Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Nascer e Crescer
versão impressa ISSN 0872-0754versão On-line ISSN 2183-9417
Nascer e Crescer vol.28 no.1 Porto mar. 2019
https://doi.org/10.25753/BirthGrowthMJ.v28.i1.13536
CASE REPORTS | CASOS CLÍNICOS
Ureteropelvic junction obstruction: three clinical cases with first symptoms during adolescence
Síndrome de junção ureteropélvica: três casos clínicos com início dos sintomas na adolescência
Mariana AbreuI, Alexandra PintoII, Cláudia AguiarI, Ribeiro de CastroIII, Célia MadalenaIV
I Pediatrics Department, Centro Materno Pediátrico, Centro Hospitalar Universitário de São João. 4200-319 Porto, Portugal. marianacgabreu@gmail.com; claudiaccmaguiar@gmail.com
II Pediatrics Department, Centro Hospitalar Lisboa Norte. 1649-035 Lisboa, Portugal. alexandra.r.pinto@gmail.com
III Urology Department, Centro Hospitalar Universitário do Porto. 4099-001 Lisboa, Portugal. luis.joao.castro@gmail.com
IV Pediatrics Department, Centro Hospitalar Póvoa de Varzim - Vila do Conde. 4490-421 Póvoa de Varzim, Portugal. celia.madalena@hotmail.com
Endereço para correspondência | Dirección para correspondencia | Correspondence
ABSTRACT
Ureteropelvic junction obstruction (UPJO) is defined as urine flow blockage occurring where the ureter enters the kidney and is presented as urinary tract dilatation (UTD), formerly named hydronephrosis. The condition may be congenital or acquired. Most UTD are diagnosed by antenatal ultrasonography, but some cases present later. In adolescence, clinical manifestations include intermittent flank or abdominal pain, hematuria, nephrolithiasis, urinary tract infection, deterioration of renal function, or arterial hypertension. The imaging modality of choice to diagnose UTD is ultrasonography (US). A diuretic renography will allow to identify UPJO. Treatment goals are to prevent renal function deterioration and relieve symptoms. Although conservative treatment measures are favored, some patients require surgical correction (pyeloplasty).
Three clinical cases with first symptom onset during adolescence are presented. The first case is a 14-year-old boy with abdominal pain suspected to correspond to acute appendicitis; the second case is a healthy 15-year-old female which presented with dysuria and lumbar pain; the third case is a 15-year-old female with prenatal diagnosis of left ureteropelvic dilation but no further medical problems, with left lumbar pain, dysuria, and fever.
Conclusion: A high degree of suspicion is required to include UPJO in the differential diagnosis of flank or back pain in adolescents.
Keywords: adolescence; hydronephrosis; ureteral obstruction
RESUMO
A Síndrome de Junção Ureteropélvica (SJUP) é definida como obstrução ao fluxo de urina na transição entre a pelve renal e o ureter e manifesta-se por dilatação do trato urinário (DTU), anteriormente designada hidronefrose. Esta condição pode ser congénita ou adquirida. A maioria dos casos de DTU são diagnosticados na ecografia pré-natal, mas alguns casos são detetados mais tarde. Na adolescência, as manifestações clínicas incluem dor abdominal ou lombar intermitente, hematúria, nefrolitíase, infeção do trato urinário, deterioração da função renal ou hipertensão arterial. O exame de imagem de escolha para diagnosticar DTU é a ecografia. O renograma permite identificar os casos de SJUP. Os objetivos do tratamento são prevenir a deterioração da função renal e controlar os sintomas. O tratamento conservador é prioritário, mas pode ser necessária correção cirúrgica (pieloplastia). São apresentados três casos clínicos com apresentação dos primeiros sintomas de doença na adolescência. O primeiro caso refere-se a um adolescente de 14 anos com dor abdominal inicialmente interpretada como apendicite aguda; o segundo, a uma adolescente saudável de 15 anos com queixas de disúria e dor lombar; e o terceiro, a uma adolescente de 15 anos saudável, com diagnóstico pré-natal de dilatação uretero-pélvica esquerda, sem outros antecedentes de relevo, com dor lombar à esquerda, disúria e febre.
Conclusão: É necessário um alto grau de suspeição para incluir a SJUP no diagnóstico diferencial da dor lombar e/ou abdominal em adolescentes.
