Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Nascer e Crescer
versão impressa ISSN 0872-0754versão On-line ISSN 2183-9417
Nascer e Crescer vol.26 no.4 Porto 2017
CASE REPORTS | CASOS CLÍNICOS
X – linked Hypohidrotic Ectodermal Dysplasia and atopic eczema – case report and discussion on mechanisms of eczema
Displasia Ectodérmica Hipohidrótica ligada ao X e eczema atópico - relato de um caso e discussão sobre os mecanismos do eczema
Catarina MoreiraI,II; Ana Filipa DuarteIII; Filomena AzevedoII; Alberto MotaI,II
I Department of Dermatology and Venereology, Centro Hospitalar São João. 4200-319 Porto, Portugal. cat_moreira@icloud.com; filomena.azevedo@hsjoao.min-saude.pt; ajvmota@gmail.com
II Faculty of Medicine, University of Porto. 4200-319 Porto, Portugal. cat_moreira@icloud.com; ajvmota@gmail.com
III Centro de Dermatologia Epidermis, Instituto CUF Porto. 4460-188 Senhora da Hora, Portugal. duarte.af.t30@gmail.com
ABSTRACT
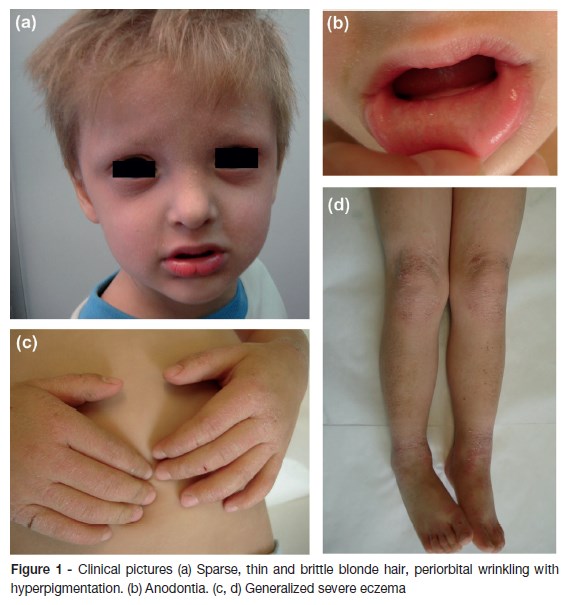
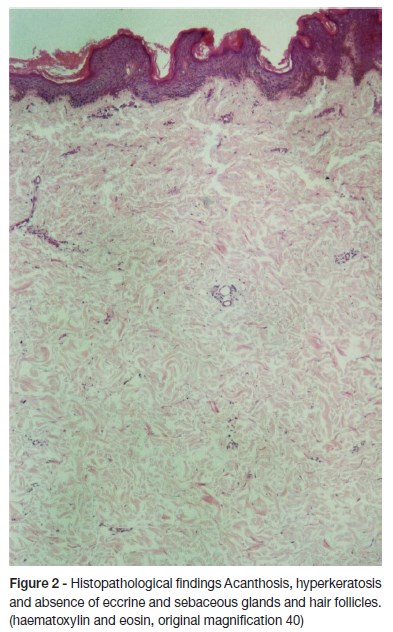
X-linked Hypohidrotic Ectodermal Dysplasia (XHED) is an inherited disorder that involves defective development of tissues derived from embryonic ectoderm and it is generally suspected by the triad of hypohidrosis, hypotrichosis and hypodontia. We report a four-year-old boy with a persistent and severe eczema, anodontia, a sparse, thin and blonde hair, periorbital wrinkling with hyperpigmentation and absence of sweating. Laboratory results showed elevation of total serum IgE and IgE specific to house dust mites and grass pollen. Skin biopsy revealed absence of eccrine and sebaceous glands and hair follicles. The genetic molecular study disclosed a c.463C>T (p.Arg155Cys) mutation of the EDA1 gene, consistent with X-linked HED. Although XHED has a favorable prognosis, eczema is a major problem and the eczematous characteristics of patients skin resemble those of atopic dermatitis. Ceramide profile, reduction of natural moisturizing factors due to hypohidrosis and skin barrier dysfunction elicited by airborne proteins likely contribute to persistent and difficult-to-control AD-like eczema. As a consequence of the rarity of the disease, obtaining a significant number of clinical studies to clarify and validate the pathways involved in skin barrier dysfunction and the consequent eczematous lesions in HED patients will probably remain a challenge.
