Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Nascer e Crescer
versão impressa ISSN 0872-0754versão On-line ISSN 2183-9417
Nascer e Crescer vol.27 no.4 Porto dez. 2018
https://doi.org/10.25753/BirthGrowthMJ.v27.i4.13698
ORIGINAL ARTICLES | ARTIGOS ORIGINAIS
Fluid administration − Which direction?
Administração de soros − Que direção?
Sara VazI,II*,Sofia Cochito SousaI*, Francisco AbecasisI, Leonor BotoI, Joana RiosI, Cristina CamiloI, Marisa VieiraI
I Pediatric Intensive Care Unit, Pediatrics Department, Hospital de Santa Maria, Centro Hospitalar de Lisboa Norte; Centro Académico de Medicina de Lisboa. 1649-035 Lisboa, Portugal. saravaz87@gmail.com; sofia.cochito.sousa@gmail.com; francisco@abecasis.name; boto.leonor@gmail.com; joanarios6@gmail.com; cristinacamilo.cc@gmail.com; marisa.p.vieira@gmail.com
II Pediatrics Department, Hospital de Santo Espírito da Ilha Terceira. 9700-049, Angra do Heroísmo, Portugal. saravaz87@gmail.com
*Both authors contributed equally to this work
Endereço para correspondência | Dirección para correspondencia | Correspondence
ABSTRACT
Introduction: Although fluid administration for intravenous hydration is a common practice in pediatric age, it is not devoid of risks.
Methods: This was a retrospective cohort study including all children admitted to surgical recovery and receiving intravenous hydration at a Pediatric Intensive Care Unit between January and December 2015. Sodium, chloride, and base excess values were registered on two occasions: after surgery and during Unit’s hospitalization.
Results: Two hundred and seven children were included in the study, 66% of which, male, with a median age of 6.7 years. Fluids used consisted of 0.9% saline solution, 0.45% saline solution, and polyelectrolyte solution. The most frequently used fluids were polyelectrolyte (62%) and 0.9% saline solution (48%) at the operating room, and 0.9% saline (63%) and 0.45% saline (44%) solutions at the Pediatric Intensive Care Unit.
At the operating room, 0.9% saline solution led to higher chloride median values and more negative base excess (metabolic acidosis) values compared with polyelectrolyte solution. At the Pediatric Intensive Care Unit, 0.9% saline solution administration resulted in hyperchloremia (p=0.002) and more metabolic acidosis (p=0.019) compared with 0.45% saline solution. There was no statistically significant association between type of solution used and sodium values.
Discussion: This study shows that the use of 0.9% saline solution is associated with development of hyperchloremic acidosis. This suggests that replacement of 0.9% saline solution with a plasma-like electrolyte solution may improve patient outcomes.
Keywords: Acid-base imbalance; Fluids; Hyperchloremia; Hyponatremia; Metabolic acidosis; Water-electrolyte imbalance
RESUMO
Introdução: A utilização de soros para hidratação endovenosa é uma prática comum em idade pediátrica, não sendo isenta de riscos.
Métodos: Este foi um estudo de coorte retrospetivo que incluiu todas as crianças admitidas para recobro cirúrgico com necessidade de hidratação endovenosa numa Unidade de Cuidados Intensivos Pediátricos, entre janeiro e dezembro de 2015. Foram registados os valores de sódio, cloro e excesso de bases em dois períodos: após a cirurgia e durante o internamento na Unidade.
Resultados: Foram incluídas 207 crianças, 66% das quais do sexo masculino, com idade mediana de 6,7 anos. Os soros utilizados foram soro fisiológico, NaCl 0,45% com 5% de dextrose e polieletrolítico. Os soros mais frequentemente utilizados foram polieletrolítico (62%) e soro fisiológico (48%) no bloco operatório e soro fisiológico (63%) e NaCl 0,45% (44%) na Unidade de Cuidados Intensivos Pediátricos. No bloco operatório, a utilização de soro fisiológico traduziu-se em valores medianos de cloro mais elevados e valores de excesso de bases (acidose metabólica) mais negativos do que os observados com soro polieletrolítico. Na Unidade de Cuidados Intensivos Pediátricos, a administração de soro fisiológico conduziu a hipercloremia (p=0,002) e acidose metabólica mais pronunciada (p=0,019) do que o observado com NaCl 0,45%. Não foi observada uma associação estatisticamente significativa entre o tipo de soro utilizado e os valores de sódio registados.
