Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Nascer e Crescer
versão impressa ISSN 0872-0754versão On-line ISSN 2183-9417
Nascer e Crescer vol.27 no.4 Porto dez. 2018
https://doi.org/10.25753/BirthGrowthMJ.v27.i4.12764
WHAT IS YOUR DIAGNOSIS? | QUAL O SEU DIAGNÓSTICO?
Dermatology clinical case
Caso dermatológico
Pedro BrandãoI, Inês Falcão-ReisII, Cátia RodriguesII, Vânia FerreiraII, Isabel SáII
I Obstetrics and Gynecology Department, Centro Hospitalar Tâmega e Sousa. 4564-007 Penafiel. Portugal. pedrobrandaoleite@gmail.com
II Obstetrics and Gynecology Department, Centro Hospitalar Entre Douro e Vouga. 4520-211 Santa Maria da Feira. Portugal. inesreis@hotmail.com; rodrigues_catia@hotmail.com; vania_ferreira@hotmail.com; misabelrcsa@gmail.com
Endereço para correspondência | Dirección para correspondencia | Correspondence
ABSTRACT
Ulcus Vulvae Acutum or Lipschütz ulcer is a rare cause of acute vulvar ulcer that usually affects young, non-sexually active women and consists on the sudden emergence of vulvar ulcers some days after an influenza-like syndrome, usually caused by Epstein-Barr virus. Despite its exuberant presentation, such ulcers are benign and self-limited. Diagnosis is clinical and treatment, symptomatic. Lesions typical resolve within a few weeks, leaving no scars.
The authors describe the case of a 17-year-old, sexually active female adolescent with Lipschütz ulcers.
Keywords: Lipschütz ulcers; Ulcus vulvae acutum; Vulvar ulcers
RESUMO
Ulcus Vulvae Acutum, também conhecida como Úlcera de Lipschütz, é uma causa rara de úlceras vulvares que afeta mulheres jovens, habitualmente virgens, e consiste no aparecimento súbito de úlceras vulvares alguns dias após uma síndrome gripal, geralmente causada pelo vírus Epstein-Barr. Apesar de exuberantes, são úlceras benignas e com resolução espontânea. O diagnóstico é baseado em achados clínicos e o tratamento, sintomático. As lesões tipicamente resolvem após algumas semanas sem deixar cicatriz.
Os autores descrevem o caso de uma adolescente de 17 anos, sexualmente ativa, com úlceras de Lipschütz.
Palavras-chave: Úlceras de Lipschütz; Úlceras vulvares; Ulcus vulvae acutum
A 17-year-old girl attended the Obstetrics and Gynecology Emergency Department due to sudden appearance of vulvar ulcers. She was nulligravida, sexually active, and reported only one sexual partner to date and the use of ethinylestradiol and gestodene (0.02/0.075 mg) combined pill for contraception. The girl had asthma and an iron deficiency anemia and was medicated with oral iron supplement. She reported no past surgeries.
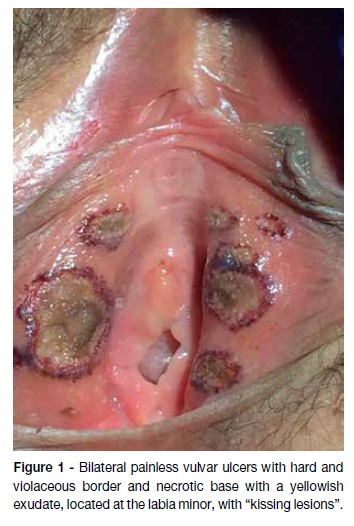
Patient presented with multiple bilateral painless vulvar ulcers (the largest having 1.5 cm diameter), with hard and violaceous borders and necrotic base with a yellowish exudate, located at the internal face of the labia minora. Some lesions were confluent (Figure 1). No inguinal lymphadenopathies were observed. The remaining gynecological examination was normal. She was apyretic (37.4ºC) and had normal vital signs.
The girl reported the occurrence of oral aphthae three days before, at the inferior labial mucosa, left tonsil, and left sub-molar gingiva (Figure 2). Four days earlier, she had flu-like symptoms, including fever (38ºC axillary temperature) and malaise. She had no ophthalmic, neurologic, gastrointestinal, or other genitourinary symptoms.