Keywords: Atopic dermatitis; developmental defects; ectodermal dysplasia
RESUMO
A Displasia Ectodérmica Hipohidrótica ligada ao X (DEHX) é uma patologia hereditária responsável por defeitos no desenvolvimento dos tecidos de origem ectodérmica, sendo geralmente sugerida pela tríade de hipohidrose, hipotricose e hipodontia. Reportamos o caso de uma criança de quatro anos, do género masculino, com um eczema grave e persistente, anodontia, cabelo fino e esparso, pregueamento periorbitário e ausência de sudorese. Os exames laboratoriais mostraram elevação da IgE sérica total e das IgEs específicas para ácaros e pólens. A biópsia cutânea realizada evidenciou ausência de glândulas écrinas e sebáceas e de folículos pilosos. O estudo genético molecular revelou uma mutação c.463C>T (p.Arg155Cys) no gene EDA1, consistente com DEHX. Embora a DEHX tenha um prognóstico favorável, o eczema constitui um problema importante e as características eczematosas da pele dos doentes relembram as dos doentes com dermatite atópica. O perfil de ceramidas, a redução dos fatores emolientes naturais devido à hipohidrose e a disfunção da barreira cutânea potenciada por proteínas aerotransportadas, parecem constituir fatores contributivos para o eczema persistente e de difícil controlo. Em virtude da raridade da doença, é provável que se mantenha desafiadora a obtenção de um número significativo de estudos clínicos que clarifiquem e validem os mecanismos envolvidos na disfunção da barreira cutânea e das lesões cutâneas eczematosas nestes doentes.
Palavras-chave: Dermatite atópica; defeitos do desenvolvimento; displasia ectodérmica
INTRODUCTION
Ectodermal dysplasias (ED) comprise a large, heterogeneous group of inherited disorders defined by primary defects in the development of two or more tissues derived from embryonic ectoderm, primarily the skin and its appendages (hair follicles, eccrine glands, sebaceous glands and nails) and also the teeth.1
Hypohidrotic ectodermal dysplasia (HED) is the most common form of ED, and the majority of HED cases are associated with mutations or deletions in the ectodysplasin (EDA) gene inherited on the X-chromosome. X-linked Hypohidrotic Ectodermal Dysplasia (XLHED) is generally suspected by the triad of hypohidrosis, hypotrichosis and hypodontia.2
CASE REPORT
A 4-year-old boy was referred due to a persistent and severe eczema since he was four months old. Treatment with moisturizers and topical corticosteroids was unsuccessful. Physical examination revealed a generalized eczema with lichenification and scaling more intense in the face, arms and hands, anodontia, a sparse, thin and brittle blonde hair, periorbital wrinkling with hyperpigmentation and absence of sweating (figure 1). Previous history of recurrent upper respiratory tract infections and episodes of hyperpyrexia were recorded. The parents and the four brothers were apparently healthy.
Laboratory results showed a raised serum immunoglobulin E (IgE) level (2598 kU/L; normal range: < 107 kU/L) with normal chemistry and complete blood count. High levels of specific IgE antibodies to dermatophagoides pteronyssinus (>100.00 kU/L), dermatophagoides farinae (85.40 kU/L) and grass pollen (99.10 kU/L) were also detected. Skin biopsy showed acanthosis, hyperkeratosis and absence of eccrine and sebaceous glands and hair follicles (figure 2). An orthopantography confirmed maxilla hypoplasia and anodontia. The genetic molecular study was consistent with clinical diagnosis, revealing a c.463C>T (p.Arg155Cys) mutation of the EDA1 gene.
DISCUSSION
The cardinal clinical features of XLHED comprise deficient sweating, partial or complete absence of dentition and sparse hair. Other physical findings include saddle-shaped nose or depressed nasal bridge, thick and protruding lips, sparse or absent eyebrows, dry skin with eczematous changes and periorbital pigmentation.3
It has been widely accepted that patients with HED have an increased risk of death from hyperpyrexia due to the inability to sweat and regulate core body temperatures, but recent studies show that prognosis has improved over the last decades, probably as a result of more prompt recognition and adequate management.4
Although mortality of HED has decreased, complications often occur and the greatest impact on quality of life seems to be related to cutaneous symptoms. In fact, hypohidrosis can lead to severe heat intolerance, imposing sufficient hydration and avoidance of excessive heat exposure, which may have a major impact on daily planning and activities. Eczema has also been reported a major problem influencing quality of life and seems to affect up to two-thirds of the male HED patients.5
From a clinical point of view, the eczematous characteristics of ED skin resemble those of atopic dermatitis (AD). For AD, recent knowledge suggests that barrier dysfunction is the central cause.6 Although in AD, filaggrin mutations and abnormalities in epidermal lipids are recognized mechanisms to skin barrier dysfunction, few data are available about the lipid profile and the filaggrin status in the stratum corneum of patients with HED. Jungersted et al. demonstrated that HED patients have a ceramide profile similar to that observed in AD skin, which could indicate some resemblance in the pathogenesis of both diseases.7 A study found that filaggrin expression in the skin of patients with HED was similar to normal subjects and concluded that atopic diathesis in HED appear not to be associated with filaggrin.8 Recently, Watabe et al. compared the concentrations of various natural moisturizing factors in the stratum corneum between anhidrotic regions and normal skin areas in patients with acquired idiopathic generalized anhidrosis and with segmental anhidrosis.9 The levels of lactate, urea, sodium, and potassium were significantly lower in anhidrotic areas, so the authors claimed that several natural moisturising factors components are mostly derived from sweat gland function and play a crucial role in maintaining the physiological hydration state of the stratum corneum. Therefore, it is plausible to speculate that in HED patients, hypohidrosis or anhidrosis by itself might contribute to skin barrier disruption.