Discussão: Este estudo demonstra que a utilização de soro fisiológico se associa ao desenvolvimento de acidose hiperclorémica. Tal sugere que a substituição de soro fisiológico por um soro com valores de eletrólitos semelhantes ao plasma poderá ter benefícios para o doente.
Palavras-chave: Acidose metabólica; Equilíbrio ácido-base; Equilíbrio hidro-eletrolítico; Hipercloremia; Hiponatremia; Soro
Introduction
Administration of intravenous fluids is a common practice in the perioperative setting in pediatric age.1 However, for being so frequently used, it is often trivialized. Fluids are essential in promoting adequate hydration, preventing hydroelectrolytic disorders, and maintaining hemodynamic and glycemic stability.2 As with any other therapy, its use is not devoid of risks and can have detrimental effects.3 Important hydroelectrolytic and acid-base imbalances are some of the adverse events associated with the use of intravenous fluids.4-7
The applicability of a fluid is based on three assumptions − maintenance, replacement, and resuscitation - and fluid choice is dictated by its purpose.1,2 The Holliday-Segar formula, published in 1957, allows to estimate a child’s basic water requirements and has been a cornerstone in clinical practice since, including in the postoperative setting. Based on the concept of electrolyte maintenance proposed by the authors, an hypotonic fluid is the ideal maintenance fluid for hospitalized children.8 Several studies have subsequently demonstrated the association between hypotonic fluid and a higher probability of hyponatremia, with potential risks of severe neurological damage or even death due the increased intracranial pressure promoted by cerebral edema.5,7,9-12
Postsurgical patients are at high risk of hyponatremia due to non-osmotic stimuli for antidiuretic hormone release.6 Recognition of this fact led to a change in clinical practice, through an increasing use of 0.9% saline solution. However, evidences supporting the superiority of this solution over the remaining are lacking.13 In fact, this is an unevenly balanced fluid, with an excessively high chloride content (154 mmol/L in saline solution versus 98−106±2mmol/L of plasma chloride), and its use is associated with development of hyperchloremic acidosis, which is potentially deleterious. Recent studies have shown the benefits of using balanced solutions, with a significantly lower concentration of sodium and chloride and closer to plasma composition. Such solutions seem superior in maintaining the hydroelectrolyte and acid-base balance compared to the traditionally used hypotonic and normal saline solutions.7,14-16
Considering this, it is not surprising that fluid selection in clinical practice varies considerably and there is no consensus on the optimal fluid composition.6
The present study aimed to investigate the impact on the hydroelectrolytic and acid-base balance of different types of fluid used in children care during postoperative recovery in a Portuguese Pediatric Intensive Care Unit (PICU), in order to optimize clinical practice.
Methods
This was a retrospective cohort study that analyzed the administration of intravenous fluid therapy in children hospitalized for postoperative recovery in a PICU from January 1 to December 31 of 2015. Data was collected from children’s computerized clinical processes (Pics Care Suite Program from Siemens®).
Selection criteria included children with one month to 18 years of age, admitted to the PICU for postoperative recovery and receiving intravenous hydration during hospitalization. Exclusion criteria included absence of information regarding type of fluid used at the operative room (OR) or PICU and absence of laboratory analysis during the postoperative period.
Demographic variables (sex, age), type of surgery, and type of fluid used, both in OR and PICU, were analyzed. Fluids were classified as (i) polyelectrolyte solution (e.g. Ringer Lactate® and Plasmalyte®), (ii) 0.9% saline solution, or (iii) 0.45% saline solution with 5% dextrose. Polyelectrolyte solution and 0.9% saline solution could additionally have 5% dextrose.
Sodium, chloride, and base excess (BE) values were analyzed on two occasions. The first analysis was performed at the time up to four hours after admission to the PICU and was considered to mirror the fluid used in the OR. Time since the end of this first analysis until the end of the 24-hour hospitalization period in the PICU was designated the second analysis and considered to mirror the fluid used in the Unit during hospitalization.
