Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Nascer e Crescer
versão impressa ISSN 0872-0754versão On-line ISSN 2183-9417
Nascer e Crescer vol.28 no.2 Porto jun. 2019
https://doi.org/10.25753/BirthGrowthMJ.v28.i2.14909
CASE REPORTS | CASOS CLÍNICOS
Persistent omphalomesenteric duct: a rare cause of acute intestinal volvulus in an adolescent treated by laparoscopy
Persistência do ducto onfalomesentérico: uma causa rara de vólvulo intestinal num adolescente tratado por laparoscopia
Maria Miguel GomesI, Catarina Magalhães FariaI, Manuela Costa AlvesI, Ana Raquel SilvaII,III,IV, Jorge Correia-PintoII,III,IV, Angélica OsórioII,III,IV
I Department of Pediatrics, Hospital de Braga. 4710-243 Braga, Portugal. mariamgomes@hotmail.com; catmagalhaesfaria@gmail.com; manuelacostaalves@gmail.com
II Department of Pediatric Surgery, Hospital de Braga, 4710-243 Braga, Portugal. araquelosilva6@gmail.com; jcp@med.uminho.pt; angelicosorio@gmail.com
III Life and Health Sciences Research Institute (ICVS). 4710-057 Braga, Portugal. araquelosilva6@gmail.com; jcp@med.uminho.pt; angelicosorio@gmail.com
IV School of Health Sciences, University of Minho and Portugal Government Associate Laboratory ICVS/ 3B’s. 4710-057 Braga, Portugal. araquelosilva6@gmail.com; jcp@med.uminho.pt; angelicosorio@gmail.com
Endereço para correspondência | Dirección para correspondencia | Correspondence
ABSTRACT
This report describes the case of a 14-year-old male with a prior history of recurrent abdominal pain and two previous sub-occlusive episodes. He presented at the Emergency Room with abdominal pain, emesis, abdominal distension, painful palpation, and signs of peritoneal irritation. Plain upright abdominal radiography suggested a distal small bowel obstruction. Exploratory laparoscopy showed a tubular structure connecting the antimesenteric border of the terminal ileum and the umbilicus, which was behaving as a rotation axis to the small intestine. The volvulus was laparoscopically de-rotated, and the structure was excised. Histological exam confirmed the diagnosis of persistent omphalomesenteric duct.
This case illustrates an intestinal obstruction caused by small intestine volvulus. A high index of suspicion is required to acknowledge this etiology.
Keywords: omphalomesenteric duct; vitelline duct; laparoscopy; small intestinal obstruction; volvulus
RESUMO
É descrito o caso de um adolescente masculino de 14 anos de idade com antecedentes de dor abdominal recorrente e dois episódios sub- oclusivos prévios. Recorreu às urgências com dor abdominal e vómitos. Ao exame objetivo, era evidente distensão abdominal e sinais de irritação peritoneal. A radiografia abdominal simples de pé sugeriu a presença de obstrução do íleo distal. Foi realizada uma laparoscopia exploratória, que evidenciou uma estrutura tubular a ligar o bordo antimesentérico do íleo terminal ao umbigo e se comportava como eixo de rotação. Foi efetuada de-rotação do vólvulo e excisão da estrutura. O exame histológico confirmou o diagnóstico de ducto onfalomesentérico persistente.
O presente caso ilustra uma obstrução intestinal causada por vólvulo do íleo distal, sendo necessário um alto índice de suspeição para reconhecer esta etiologia.
