Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Nascer e Crescer
versão impressa ISSN 0872-0754
Nascer e Crescer vol.24 no.1 Porto mar. 2015
ARTIGO ORIGINAL / ORIGINAL ARTICLE
Preterm infants under 27 weeks gestational age: outcomes in a tertiary hospital
Pré-Termos Abaixo Das 27 Semanas De Idade Gestacional: Desfechos Num Hospital Terciário
Maria Isabel SáI, Miguel FonteII, Cármen CarvalhoII, Paula SoaresII, Alexandra AlmeidaII, Ana JanuárioIII, Sónia GouveiaII,IV, Joaquim SaraivaI
IS. Ginecologia e Obstetrícia, Dep. da Mulher e da Medicina Reprodutiva, CHPorto, 4099-001 Porto, Portugal. E-mail: misabelrcsa@gmail.com; saraivajp@hotmail.com
IIS. Neonatologia, Dep. da Infância e da Adolescência do CHPorto, 4099-001 Porto, Portugal. E-mail: miguelfonte@gmail.com; carmencarvalho01@gmail.com; mpccsoares@hotmail.com; maria.alexandra.almeida@gmail.com; sonia.gouveia@fc.up.pt
IIIDep. Matemática, Faculdade de Ciências da Universidade do Porto e Gabinete de Estatística, Modelação e Aplicações Computacionais – Centro de Matemática da Universidade do Porto,4200-465 Porto, Portugal. E-mail: anafjanuario@hotmail.com
IVDep. Matemática, Instituto de Engenharia Electrónica e Telemática de Aveiro, Universidade de Aveiro, 3810-193 Aveiro,Portugal.
RESUMO
Introdução: Nas últimas décadas, a sobrevivência na pre- maturidade extrema aumentou mas a morbilidade mantém-se significativa. Pretendemos avaliar se determinadas attitudes/ características se associam a um aumento da sobrevida e so- brevida sem sequelas major. Pretendemos também elaborar modelos de previsão do desfecho.
Material e Métodos: Estudo observacional descritivo, in- cluindo os 205 nados-vivos/nados-mortos – 22s0d-26s6d- nasci- dos no Serviço de Obstetrícia ou transferidos para a Unidade de Neonatologia de um Hospital Nível III, de Janeiro-2000 a Dezem- bro-2009. Analisámos variáveis relativas ao período prénatal/ neonatal, desempenho dos recém-nascidos e desenvolvimen- to psicomotor(18-24 meses). As associações entre variáves/ desfechos foram identificadas através do teste chi-quadrado e teste-t; modelos de regressão logística foram elaborados para descrever e prever a mortalidade/morbilidade.
Resultados: A Idade Gestacional (IG) avançada (p=0.001), corticoterapia antenatal (p=0.001), cesariana(p=0.001), transfe- rência in-utero(p=0.021) e o maior peso(p=0.001) associam-se a aumento da sobrevivência. Ausência de hemorragia intraven- tricular (HIV) graus 3-4 (p=0.001) e de leucomalácia periven- tricular (LPV) (p=0.005) associam-se a aumento da sobrevida sem sequelas major. De acordo com os modelos construídos, o aumento da IG (OR=0.353,CI95% 0.208-0.599), do peso (OR=0.996,CI95% 0.993-0.999) e a corticoterapia antenatal (OR=0.150,CI95% 0.044-0.510) associam-se a diminuição do risco de mortalidade. Ruptura de membranas inferior a 12 horas associa-se a aumento de risco de mortalidade(OR=3.88,CI95% 1.406-10.680). HIV graus 3-4 associa-se a maior risco de morbilidade(OR=16.931,CI95% 2.744-104.452). Os modelos de mortalidade e morbilidade previram correctamente o desfecho em 78.1% e 85.7% dos casos, respectivamente.
Conclusões: Os modelos de mortalidade/morbilidade po- dem ser ferramentas importantes na previsão do desfecho dos recém-nascidos pré-termos extremos auxiliando o aconselha- mento parental.