Hyponatremia was defined as sodium values lower than 135 mmol/L and hypernatremia, as sodium values over 145 mmol/L. Hypochloremia and hyperchloremia were defined as chloride values lower than 98 mmol/L and higher than 106 mmol/L, respectively. BE values lower than -2mmol/L were used as cut-off for metabolic acidosis assumption.
Statistical analysis
Statistical analysis was performed using IBM SPSS® software version 22.0 and Excel®. Descriptive statistics were performed. Categorical variables were described as absolute (n) and relative (%) frequencies. Quantitative variables were characterized by the mean and standard deviation when data was normally distributed and by the median and interquartile range (IQR 25,75) when normality was not present. Parametric student’s t-test and non-parametric Mann-Whitney U test were used for variable analysis, when applicable. Statistical significance was set at p<0.05.
Results
A total of 220 children hospitalized during the considered time period were analyzed. From these, 207 children met the inclusion criteria and were included in the study and 13 were excluded due to absence of laboratory registries in both OR and PICU. Children included in the analysis had a median (IQR) of 6.7 (1.55−12.6) years.
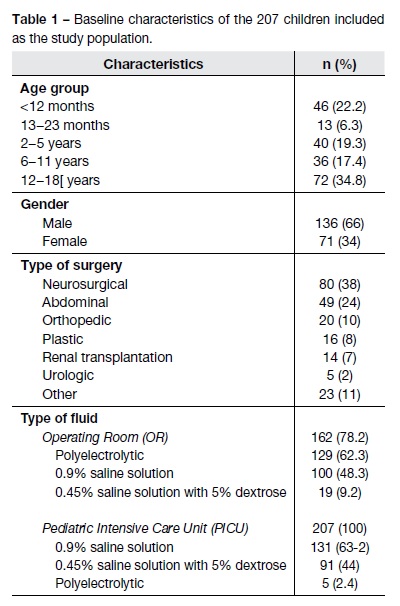
Table 1 summarizes the baseline characteristics of the population included in the study, including demographics, type of surgery, and fluid received. Hospitalizations were predominant in male children (n=136, 66%) and were mostly motivated by neurosurgical (38%) followed by abdominal (24%) interventions. Polyelectrolyte was the most frequently used fluid during surgery (62.3%), while 0.9% saline solution was the most frequently used fluid during postoperative period (63.2%).
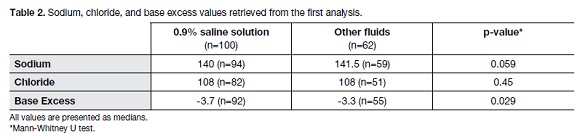
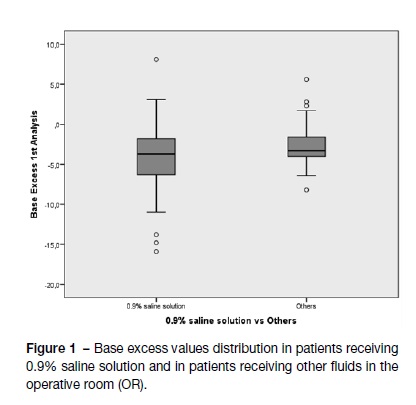
Due to lack of information regarding type of fluid administered, only 162 children were evaluated in the OR setting. Sodium, chloride, and BE values were compared amongst children receiving 0.9% saline solution and children receiving polyelectrolyte solution and 0.45% saline solution with 5% dextrose. A statistically significant association (p=0.029) was found between higher metabolic acidosis and the administration of 0.9% saline solution (Table 2). This can be observed in the boxplot depicted in Figure 1, in which more negative BE values are observed in patients receiving 0.9% saline solution compared with those who did not. Statistically significant differences were not found between both groups concerning sodium and chloride values.
No comparative analysis was performed between the use of 0.9% saline solution only and polyelectrolyte solution only in the OR, since the sample in question was too small (n=24; 14.8%).
When analyzing the prevalence of hyponatremia, hypernatremia, hyperchloremia, and metabolic acidosis in children in the OR, no differences were observed between those who did and did not receive 0.9% saline solution.