Serum analyses revealed microcytic hypochromic anemia (Hgb: 10.6g/dL; mean corpuscular volume [MCV]: 69.8fl; mean corpuscular hemoglobin: 21.2pg, leucocytosis (leucocytes: 14.6 x 103/L) with neutrophilia (neutrophils: 81%), elevated reactive C-protein [RCP] (91mg/L), and normal hepatic enzymes. Ancillary exams performed included anti-HIV, hepatitis C, Treponema pallidum, cytomegalovirus (CMV), Epstein-barr virus (EBV), Varicella-Zoster (VZV), and Herpes simplex virus (HSV) antibodies and Hbs antigen. Biopsy samples of the ulcer’s border and base were also retrieved. Patient was medicated with 2.4 millions of I.U. of intra-muscular (IM) benzylpenicillin benzathine, analgesics (paracetamol 1g or ibuprofen 400mg orally every 8 hours, if needed), topic lidocaine2% gel, and local comfort and hygiene measures (hand washing and use of tepid water for personal hygiene, especially after urinating).
After two weeks, the patient was fully recovered. Serum analysis were normal. Serologies were negative to Hepatitis B, C, HIV, and syphilis. CMV, EBV, VZV, and HSV 1 IgG were positive and IgM negative, suggesting previous contact with these agents.HSV 2 IgG and IgM were both negative. Lesion biopsy revealed neutrophilic vasculitis with abundant infiltrate of lymphocytes and neutrophils.
What is the diagnosis?
Differential diagnoses
Behçet disease
Lipschützulcers
Syphilis
Crohn’sdisease
Herpes simplex I or II infection
Diagnosis
Lipschütz ulcers (Ulcus Vulvae Acutum)
Discussion
The most common causes of vulvar ulcers in developed countries are Herpes simplex virus infection and Syphilis, but other etiologies must be considered, including chancroid, lymphogranuloma venereum, granuloma inguinale, secondary bacterial infections, sexual trauma, Behçet disease, Crohn’s disease, or malignancy.1,2Differential diagnosis is based on clinical history, findings, serologic and ulcer exudate tests. Treatment should be specific and cause-directed.
Syphilitic ulcers are typically unique, firm, round, and painless, with inguinal nontender lymphadenopathy. Herpes simplex usually causes painful multiple bilateral vesicular or ulcerative lesions.3Behçet disease is characterized by recurrent oral aphthous ulcers, painful genital ulcers, and uveitis, associated with an auto-immune response.4Crohn’s disease is rarely associated with vulvar ulcers, most cases being attributed to fistulae from intestinal lesions. However, when suspected, biopsy of the lesions is mandatory.5
Acute genital ulceration, also known as Ulcus Vulvae Acutum or Lipschütz ulcers, is a rare cause of acute vulvar ulcers. It usually affects young virgin women and consists on the sudden appearance of vulvar ulcers some days after an influenza-like syndrome. Most commonly, it is caused by Epstein-Barr virus (EBV), but that is not always the case. Ulcers are usually multiple, bilateral, painful, with a purplish hard border and a necrotic yellowish or greyish base, coalescent (“kissing lesions”) with various sizes. Inguinal lymphadenopathies and aphthae are sometimes present. The diagnosis is based on history and physical examination and may be assumed after exclusion of other etiologies. For being a self-limited disease, only local care and symptomatic relief measures are recommended. Lesions typically resolve within a few weeks, leaving no scars.6
This clinical case is relevant for several reasons: it describes a low-frequency entity, refers to an unusual presentation in a sexually active girl with no evidence of EBV recent infection, and raises awareness to health professionals concerning an incorrect diagnosis of a sexually transmitted disease, with implications for unnecessary studies, overtreatment, and potentially a detrimental impact on patient’s psychological and social welfare.
REFERENCES
1. Bandow GD. Diagnosis and Management of Vulvar Ulcers. Dermatol. Clin. 2010; 28:753-63. [ Links ]
2. Bohl TG. Vulvar Ulcers and Erosions: A Clinical Approach. Clin. Obstet. Gynecol. 2015; 58:492-502. [ Links ]
3. Drummond C. Common vulval dermatoses. Aust. Fam. Physician 2011; 40:490-6. [ Links ]
4. Alpsoy E. Behçet’s disease: A comprehensive review with a focus on epidemiology, etiology and clinical features, and management of mucocutaneous lesions. J. Dermatol. 2016; 43:620-32.
5. Barret M, de Parades V, Battistella M, Sokol H, Lemarchand N, Marteau P. Crohn’s disease of the vulva. J. Crohn’s Colitis 2014; 8:563-70.
6. Vieira-Baptista P, Lima-Silva J, Beires J, Martinez-de-Oliveira J. Lipschütz ulcers: should we rethink this? An analysis of 33 cases. Eur. J. Obstet. Gynecol. Reprod. Biol. 2016; 198:149-52. [ Links ]
Endereço para correspondência | Dirección para correspondencia | Correspondence
Pedro Brandão
Obstetrics and Gynecology Department
Centro Hospitalar Tâmega e Sousa.
Avenida do Hospital Padre Américo 210,
4564-007 Guilhufe
Email: pedrobrandaoleite@gmail.com
Received for publication: 08.08.2017
Accepted in revised form: 27.09.2017