Palavras-chave: adolescência; hidronefrose; obstrução ureteral
Introduction
Ureteropelvic junction obstruction (UPJO) is defined as partial or total blockage of urine flow where the ureter enters the kidney.1,2 It is presented as renal pelvis and calyceal dilatation without obvious dilatation of the ureter.3,4 UPJO is the most common pathologic cause of antenatally detected urinary tract dilatation (UTD).1,2 It occurs sporadically in 1:500-1500 live births and is more prevalent in boys, with a male:female ratio of 2:1.1,5-7 The left side is affected in approximately two thirds of cases and both sides in 10-40%.2,5,7 The condition may be congenital or acquired and causes can be intrinsic (more frequent and including scarring of ureteric valves and ureteric hypoplasia) or extrinsic (an aberrant or accessory renal artery may cross the lower pole of the kidney, causing an impingement on the ureter and blockage of urinary flow, congenital abnormalities of the kidney, scar formation secondary to ureteric manipulation by surgery, or fibroepithelial polyps).1,5-7
Most UTDs are diagnosed by antenatal ultrasonography (US), but they may also present later in childhood.1,6-9 In older children, clinical manifestations include intermittent flank or abdominal pain, especially with brisk diuresis (for example, after consumption of caffeine or alcohol), renal injury after experiencing minor trauma, hematuria, nephrolithiasis, urinary tract infection (UTI), deterioration of renal function, or arterial hypertension.2,5,6 Unless there is coincident vesicoureteral reflux (VUR), UTI is a rare entity.1
Although US is the imaging modality of choice to diagnose UTD, this technique is unable to differentiate between obstructed and non- obstructed kidneys. For this purpose, a diuretic renography − usually with 99mTc-mercaptoacetyltriglycine-3 (MAG-3) − is essential, as it allows to distinguish between an obstructed and a dilated but otherwise normal renal pelvis.1,2,5,7,8 Occasionally, a voiding cystourethrogram has to be performed to rule out VUR.1,2,7,10
The goals of treatment are to prevent deterioration of renal function and relieve symptoms (if present). Conservative treatment measures (as antibiotic prophylaxis, in cases of previous symptomatic UTI and until VUR has been excluded) are priority.11 Surgical correction is
required when renal function is decreased (differential renal function of obstructed kidney <40%) or if the patient became symptomatic.5 If surgery is indicated, pyeloplasty is the gold-standard treatment.1,5 Three clinical cases are reported with first symptoms of disease manifesting during adolescence.
Case 1
Young, previously healthy, 14-year-old male admitted to the Emergency Department with acute onset abdominal pain in the right flank and lower quadrant with 24 hours of evolution, without fever. The boy had one episode of flank pain four years before, with spontaneous resolution. On physical examination, he weighted 84 Kg (over the 95 percentile for age) and his abdomen was tender in the right lower quadrants, without further remarkable findings. Laboratory evaluation revealed white blood cell (WBC) count of 7.56x103/μL with 58.8% neutrophils, C-reactive protein (CRP) of
10.4 mg/dL (normal: <0.5 mg/dL), blood urea of 16.4 mg/dL, serum creatinine of 0.64 mg/dL, and electrolytes within the normal range. Urinalysis by microscopy showed 2−5 red blood cells per high-power field (HPF), with no other abnormalities. Abdominal radiography was normal. At this point, acute appendicitis was suspected by the surgical team. During surgery, a retroperitoneal mass was found in the right kidney.
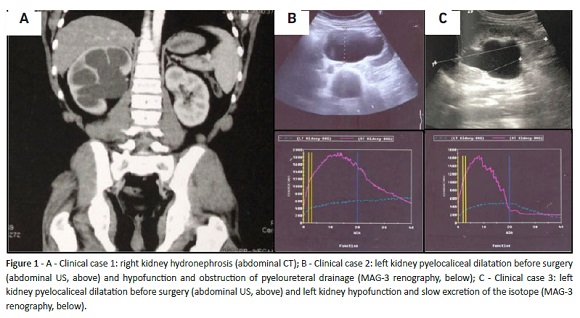
An abdominal computed tomography (CT) scan was performed, showing dilatation of the renal pelvis and suggesting UPJO (Fig. 1A). In renal US, an enlarged right kidney was observed, with parenchyma confined to an echogenic blade of 5 mm and anteroposterior renal pelvis diameter (APRPD) of 40 mm. MAG-3 renography revealed pyeloureteral obstruction and slightly decreased (44%) differential function of the right kidney. The patient was submitted to pyeloplasty. On follow-up, right kidney APRPD was 35 mm in US, and two years later MAG-3 renography revealed differential function improvement (48.5%). After five years, the patient remains well, with no symptoms.
Case 2
A young, healthy 15-year-old female presented to the Emergency Department with dysuria and left lumbar pain, with no fever. Physical findings included tenderness on palpation of the left flank, with the remaining examination unremarkable. Laboratory findings comprised WBC count of 15.65x103/μL with 88.6% neutrophils, CRP of 7.9 mg/dL, blood urea of 17.4 mg/dL, serum creatinine of 0.72 mg/dL, and electrolytes within the normal range. Urinalysis by microscopy revealed > 50 white blood cells per HPF, without further abnormalities, and urine culture presented > 105 colony-forming units (CFU) per milliliter of Escherichia coli, confirming the diagnosis of febrile UTI. At further evaluation, renal US showed pyelocaliceal dilation of the left kidney, with 42mm APRPD and reduced left renal parenchyma. MAG-3 renography showed hypofunction of the left kidney (24.91%) and pyeloureteral drainage obstruction implying left UPJO. The right kidney was normal (Fig. 1B). The girl underwent pyeloplasty, with good evolution. Six months later, an abdominal US revealed left kidney renal pelvis with 13 mm and renal function stable in MAG-3 renography. After four years, she remains asymptomatic.