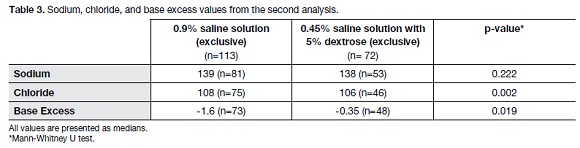
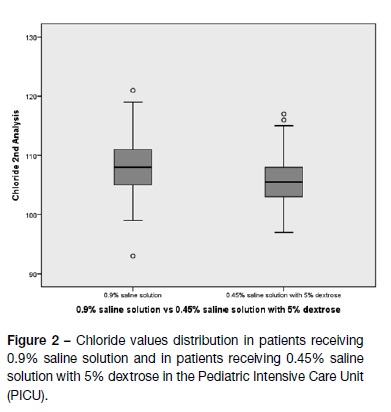
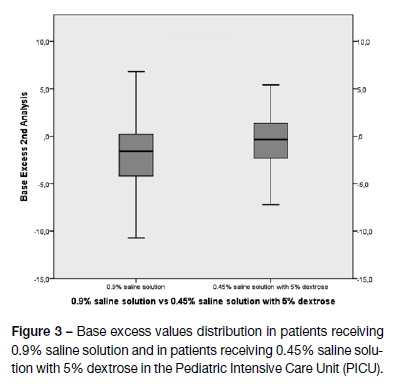
Table 3 compares sodium, chloride, and BE content between the two fluids most frequently used in the PICU: 0.45% saline solution with 5% dextrose and 0.9% saline solution. Use of polyelectrolyte solution in the PICU was not analyzed due to small sample size (n=5; 2.4%). Results showed a significantly higher median chloride value with the use of 0.9% saline solution only than with the use of 0.45% saline solution with 5% dextrose (p=0.002). Considering BE medians, more negative values were found when 0.9% saline solution was administered compared with 0.45% saline solution with 5% dextrose (p=0.019).
Figures 2 and 3 depict chloride and BE values variability when using 0.9% saline solution and 0.45% saline solution with 5% dextrose. There is a clear hyperchloremia increase and more negative BE values when 0.9% saline solution is used in detriment of a less chloride-rich fluid. There was no significant difference between groups regarding sodium values in PICU.
On the other hand, there was a statistically significant difference in the prevalence of hyperchloremia between 0.9% saline solution and 0.45% saline solution with 5% dextrose (p=0.005, ANOVA test). There was no difference in hyponatremia, hypernatremia, or metabolic acidosis prevalence between both groups.
Discussion
Fluid selection and composition is currently a subject of debate. Although studies are not unanimous, they seem to agree on a superiority of balanced solutions with a similar composition to plasma.4,17-19 Ringer’s lactate and Plasma-lyte A are examples of balanced solutions, with an electrolyte concentration similar to plasma, and have been shown to maintain a better acid-base balance after elective surgery.19
Neurosurgical interventions are one of the most common reasons for hospital admission in the PICU and one of current indications for NaCl 0.9% use, together with other situations with significant risk of inappropriate antidiuretic hormone secretion (e.g. central nervous systems disease; hypovolemic states; pulmonary diseases; post otorhinolaryngology and orthopedics surgery).20 However, recent studies also favor the use of balanced solutions instead of NaCl 0.9% in these situations.1,7,14,16,17,19-20
Although normal saline can occur in specific clinical conditions, results of this study suggest that the use of a 0.9% saline solution is associated with greater hyperchloremic metabolic acidosis when compared with a fluid with half that ionic concentration. These results agree with other studies and meta-analyses available in the literature.1,17,19-22
In the present study, the use of 0.9% saline solution in the OR was associated with a greater metabolic acidosis. However, and although chloride median values were higher in the 0.9% saline solution group, chloride values in patients receiving this solution were not significantly different from patients receiving other solutions. These results should be interpreted with caution, since some patients simultaneously received other fluids (polyelectrolytic or 0.45% saline solution with 5% dextrose) besides 0.9% saline solution.