Palavras-chave: Pré-termos extremos, desfecho, modelos, aconselhamento parental
ABSTRACT
Introduction: Over the last decades, survival of extremely preterm infants improved but there´s still signifi morbidity among this group. We pretend to evaluate if specifi attitudes/ characteristics are associated with higher survival or survival without severe disabilities and elaborate predicting outcome models.
Material and Methods: Observational descriptive study, including the 205 liveborn/stillborn infants -gestational age 22w0d-26w6d- born at an Obstetrics Unit or transferred to a Neonatology Unit of a Level III Hospital, from January-2000 to December-2009. We collected variables related to management in the prenatal/neonatal period, neonate performances and psychomotor development(18-24 months). Significant associations between variables/outcomes were identified by chi-square test or t-test; multivariate logistic regression models were used to describe and predict mortality/morbidity.
Results: Advanced Gestational Age (GA) (p=0.001), antenatal corticotherapy(p=0.001), cesarean section(p=0.001), inborn delivery(p=0.021) and increased weight(p=0.001) were associated with survival. Absence of Intraventricular Hemorrhage (IVH) grade 3-4(p=0.001) and absence of Periventricular Leukomalacia (PVL) (p=0.005) were associated with survival without severe neurossensorial deficit. According to multivariable models, advanced GA (OR=0.353,CI95% 0.208- 0.599), increased weight (OR=0.996,CI95% 0.993-0.999) and antenatal corticotherapy (OR=0.150,CI95% 0.044-0.510) were associated with lower mortality risk. Rupture of membranes less than 12 h duration was associated with higher mortality risk (OR=3.88,CI95% 1.406-10.680). IVH grades 3-4 was associated with higher morbidity risk (OR=16.931,CI95% 2.744-104.452). Mortality and severe morbidity models predicted correctly the outcome in 78.1% and 85.7% of the cases, respectively.Conclusions: Mortality/morbidity models might be valuable tools providing insight in the prediction of the outcome of these neonates and helping parental counseling.
Keywords: Extremely preterm, outcomes, models, parental counseling
INTRODUCTION
Survival of preterm neonates has progressively improved over the last decades1-7. The gestational age (GA) at which half of the neonates survive has decreased from 30-31weeks (w)in 1960 to 23-24w at this point1 due to improvements in obstetric and neonatal care, such as the generalized use of antenatal corticotherapy and surfactant. There has been also an improvement in the neurodevelopmental outcome of the extremely premature infants, however, it was significantly lower than the increase in survival and there is still significant morbidity among these children1,2,4-7. Nowadays, survival with less than 23w gestation is extremely unlikely and most of the health care providers consider that only comfort care is reasonable. With 25w, a significant number of the newborns survive without cerebral palsy or severe neurossensorial deficits and clinicians accept that full resuscitation is indicated for the overwhelming majority of these neonates. Between 22 and 25w some authors defined the gray zone, where infants will probably survive but the uncertainty of the outcome is the rule1. We examined our series of preterm infants under 27w gestational age over a 10 year period concerning clinical management in the prenatal/neonatal period, infant performances and psychomotor development at 18-24 months corrected age. We also evaluated if specific attitudes (namely therapy with antenatal steroids, mode of delivery and iatrogenic delivery) or characteristics explained higher rates of mortality and morbidity (survival with long-term severe disabilities). Our goal is to provide some insight in the prediction of the outcome of these preterm neonates.
MATERIAL AND METHODS
A observational descriptive study was conducted in which were included all liveborn and stillborn infants that were born in the Obstetric Unit, or transferred to the Neonatology Intensive Care Unit of a Level III Hospital, with GA 22w0 days to 26w6 days, from January 2000 to December 2009. Terminations of pregnancy and infants with congenital malformations were excluded.
Data were obtained from the Neonatology Database of Extreme Prematurity and from mothers and infants clinical charts. We collected variables related to mothers intrinsic characteristics, obstetric surveillance of pregnancy, clinical interventions before and during labor, management on postnatal period, infants performances, and psychomotor development at 18-24 months of corrected age.
After maternal age median determination, maternal age was classified into 4 categories: younger than 20 years old; 20 to 34 years old; 35 to 39 years old; and above the age of 39.