Palavras-chave: ducto onfalomesentérico; ducto vitelino; laparoscopia; obstrução ileal; vólvulo
Introduction
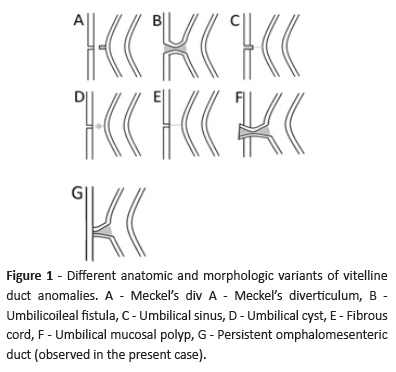
During embryonal development, the omphalomesenteric duct (OMD) behaves as a primitive connection between the midgut and the yolk sac.1,2 The OMD undergoes obliteration and reabsorbs spontaneously between the fifth and ninth weeks of gestation.1,2 Failure of closure or reabsorption occurs in 2% of the population.1-3 Different anatomic and morphologic variants of OMD anomalies exist (Figure 1): Meckel’s diverticulum, umbilicoileal fistula (patent OMD throughout its length), umbilical sinus (OMD remains open only at its outer portion), umbilical cyst (central cystic dilatation in which the OMD is closed at both ends but patent in the center), fibrous cord (complete obliteration of the duct connecting the ileum to the umbilicus), or umbilical mucosal polyp (persistence of OMD distal end).1,3 Meckel´s diverticulum is the most common variant, accounting for 65% of cases. Other variants are extremely rare.3 The affected population can remain asymptomatic until advanced ages.1-4 Symptoms are age-dependent and most usually manifest before the age of four (mainly in the neonatal period).1-4 Frequency of these entities is similar in both genders, but frequency of symptoms is higher in males.2 Symptoms include umbilical changes, gastrointestinal obstruction, abdominal pain, and gastrointestinal bleeding, with surgical excision being the treatment of choice.1-4
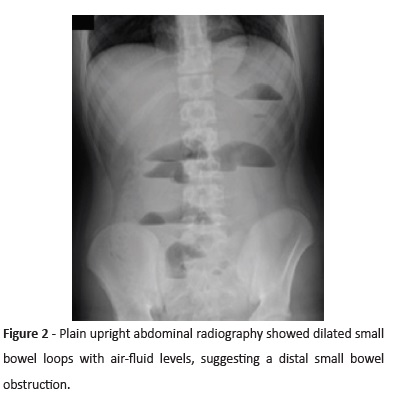
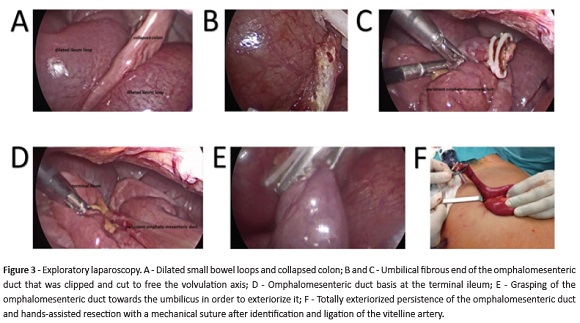
treatment but required hospitalization, and no previous history of abdominal surgery. No family history of gastrointestinal or other diseases was reported. The boy presented at the Emergency Room with a four-hour history of cramping abdominal pain and emesis (initially bilious emesis but later coffee-ground material), and no further complaints. Intestinal transit was present but decreased. He denied prior trauma and drug or toxic consumption. On examination, abdominal distension, decreased bowel sounds with normal tone, diffuse painful palpation, and mild signs of peritoneal irritation were noted. The remaining physical examination was unremarkable. Plain upright abdominal radiography revealed dilated small bowel loops with air-fluid levels, suggesting a small bowel obstruction (Figure 2). The boy started oral intake restriction and a nasogastric tube drain was placed. Laboratory tests revealed mild leukocytosis (23.9 x 103/µL leukocytes, with 19.9 x 103/µL neutrophils) and negative C-Reactive Protein (<2.90 mg/L). Digestive endoscopy identified no hemorrhagic injury or other changes. An exploratory laparoscopy was performed, which revealed distension of small intestine loops but no macroscopic signs of ischemia. Cecum was normally placed in the lower right quadrant and the colon loops were collapsed. A tubular structure with macroscopic appearance, similar to the small intestine (not just a fibrotic band), was found connecting the antimesenteric border of the terminal ileum to the umbilicus, which was behaving as a rotation axis for the small intestine (Figure 3). The umbilical border was ligated with 2 XL hemolocks, and the volvulus laparoscopically de-rotated. The structure was brought extracelomically and resected with a GIA 55 after ligation of the vitelin artery. Histological examination confirmed the diagnosis of persistent OMD. The post-operative period was uneventful, and the boy was successfully discharged on the fifth postoperative day. He remained asymptomatic over a six-month follow-up period.
Case report
Here in is reported the case of a 14-year-old male with prior history of recurrent abdominal pain, constipation, and overweight, who was undergoing a dietary plan, with regular exercise and daily laxative intake. He had two sub-occlusive episodes of unknown etiology in the previous three years, which resolved after conservative
Discussion
Mechanical obstruction is the most frequent surgical problem of the small intestine.5,6 Intra-abdominal adhesions related to previous abdominal surgery account for up to 75% of cases.5,6 Less prevalent etiologies include hernias, gallstones, neoplasms, intestinal malrotation disorders, or inflammatory pathologies such as tuberculosis or Crohn´s disease.5,6 In this case, as there was no history of prior surgery, intra-abdominal post-operative adhesions were rejected as a possible etiology. Presence of two previous episodes of intestinal sub-occlusion and the fact that the patient was followed for recurrent abdominal pain, overweight, and constipation (which was resistant to treatment with symptomatic measures) led to an initial unremarkable investigation comprising laboratory tests, radiographic contrast study, and abdominal ultrasonography.
The initial intestinal obstruction therapy is standard and etiology- independent. Analgesics, oral intake restriction, fluids, electrolyte replacement, and nasogastric drainage are important aspects of supportive care. Broad-spectrum antibiotics may be administered due to risk of bacterial translocation or as prophylaxis for possible resection. This patient followed the initially recommended supportive care and received empirical antibiotics.