Saline solution 0.9% is commonly used in clinical practice, although it is not the main fluid used in Pediatrics as maintenance therapy in Portugal. Although it is termed physiological’, it is known to have supraphysiological concentrations of sodium (Na+ 154 mEq/L) and chloride (Cl- 154 mEq/L).4,13 Results from this study suggest that this fluid may pose risk to patients, since it favors development of hyperchloremic acidosis, which can be associated with decreased renal perfusion and acute kidney injury.17,18,20-24 Other studies have also demonstrated that administration of large volumes of 0.9% saline solution may associate with coagulopathy.25,26 On the other hand, the association between hyperchloremic acidosis and mortality remains unclear.4,17,20
In this analysis, the authors could not establish an association between the use of one type of (iso or hypotonic) fluid and development of hypo or hypernatremia. This contrasts with results retrieved from studies reporting that 0.45% saline solution with 5% dextrose (hypotonic, Na+ 77mmol/L) was associated with hyponatremia, a potentially life-threatening condition.6,7,9-11,15,27 The authors of the present work speculate that their results may be related to study limitations.
This study has some limitations due to its retrospective nature, including its external validity. Also, because there was no a priori defined protocol, not all patients completed laboratory evaluations on the two predefined occasions. Consequently, patient’s preoperative analyses were not systematically accessed, hindering the verification of whether hydroelectrolytic or acid-base changes were due to preexisting alterations or to the administered fluid. The volume of fluid administered was also not quantified, which would have been important to understand how each fluid influenced results obtained. One final study limitation is the fact that some patients simultaneously used more than one type of fluid.
According to the authors’ understanding, this is the first study in Portugal to assess fluid therapy in patients with pediatric age, exclusively in the postoperative setting. And, despite its retrospective nature and discussed limitations, results retrieved generally agree with previously published data.
In conclusion, this study demonstrates that the use of fluids with high chloride content is associated with a higher risk of hyperchloremic acidosis. Data suggests that replacement of 0.9% saline solution by another fluid with an electrolyte content closer to plasma, either in the OR or in the recovery room, may benefit patients. Although NaCl 0.9% still has a role in a goal-oriented balanced fluid therapy strategy, more studies are needed to determine how much is too much. Therefore, the authors believe that further prospective, controlled, randomized studies are necessary to better identify which fluid has the lowest impact in patients’ hydroelectrolytic and acid-base balance.
REFERENCES
1. Orbegozo Cortés D, Rayo Bonor A, Vincent JL. Isotonic crystalloid solutions: A structured review of the literature. Br J Anaesth. 2014; 112:968-81. [ Links ]
2. Intravenous fluid therapy in children and young people in hospital. Nice Guidelines (2016). [ Links ]
3. Holliday MA, Ray PE, Friedman AL. Fluid therapy for children: facts, fashions and questions. Arch Dis Child. 2007; 92:546-50. [ Links ]
4. Guidet B, Soni N, Rocca G, Kozek S, Vallet B, Annane D, et al. A balanced view of balanced solutions. Critical Care. 2010; 14:325. [ Links ]
5. Moritz ML, Ayus JC. Hospital-acquired hyponatremia-why are hypotonic parenteral fluids still being used? Nat Clin Pract Nephrol. 2007; 3:374-82. [ Links ]
6. Oh GJ, Sutherland SM. Perioperative fluid management and postoperative hyponatremia in children. Pediatr Nephrol. 2016; 31:53-60. [ Links ]
7. Mcnab S, Duke T, South M, Babl FE, Lee KJ, Arnup SJ, et al. 140 mmol/L of sodium versus 77 mmol/L of sodium in maintenance intravenous fluid therapy for children in hospital (PIMS): a randomised controlled double-blind trial. 2014; 6736:1-8. [ Links ]
8. Holliday MA, Segar WE. The maintenance need for water in parenteral fluid therapy. Pediatrics. 1957; 19:823-32. [ Links ]
9. Friedman JN. Risk of acute hyponatremia in hospitalized children and youth receiving. Paediatr Child Health. 2013; 18:102-4. [ Links ]
10. Hoorn EJ, Geary D, Robb M, Halperin ML, Bohn D. Acute hyponatremia related to intravenous fluid administration in hospitalized children: an observational study. Pediatrics. 2004; 113:1279-84. [ Links ]
11. Wang J, Xu E, Xiao Y. Isotonic Versus Hypotonic Maintenance IV Fluids in Hospitalized Children: A Meta-Analysis. Pediatrics. 2014; 133:105-13. [ Links ]
12. Cavari Y, Pitfield AF, Kissoon N. Intravenous Maintenance Fluids Revisited. Pediatr Emerg Care. 2013; 29:1225-8. [ Links ]
13. Lobo DN, Awad S. Should chloride-rich crystalloids remain the mainstay of fluid resuscitation to prevent “pre-renal” acute kidney injury? Kidney Int. 2014; 86:1096-105.