Variables related to mothers characteristics – primiparae, pregnancy surveillance, multifetal gestation – and related with neonatal period – antenatal steroids, iatrogenic delivery, vaginal delivery, stillbirth, small for gestational age, intubation, 5min. Apgar score ≤3, one year survivor were addressed in two categories – yes or no. Antenatal corticotherapy was defined as one or two doses of betamethasone, and iatrogenic delivery as the delivery occurring due to maternal or fetal pathology, either after induction of labor or after cesarean section.
Gender was assigned as male or female and Birth location was recorded in the following categories: Inborn, Other Level III hospital, Level I-II hospital and Home.
GA was recorded in completed weeks. The method used to determine it (either by the last menstrual period or by ultrasound) was not specified. Weight was also studied as a continuous variable. Were considered small for GA, the newborns whose weight was below the 10th percentile.
Hyaline membrane disease (HMD) was defined as respiratory distress syndrome due to primary surfactant deficiency; bronchopulmonary dysplasia (BPD) as oxygen dependence at 36 gestacional weeks or persistent oxygen dependency up to 28 days of life ; according to Papile classification, intraventricular hemorrhage (IVH) grade 3 as that occurring with ventricular dilatation, and grade 4 as that with intraparenchymal hemorrhage; periventricular leukomalacia (PVL) as ischemic brain injury due to prematurity based on De Vries Classification. Both HMD, BPD, no IVH, IVH grades 1-2, IVH grades 3-4, PVL, Persistent Ductus Arteriosus (PDA) and Infection were addressed in two categories – yes or no.
Mortality was defined as death occurring from 22w of GA forward, including stillbirths. It was further divided in early neonatal death (if occurred in the first 7 days of life), late neonatal death (between 8 and 28 days of life) and postneonatal death (if after that period).
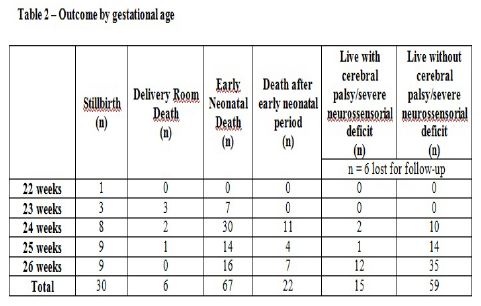
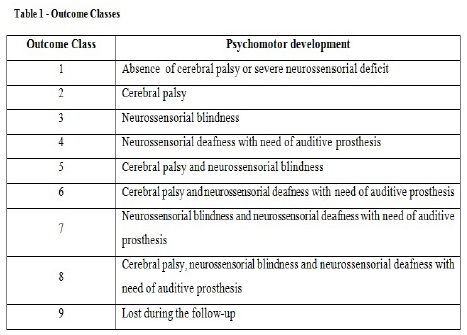
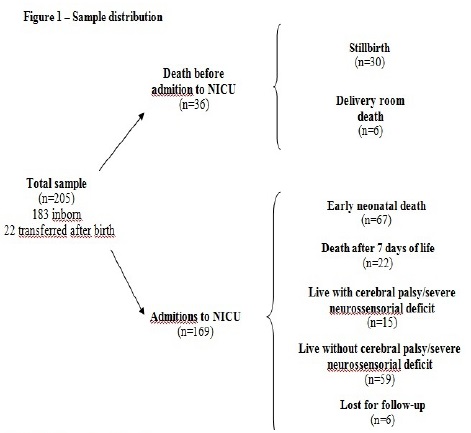
The newborns were classified into 6 classes of outcome: 1) Stillbirth; 2) Delivery room death; 3) Early neonatal death; 4) Death after 7 days of life; 5) Live with cerebral palsy or severe neurossensorial deficit; 6) Live without cerebral palsy or severe neurossensorial deficit. The inclusion in the two last classes was possible because infants were classified according to their psychomotor development at 18-24 months of corrected age (Table I). Cerebral palsy was defined according to the European Surveillance of Cerebral Palsy Network as a disorder of the development of movement and posture causing activity limitation that is attributed to non progressive disturbance in infant brain.