Three mechanisms of intestinal obstruction caused by persistent OMD have been reported: intussusception, volvulus, and hernia.7-12 The present case illustrates an intestinal obstruction caused by small intestine volvulus. Surgery must be performed early due to risk of strangulation and intestinal perforation and loss. Etiology recognition is difficult without performing exploratory surgery and a high index of suspicion is required.
Clinical presentation is age-dependent and unspecific. Possible symptoms include irritability, umbilical discharge, umbilical hernia, emesis, abdominal pain, gastrointestinal bleeding, and absence of intestinal transit. Initial laboratory tests may be normal or show elevated inflammatory parameters. Abdominal radiography and ultrasonography are unspecific. Abdominal computed tomography may occasionally evidence the presence of a fibrotic band connecting the umbilicus to the small intestine. In this case, an abdominal computed tomography was not performed because the patient presented with an acute abdomen and such exam would delay treatment. Diagnosis was only possible through surgical exploration. Surgical excision of the vitelline duct anomaly is considered therapeutic.
Intestinal obstruction by persistent OMD is extremely rare.7-9,13 Early surgical resection by laparotomy is performed in symptomatic patients in most cases described in the literature.
Laparoscopy is associated with several technical difficulties, mainly due to bowel distension. Presence of a structure connected to the umbilicus may pose some problems when using the umbilicus as a working channel for laparoscopic instruments. Nevertheless, we consider that laparoscopy should be the preferred choice for approaching these patients due to the advantages of a minimally invasive surgery, including reduced pain and infectious complications, early recovery, and better cosmetic results.
REFERENCES
1. Vane DW, West KW, Grosfeld JL. Vitelline duct anomalies: experience with 217 childhood cases. Archives of Surgery 1987; 122:542-7. [ Links ]
2. Moore TC. Omphalomesenteric duct malformations. Semin Pediatr Surg 1996; 5:116-23. [ Links ]
3. Gluecklich B. Johann Friedrich Meckel, the younger (1781-1833). The American Journal of Surgery 1976; 132:384-6. [ Links ]
4. Durakbasa CU, Okur H, Mutus HM, Bas A, Ozen MA, Sehiralti V, et al. Symptomatic omphalomesenteric duct remnants in children. Pediatrics International 2010; 52:480-4. [ Links ]
5. Miller G, Boman J, Shrier I, Gordon PH. Etiology of smallbowel obstruction. Am J Surg 2000; 180:33-6. [ Links ]
6. Sarraf-Yazdi S, Shapiro ML. Small bowel obstruction: the eternal dilemma of when to intervene. Scand J Surg 2010; 99:78-80. [ Links ]
7. Herman M, Gryspeerdt S, Kerckhove D, Matthijs I, Lefere P. Small bowel obstruction due to a persistent omphalomesenteric duct. JBR-BTR2005; 88:175-7. [ Links ]
8. Bueno Lledó J, Serralta Serra A, Planeéis Roig M, Dobón Giménez F, Ibáñez Palacín F, Rodero Rodero R. Intestinal obstruction caused by omphalomesenteric duct remnant: usefulness of laparoscopy. Rev Esp Enferm Dig 2003; 95:736-8. [ Links ]
9. Amendolara M, Pasquale S, Perri S, Carpentieri L, Errante D, Biasiato R. Intestinal occlusion caused by persistent omphalomesenteric duct and Meckel’s diverticulum: report of 2 cases. Chir Ital 2003; 55:591-5.
10. Schillings GJ. Strangulation ileus caused by a not completely obliterated omphaloenteric duct in a 32-year-old patient. Zentralbl Chir 1987; 112:383-6. [ Links ]
11. Bedard CK, Ramirez A, Holsinger D. Ascending colon volvulus due to a vitelline duct remnant in an elderly patient. Am J Gastroenterol 1979; 71:617-20. [ Links ]
12. 1Gumport SL, Aronson SG. Acute intestinal obstruction secondary to Meckel’s diverticulum with persistent obliterated omphalomesenteric duct. Am J Surg 1959; 97:225-8.
13. Markogiannakis H, Theodorou D, Toutouzas KG, Drimousis P, Panoussopoulos SG, Katsaragakis S. Persistent omphalomesenteric duct causing small bowel obstruction in an adult. World J Gastroenterol 2007; 13:2258-60. [ Links ]
Endereço para correspondência | Dirección para correspondencia | Correspondence
Maria Miguel Gomes Department of Pediatrics, Hospital de Braga
Sete Fontes 4710-243 São Victor, Braga
Email: mariamgomes@hotmail.com
Received for publication: 22.10.2017
Accepted in revised form: 19.12.2018