Case 3
The third case refers to a 15-year-old female with prenatal diagnosis of left urinary tract dilatation but normal postnatal scan, with no further follow-up and no known medical problems. The girl was taken to the Emergency Department due to intense left lumbar pain, dysuria, and fever (40.7oC). Laboratory findings showed WBC count of 9.36 x 103/μL with 77.5% neutrophils and 16.6% lymphocytes; CRP of 9.8 mg/dL; blood urea of 24.8 mg/dL; creatinine of 0.79 mg/ dL, and electrolytes within the normal range. Urine culture revealed >105 CFU/mL of Escherichia coli. The patient was hospitalized with acute pyelonephritis. An enlarged left kidney with renal pelvis with 40 mm of anteroposterior diameter was detected on abdominal US. MAG-3 renography showed left kidney hypofunction (22.6%) and slow excretion of the isotope (Fig. 1C). Retrograde cystourethrogram was normal. The patient was submitted to a laparoscopic pyeloplasty. Sixteen months later, kidney’s APRPD was 23 mm in US and in MAG-3 renography the left kidney function further decreased but remained stable. Over a two-year follow-up, the girl remained asymptomatic.
Discussion
The three patients described presented with flank or lumbar pain, in addition to other symptoms. All had a late diagnosis of UPJO, with symptoms and deterioration of renal function, requiring surgical treatment. Pyeloplasty prevented stabilization of renal function in two patients, improved renal function in one case, and all patients became asymptomatic. These findings are similar to those described in the literature.
A high degree of suspicion is required to include UPJO in differential diagnosis of abdominal or back pain in older children and adolescents.
Abbreviations
CFU: Colony-forming units
CRP: C-reactive protein
CT: computed tomography
MAG-3: 99mTc-mercaptoacetyltriglycine-3
UPJO: ureteropelvic junction obstruction
US: ultrasonography
UTI: urinary tract infection
VUR: vesicoureteral reflux
WBC: white blood cell
UTD: urinary tract dilatation
APRPD: anteroposterior renal pelvis diameter
REFERENCES
1. Hashim H, Woodhouse CRJ. Ureteropelvic Junction Obstruction. Eur Urol Suppl 2012; 11:25-32. DOI: 10.1016/j.eursup.2012.01.004. [ Links ]
2. Baskin LS, Wilcox D, Kim MS. UpToDate. Congenital ureteropelvic junction obstruction. [ Links ]
3. Chen F. Genetic and developmental basis for urinary tract obstruction. Pediatr Nephrol 2009;24:1621-32. DOI: 10.1007/s00467-008-1072-y. [ Links ]
4. Hiep T, Nguyen HT, Benson CB, Bromley B, Campbell JB, Chow J, et al. Multidisciplinary consensus on the classification of prenatal and postnatal urinary tract dilation (UTD classification system). J Pediatr Urol 2014; 10: 982-99. DOI: 10.1016/J.JPUROL.2014.10.001. [ Links ]
5. Poudel A, Afshan S, Dixit M. Congenital Anomalies of the Kidney and Urinary Tract. NeoReviews 2016;17:e18-e27. DOI: 10.1542/neo.17-1-e18. [ Links ]
6. Alberti C. Congenital ureteropelvic junction obstruction: physiopathology, decoupling of tout court pelvic dilatation- obstruction semantic connection, biomarkers to predict renal damage evolution. Eur Rev Med Pharmacol Sci 2012; 16:213-9. [ Links ]
7. Lee H, Han SW. Ureteropelvic Junction Obstruction: What We Know and What We Don’t Know. Korean J Urol 2009;50:423-31. DOI: 10.4111/kju.2009.50.5.423.
8. Rosenblum,ND. UpToDate. Evaluation of congenital anomalies of the kidney and urinary tract (CAKUT). [ Links ]
9. Trnka P, Hiatt MJ, Tarantal AF, Matsell DG. Congenital urinary tract obstruction: defining markers of developmental kidney injury. Pediatr Res 2012; 72:446-54. DOI: 10.1038/pr.2012.113. [ Links ]
10. Piscitelli A, Galiano R, Serrao F, Concolino D, Vitale R, D’Ambrosio G, et al. Which cystography in the diagnosis and grading of vesicoureteral reflux? Pediatr Nephrol 2008; 23:107-10. DOI: 10.1007/s00467-007-0651-7.
11. Balighian E, Burke M. Urinary tract infections in children. Pediatr Rev 2018; 39:3. DOI: 10.1542/PIR.2017-0007. [ Links ]
Endereço para correspondência | Dirección para correspondencia | Correspondence
Mariana Abreu
Pediatrics Department
Centro Materno Pediátrico
Centro Hospitalar Universitário de São João
Alameda Prof. Hernâni Monteiro
4200-319 Porto
Email: marianacgabreu@gmail.com
Received for publication: 29.11.2017
Accepted in revised form: 13.11.2018