Legal and ethical considerations had been approved by the Institution Research Ethical Committee.
Significant associations (p <0.05) between variables and outcomes were identified by chi-square test or t-test, and multivariable logistic regression models were used to describe and predict mortality and morbidity. Estimates for both models are expressed as odds ratios with 95% confidence intervals. The statistical analysis was conducted with SPSS Statistics 17.0 software.
RESULTS
Over the 10 year period considered, 33 638 deliveries occurred in our institution, 183 (0.54%) before 27w gestation. In the same period, there were 4 245 admissions to Neonatology Intensive Care Unit, 169 (3.98%) of infants born before that GA.
We obtained a sample of 205 newborns: 183 delivered at our institution and 22 admitted alive after birth outside our hospital as shown in Figure1. Six infants were excluded from the psychomotor development analysis because they were lost for the follow-up after the first year of life.
The sample had the following distribution by GA: 0.5% (n=1) with 22w, 6.3% (n=13) with 23w, 31.2% (n=64) with 24w, 21.5% (n=44) with 25w; and 40.5% (n=83) with 26w; 175 (85.4%) born alive.
The median maternal age was 28 years (range, 15- 45 years); 8.0% (n=16) younger than 20 years old; 81.4% (n=162) 20 to 34 years old; 10.1% (n=20) 35 to 39 years old; and 0.5% (n=1) above the age of 39. There were 52% (n=103) of primiparae and 8.0% (n=16) of pregnancies without regular surveillance.
There were 32.2% (n=66) of infants from multiple gestations; antenatal corticotherapy was administered in 73.2% (n=150) of gestations, with a trend to increase with gestational age; of all infants, 9.9% (n=20) were born after iatrogenic delivery and 51.5% (n=105) after cesarean section. Most of the newborns, 89.3% (n=183), were born at our institution. The others were born at another Level III Hospital (2.0%, n=4), at another Level I-II hospital (7.8%, n=16) or at home (1.0%, n=2).
Of all infants, 57.6% (n=118) were male. There were 12.2% infants small for gestational age and the mean birthweight was 743g ±162g. For those who born alive, low Apgar score (5min. Apgar score ≤3) was found in 11.2% (n=19) newborns, with a trend to decrease with increasing GA. Intubation at birth was needed in 69.7% (n=122), and 86.3% (n=151) received surfactant in Neonatology Intensive Care Unit.
The overall mortality was 60.9%, ranging from 100% at 22w to 33.7% at 26w. There were 14.6% (n=30) stillborn and 2.9% (n=6) infants with delivery room death. From all sample, 32.7% (n=67) died in the first seven days of life, and 10.7% (n=22) after that period (Figure 1 and Table 2). If we consider only the 169 infants admitted to NICU, the same as excluding stillbirths and delivery room deaths, the mortality rate was 52.7%.
In the univariable analysis, advanced GA (p=0.001), antenatal corticotherapy (p=0.001), cesarean section (p=0.001), inborn delivery (p=0.021) and increased weight (p=0.001) were associated with survival. However, considering infants with the same GA, only at 26w gestation the increase in this last variable was associated with an increase in survival.
Considering the morbidity in the postnatal period of all infants admitted to Neonatology Intensive Care Unit, we found HMD in 90.2% (n=147), BPD in 36.8% (n=60), IVH grade 3-4 in 30.1% (n=49); PVL in 3.7% (n=6), PDA in 38.7% (n=63) and infection, including necrotizing enterocolitis, in 55.2% (n=90). Considering only the infants that survived the first year of life, we found an increase in the prevalence of HMD, BPD, PDA and infection. IVH grade 3-4 and PVL decreased in this group of infants. If we consider only infants alive at the age of the follow-up (n=74, 6 lost for follow-up), 79.7% (n=59) had nor cerebral palsy nor severe neurossensorial deficit (Table 2). In this group, we found even lower incidence of IVH grade 3-4 and PVL (8.2% and 0%, respectively). In the univariable analysis, the absence of these two ultrasound markers was associated with this outcome at the age of 18-24 months (p=0.001 and p=0.005 respectively).
