltimore, USA. Williams & Wilkins, 1949.
13. Coll DM, Meyer JM, Mader M, et al. Imaging appearances of Sister Mary Joseph nodule. Brit J Radiol 1999;72:1230-1233.
14. Gabriele R, Conte M, Egidi F, et al. Umbilical metastases: current viewpoint. World J Surg Oncol 2005;3:13-15.
15. Edoute Y, Malberger E, Kuten A. Umbilical metastasis diagnosed by fine needle aspiration. J Surg Oncol 1990;45:56-58.
António Murinello; Avª Engº António Azevedo Coutinho, lote 8 r/c dto,
2750-644 Cascais; Portugal;
Telemóvel: +351 918 626 874;
E-mail: amurinello@gmail.com
Recebido para Publicação: 17/07/2009 e Aceite para Publicação: 06/08/2010.