It was interesting to observe that our patient had a generalized eczema that was more intense in air-exposed skin surfaces. In fact, it has been previously indicated that periorbital dermatitis could be one of the characteristics of HED skin lesions.8 However, the meaning of this finding and the elucidation of the underlying mechanism are lacking. It is recognized that in a subset of patients with AD, airborne proteins are a contributing factor to the disease, and this group typically shows lesions predominately on air-exposed skin surfaces including the face, neck and arms and a more severe disease, resistant to conventional therapies. The most common airborne proteins significant in AD include house dust mites, cockroach, pet dander and multiple pollens. The reactions to airborne proteins are likely mediated by multiple mechanisms, including direct proteolytic activity leading to degradation of the stratum corneum, direct activation of proteinase-activated receptors-2 itch receptors, and IgE binding leading to increased local inflammation. Although, atopy patch test has the best evidence for identifying AD patients with a relevant airborne protein reaction driving their disease, it has also been demonstrated a linear correlation between increasing severity of AD and increasing levels of IgE specific to house dust mites and other proteins.10
In the light of these views, it is possible that in our patient, a significant skin barrier dysfunction was elicited by airborne proteins, for which high levels of specific IgE to house dust and grass pollen were demonstrated. This effect acting synergistically with the reduction of natural moisturizing factors due to hypohidrosis as discussed previously, likely contributed to the persistent and difficult-to-control AD-like eczema.
As a consequence of the rarity of the disease, obtaining a significant number of clinical studies to clarify and validate the pathways involved in skin barrier dysfunction and the consequent eczematous lesions in HED patients will probably remain a challeng.
REFERÊNCIAS BIBLIOGRÁFICAS
1. Itin PH. Ectodermal dysplasia: thoughts and practical concepts concerning disease classification - the role of functional pathways in the molecular genetic diagnosis. Dermatology. 2013; 226:111-4. [ Links ]
2. Fete M, Hermann J, Behrens J, Huttner KM. X-linked hypohidrotic ectodermal dysplasia (XLHED): clinical and diagnostic insights from an international patient registry. Am J Med Genet A. 2014; 164A:2437-42. [ Links ]
3. Callea M, Teggi R, Yavuz I, Tadini G, Priolo M, Crovella S, et al. Ear nose throat manifestations in hypoidrotic ectodermal dysplasia. Int J Pediatr Otorhinolaryngol. 2013; 77:1801-4. [ Links ]
4. Bluschke G, Nusken KD, Schneider H. Prevalence and prevention of severe complications of hypohidrotic ectodermal dysplasia in infancy. Early Hum Dev. 2010; 86:397-9. [ Links ]
5. Pavlis MB, Rice ZP, Veledar E, Bradley BR, Spraker MK, Chen SC. Quality of life of cutaneous disease in the ectodermal dysplasias. Pediatr Dermatol. 2010; 27:260-5. [ Links ]
6. Weidinger S, Novak N. Atopic dermatitis. Lancet 2016; 387:1109-22. [ Links ]
7. Jungersted JM, Hogh JK, Hellgren LI, Agner T, Jemec GB. Ceramide profile in hypohidrotic ectodermal dysplasia. Clin Exp Dermatol. 2012; 37:153-5. [ Links ]
8. Koguchi-Yoshioka H, Wataya-Kaneda M, Yutani M, Murota H, Nakano H, Sawamura D, et al. Atopic diathesis in hypohidrotic/anhidrotic ectodermal dysplasia. Acta Derm Venereol. 2015; 95:476-9. [ Links ]
9. Watabe A, Sugawara T, Kikuchi K, Yamasaki K, Sakai S, Aiba S. Sweat constitutes several natural moisturizing factors, lactate, urea, sodium, and potassium. J Dermatol Sci. 2013; 72:177-82. [ Links ]
10. Schafer T, Heinrich J, Wjst M, Adam H, Ring J, Wichmann HE. Association between severity of atopic eczema and degree of sensitization to aeroallergens in schoolchildren. J Allergy Clin Immunol. 1999; 104:1280-4. [ Links ]
Catarina Moreira
Department of Dermatology and Venereology
Centro Hospitalar São João
Alameda Prof. Hernâni Monteiro,
4200-319 Porto
Email: cat_moreira@icloud.com
Received for publication: 30.12.2016 Accepted in revised form: 06.02.2017