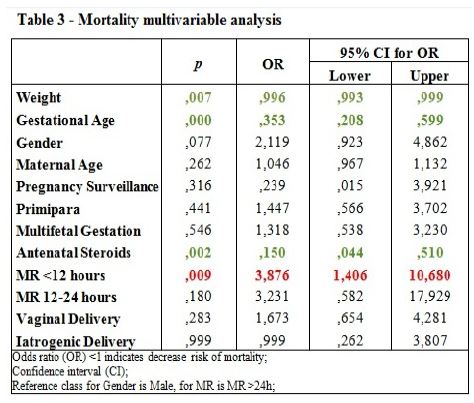
The mortality model was obtained by multivariable logistic regression considering 11 prenatal variables (Table 3). Advanced GA (OR=0.353; 95% CI=0.208 to 0.599; p=0.001), increasing weight (OR=0.996; 95% CI=0.993 to 0.999; p=0.007) and antenatal corticotherapy (OR=0.150; 95% CI=0.044 to 0.510; p=0.002) were associated with lower mortality risk while membranes rupture (MR) of less than 12h was associated with increased mortality risk (OR=3.876; 95% CI=1.406 to 10.680; p=0.009).
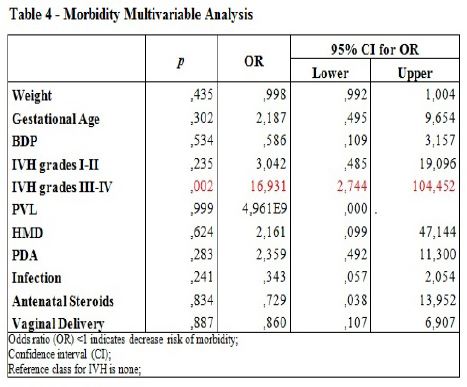
Likewise, the logistic regression model built to describe and predict morbidity at 18-24 months of corrected age was based on 10 variables (Table 4). The presence of IVH grade 3 and 4 was associated with higher morbidity risk (OR=16.931; 95% CI=2.744 to 104.452; p=0.002), while no other variables were found significant probably due to the very small sample size.
Hosmer-Lemeshow test for the goodness of fit of the multivariable models indicated that both models are suitable for these data (p=0.194 for mortality and p=0.289 for morbidity), and the large Nagelkerkes R2 values indicated that the models explain a substantial amount of proportion of mortality/morbidity variance (R2=52.6% for mortality and R2=42.4% for morbidity). Therefore, these multivariable models are expected to predict adequately mortality/ morbidity in extremely premature newborns. In fact, the models predicted correctly mortality outcome in 78.1%, and severe morbidity in 85.7% of the cases.
DISCUSSION
The relevance of our work is related to the construction of outcome predicting tools which assume an important role in parental counseling, since as suggested by other authors, this counseling must be based on local data8. When dealing with infants in the limit of viability, continuous reassessing of clinical situation and management options discussion with parents is necessary. Most of the times those options include withholding or withdrawal of life support and should be based on accurate survival and disability rates. These models reflect the results of our units in a period of ten years, in which medical resources were the same as nowadays, and showed high levels of accuracy predicting both survival and survival without major disabilities (more accurate than predicting randomly or assigning the same outcome to all infants). The next step would be the application of the models to a new sample of newborns. Moreover, our work can be helpful in elucidating the professionals of our institution and our country, about our own outcomes since many professionals are not aware of these kind of data6 and according to Blanco et al. health care providers often underestimate survival and overestimate long-term impairment rates9. With this work we actually can improve our medical practice, particularly concerning parental counseling, since medical management is well defined in published guidelines.
According to guidelines concerning management of extreme premature fetus/newborns, full investment is only justified from 24w forward. Our results reflect and reinforce that conduct and are in accordance with other published works, particularly those from Central Europe8. The full investment in advanced gestational ages is illustrated by the trend in greater use of corticotherapy with advanced GA.
It is important to consider the weight of multifetal pregnancies in this sample – one third of all sample. Control of outcomes in assisted reproductive techniques may play an important role preventing mortality and morbidity associated to extreme prematurity.