14. Taylor D, Durward A. What routine intravenous maintenance fluids should be used? Arch Dis Child. 2004; 89:411-8. [ Links ]
15. Choong K, Arora S, Cheng J, Farrokhyar F, Reddy D, Thabane L, et al. Hypotonic Versus Isotonic Maintenance Fluids After Surgery for Children: A Randomized Controlled Trial. Pediatrics. 2011; 128:857-66. [ Links ]
16. Coulthard MG, Long DA, Ullman AJ, Ware RS. A randomised controlled trial of Hartmann’s solution versus half normal saline in postoperative paediatric spinal instrumentation and craniotomy patients. Arch Dis Child. 2012; 97:491-6.
17. Krajewski ML, Raghunathan K, Paluszkiewicz SM, Schermer CR, Shaw AD. Meta-analysis of high-versus low-chloride content in perioperative and critical care fluid resuscitation. Br J Surg. 2015; 102:24-36. [ Links ]
18. McFarlane C, Lee A. A comparison of Plasmalyte 148 and 0.9% saline for intra-operative fluid replacement. Anaesthesia. 1994; 49:779-81. [ Links ]
19. Young JB, Utter GH, Schermer CR, Galante JM, Phan HH, Yang Y, et al. Saline versus Plasma-Lyte A in initial resuscitation of trauma patients: a randomized trial. Ann Surg. 2014; 259:255-62. [ Links ]
20. Jagt VD. Fluid management of the neurological patient: a concise review. Critical Care. 2016; 20:126. doi: 10.1186/s13054-016-1309-2. [ Links ]
21. Handy JM, Soni N. Physiological effects of hyperchloraemia and acidosis. Br J Anaesth. 2008; 101:141-50. [ Links ]
22. Magder S. Balanced versus unbalanced salt solutions: What difference does it make? Best Pract Res Clin Anaesthesiol. 2014; 28:235-47. [ Links ]
23. Waters JH, Gottlieb A, Schoenwald P, Popovich MJ, Sprung J, Nelson DR. Normal saline versus lactated Ringer’s solution for intraoperative fluid management in patients undergoing abdominal aortic aneurysm repair: an outcome study. Anesth Analg [Internet]. 2001; 93:817-22.
24. Yunos NM, Bellomo R, Hegarty C, Story D, Ho L, Bailey M. Association between a chloride-liberal vs chloride-restrictive intravenous fluid administration strategy and kidney injury in critically ill adults. Jama. 2012; 308:1566-72. [ Links ]
25. Todd SR, Malinoski D, Muller PJ, Schreiber MA. Lactated Ringer’s is Superior to Normal Saline in the Resuscitation of Uncontrolled Hemorrhagic Shock. 2007; 62:636-9.
26. Ahn HJ, Yang M, Gwak MS, Koo MS, Bang SR, Kim GS, et al. Coagulation and biochemical effects of balanced salt-based high molecular weight vs saline-based low molecular weight hydroxyethyl starch solutions during the anhepatic period of liver transplantation. 2008; 63:235-42.
27. McNab S, Ware RS, Neville KA, Choong K, Coulthard MG, Duke T, et al. Isotonic versus hypotonic solutions for maintenance intravenous fluid administration in children. Cochrane Database Syst Rev. 2014:CD009457. doi: 10.1002/14651858.CD009457.pub2. [ Links ]
Endereço para correspondência | Dirección para correspondencia | Correspondence
Sara Vaz
Pediatric Intensive Care Unit,
Pediatrics Department,
Hospital de Santa Maria
Centro Hospitalar de Lisboa Norte
Avenida Prof. Egas Moniz s/n
1649-035 Lisboa, Portugal
Email: sara.o.vaz@azores.gov.pt
Acknowledgments
The authors sincerely acknowledge all the clinicians involved in patient care.
Received for publication: 30.12.2017
Accepted in revised form: 20.08.2018