Another important aspect concerning extreme preterm infants is the lack of value for the Apgar score. This aspect is well illustrated with our data. We find 5 min. Apgar score ≤3 in 11.2% of the sample, a much lower than mortality.
The role of advanced GA, increasing weight, antenatal corticotherapy and inborn delivery in increasing survival is well documented1,2,4,7,8. Similarly, association between absence of IVH grades 3 and 4 and survival without major disabilities is also described in numerous papers2,5.
Concerning cesarean delivery, this was associated with an increase in survival only in the univariable analysis, probably reflecting the benefits of cesarean section only in specific scenarios3,4, as lower GA, multiple pregnancies, breech presentations and growth restricted fetuses between 26 and 30 weeks. Another interesting finding is the relationship between mortality and the duration of MR. MR of less than 12 hours was associated in the multivariable analysis with increased mortality, probably in relation with incomplete cicle of corticotherapy for lung maturation or precocious interruption of pregnancy due to other complications such as infection, which also play an important role in unfavorable outcomes.
Although our sample is composed of 205 infants (with small number of neonates with lower GA) we include stillbirths and delivery room deaths, an advantage in the understanding of the outcomes of pregnancies in the gestational ages considered, but also a bias in mortality assessment since we don´t include stillbirths and delivery room deaths from the institutions that transferred their extremely preterm infants to us.
Among the limitations of this study, we consider the uncertainty in the method of assessment of GA which reinforce the opinion of some authors who consider the GA an unreliable data3; it is also a single institution study, which may add selection bias and clinicians bias in treatment decisions; and the short period of follow-up since even those infants without cerebral palsy or severe neurossensorial deficits, may reveal cognitive deficits at school age and cardiovascular co morbidities such as hypertension or diabetes later in life2.
Conclusions
Since management of extreme preterm infants should be based on local data or data from other units in the same country, we think our work can help other professionals in their daily management with patients at high risk of extremely preterm labor.
IN FOCUS
- Parents counseling in extremely low gestational ages is important so their involvement in decisions related to withholding or withdrawal of life support be based on local and realistic data;
- We present our mortality and morbidity rates for infants under 27w gestational age, as well as models to predict the outcomes, both for mortality and morbidity;
- These models might be valuable tools for parental counseling;
EM DESTAQUE
- O aconselhamento parental nas idades gestacionais da prematuridade extrema é fundamental para que o
envolvimento dos pais nas decisões de manutenção de medidas de suporte de vida, ou instituição de cuidados paliativos, seja baseado em dados locais e realistas;
- Apresentamos as nossas taxas de mortalidade e morbilidade para recém-nascidos com idade gestacional inferior a 27 semanas, assim como modelos de previsão do desfecho, tanto de mortalidade como de morbilidade;
- Estes modelos podem ser ferramentas úteis no aconselhamento parental;
DECLARATION OF INTERESTS
The authors don´t have any conflict of interests to declare.
There was no involvement of any pharmaceutical company or other sponsor funding our work, nor any assistance by medical writing or editorial company.
REFERENCES
1. Seri I, Evans J. Limits of viability: definition of the gray zone. Journal of Perinatology 2008;28:S4-8. [ Links ]
2. The EXPRESS Group. One-Year Survival of Extremely Preterm Infants After Active Perinatal Care in Sweden. Journal of American Medical Association 2009;301(21):2225-33. [ Links ]
3. Kaiser J, Tilford JM, Simpson PM, Salhab WA, Rosenfeld CR. Hospital Survival of Very-Low-Birth-Weight Neonates from 1977 to 2000. Journal of Perinatology 2004;24:343-50. [ Links ]
4. Wang Y, Tanbo T, Ellingsen L, Abyholm T, Henriksen T. Effect of pregestational maternal, obstetric and perinatal factors on neonatal outcome in extreme prematurity. Arch Gynecol Obstet 2011;404-011:1870-5. [ Links ]
5. Bodeau-Livinec F, Marlow N, Ancel PY, Kurinczuk JJ, Costeloe K, Kaminski M. Impact of Intensive Care Practices on Short-Term and Long-term Outcomes for Extremely Preterm Infants: Comparison Between the British Isles and France. Pediatrics 2008;122:e1014-21. [ Links ]
6. Lorenz JM, Wooliever DE, Jetton JR, Paneth N. A Quantitative Review of Mortality and Developmental Disability in Extremely Premature Newborns. Arch Pediatr Adolesc Med 1998;152:425-35. [ Links ]
7. Vento M, Cheung PY, Aguar M. The First Golden Minutes of the Extremely-Low-Gestational-Age Neonate: A Gentle Approach. Neonatology 2009;95:286-98. [ Links ]
8. Berger T, Bervet V, Alama SE, Fauchère JC, Hosli I, Irion O, et al. Perinatal care at the limit of viability between 22 and 26 completed weeks of gestation in Switzerland. The European Journal of Medical Sciences 2011;141:w13280. [ Links ]
9. Blanco F, Suresh G, Howard D, Soll RF. Ensuring Accurate Knowledge of Prematurity Outcomes for Prenatal Counseling. Pediatrics 2005;115:e478-87. [ Links ]
10. Marlow N, Wolke D, Bracewell MA, Samara M. Neurologic and Developmental Disability at Six Years of Age after Extremely Preterm Birth. The New England Journal of Medicine 2005;352,1: 9-18. [ Links ]
11. Pignotti MS, Donzelli G. Perinatal Care at the Threshold of Viability: An International Comparison of Practical Guidelines for the Treatment of Extremely Preterm Births. Pediatrics. 2008;121,1:e193-8. [ Links ]
12. Field DJ, Dorling JS, Manktelow BN, Draper ES. Survival of extremely premature babies in a geographically defined population: prospective cohort study of 1994-9 compared with 2000-5. British Medical Journal 2008;online edition:1-4. [ Links ]
13. Kent AL, Casey A, Lui K. Collaborative decision-making for extreme premature delivery. Journal of Paediatrics and Child Health. 2007;43:489-91. [ Links ]
14. Kaempf JW, Tomlinson MW, Campbell B, Ferguson L, Stewart VT. Counseling pregnant women who may deliver extremely premature infants: Medical care guidelines, family choices and neonatal outcomes. Pediatrics 2009;123,6:1509-15. [ Links ]
15. Keogh J, Sinn J, Hollebone K, Bajuk B, Fischer W, Lui K. Delivery in the grey zone: Collaborative Approach to extremely preterm birth. Australian and New Zealand Journal of Obstetrics and Gynaecology 2007;47:273-8. [ Links ]
16. Secção de Neonatologia da Sociedade Portuguesa de Pediatria. Consensos em Neonatologia. 2004. [ Links ]
17. Guillén U, Suh S, Munson D, Posencheg M, Truitt E, Zupancic JAF, et al. Development and Pretesting of a Decision-Aid to Use When Counseling Parents Facing Imminent Extreme Premature Delivery. The Journal of Pediatrics 2012;160,3:382-7. [ Links ]
18. Schroeder J. Ethical issues for parents of extremely premature infants. Journal of Paediatrics and Child Health 2008;44:302-4. [ Links ]
19. Kaempf JW, Tomlinson M, Arduza C, Anderson S, Campbell B, Ferguson LA, et al. Medical Staff Guidelines for Periviability Pregnancy Counseling and Treatment of Extremely Premature Infants. Pediatrics 2006;117,1:22-9. [ Links ]
20. Savage TA, Kavanaugh K. Resuscitation of Extremely Preterm Infant: a Perspective from the Social Model of Disability. Newborn and Infant Nursing Reviews 2004;4,2:114-20. [ Links ]
21. Chan KL, Kean LH, Marlow N. Staff views on management of the extremely preterm infant. European Journal of Obstetrics and Gynecology and Reproductive Biology 2006;128:142-7. [ Links ]
Endereço para correspondência
Maria Isabel Sá
Av. do Bessa, 216 - Entrada1 - 9º centro 4100-012 PORTO
E-mail: misabelrcsa@gmail.com Phone: 919 195 922
Recebido a 28.04.2014 | Aceite a 10.12.2014