Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Nascer e Crescer
versão impressa ISSN 0872-0754
Nascer e Crescer vol.23 no.1 Porto mar. 2014
CASOS CLÍNICOS / CASE REPORTS
Gradenigo syndrome: an unexpected otitis complication
Síndrome de Gradenigo: uma complicação inesperada da otite
Catarina MendesI; Cristina GarridoI; Margarida GuedesI; Laura MarquesI
IS. Pediatria, CH Porto, 4099-001 Porto, Portugal. E-mail: catarinamendes@gmail.com; cgarridopt@gmail.com; margguedes@gmail.com; laurahoramarques@gmail.com
RESUMO
Introdução: O síndrome Gradenigo (também conhecido como petrosite apical) é uma tríade clínica definida por otite média, nevralgia do trigémeo e parésia ipsilateral do nervo abducente. Desde o advento da antibioterapia, passou a ser uma complicação rara da otite média aguda mas potencialmente fatal, requerendo diagnóstico e tratamento atempados.
Caso clínico: Criança do sexo feminino, com sete anos de idade e história prévia de otite, com quadro de otalgia, cefaleia, diplopia e febre. Foi feito o diagnóstico de síndrome de Gradenigo e instituída antibioterapia de amplo espectro e miringotomia com colocação de tubos de ventilação transtimpânicos. A evolução clínica foi favorável.
Conclusão: Este caso documenta o sucesso terapêutico e a recuperação total de uma criança imunocompetente com síndrome de Gradenigo com recurso a uma abordagem conservadora.
Palavras-chave: Gradenigo, otite média, petrosite.
ABSTRACT
Introduction: Gradenigo syndrome (also known as apical petrositis) is a clinical triad of otitis media, trigeminal neuralgia and ipsilateral abducens nerve palsy. In the era of antibiotic therapy, it is an exceptional but potentially life threatening complication of acute otitis media, requiring prompt diagnosis and treatment.
Case report: A seven-year-old girl with previous history of otitis, presented with left ear pain, headache, diplopia and fever. Diagnosis of Gradenigo syndrome was established and she was treated with systemic broad-spectrum antibiotics and myringotomy with timpanostomy tube placement. Clinical outcome was favourable.
Conclusion: This case documents therapeutic success and total recovery with a conservative approach in an immunocompetent child with Gradenigo syndrome.
Key-words: Gradenigo, otitis media, petrositis.
INTRODUCTION
Gradenigo syndrome, first described in 1907 by Giuseppe Gradenigo, is characterized by the clinical triad of acute otitis media, facial pain in the fifth cranial nerve distribution and ipsilateral abducens nerve palsy.(1) It is a serious complication of acute otitis media and mastoiditis, although increasingly rare due to wide antibiotic availability, and results of direct extension of the infectious process into the petrous apex.(2) Cranial nerve dysfunction is caused by osteitis and local leptomeningitis near the petrous apex. In that location, the trigeminal nerve ganglion and the abducens nerve lie closely together, making them vulnerable to any local inflammatory process.(2,3) Infections in the petrous apex can be life threatening, given their propensity to spread medially and to involve meninges, cavernous sinus and brain.(3)
Acute petrositis diagnosis requires imaging studies, namely, computed tomography (CT), magnetic resonance imaging (MRI) or nuclear imaging techniques, to identify the petrous apex as the site of the inflammatory process.(3) The treatment of Gradenigo syndrome is not consensual and should be managed on an individual basis.(4)
CASE REPORT
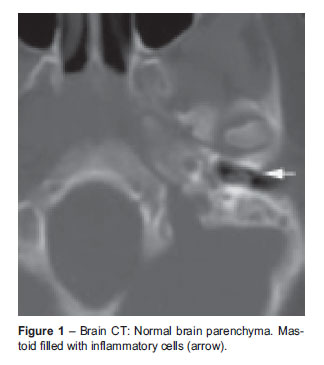
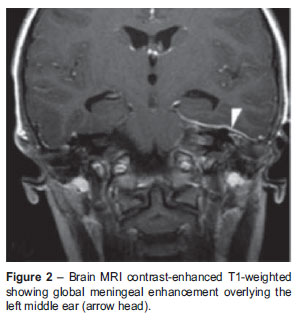
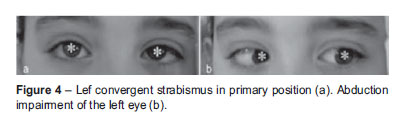
A seven-year old caucasian girl was admitted to our hospital for meningitis and acute onset strabismus. The patient had previous history of acute otitis media (about one or two episodes per year), the last one occurring the previous month. She had been examined seven days before for left otalgia, without fever or any other complaints and was discharged with symptomatic treatment. On admission day, she complained of diplopia, photophobia and left facial pain; left strabismus was noticed. On physical examination, she presented fever, meningeal signs and left acute otitis media without clinical signs of mastoiditis. Left convergent strabismus was evident with abduction impairment of the same eye. Brain CT scan showed inflammatory changes of the sphenoidal sinus and both mastoid cavities; brain parenchyma was normal, no deviation from the midline structures was found and cerebrospinal fluid spaces showed no signs of hydrocephaly (Figure 1). Laboratory tests revealed elevated inflammatory parameters, with a white blood cell count of 18.500/mm3, polymorphonuclear neutrophils of 15.000/mm3 and C-reactive protein of 317 mg/L. Lumbar puncture revealed cloudy cerebrospinal fluid (CSF), with cytochemical examination showing pleocytosis (736 cells, 91% polymorphonuclear and 3% of mononuclear cells), hypoglycorrhachia (0,09 g/L) and hyperproteinorhachia (3,18 g/L). A single dose of dexamethasone was administered and intravenous antibiotic treatment with ceftriaxone (100 mg/kg) and vancomycin (60 mg/kg) was started. Brain MRI (Figure 2) found global meningeal enhancement, in particular within the region overlying the left middle ear, suggesting an inflammatory/infectious process centred in the left ear, with extension into the cranial cavity. Venous sinus thrombosis was excluded.
On second day of admission, the patient was submitted to a left myringotomy with tympanostomy tube placement, with relief of pain complaints.
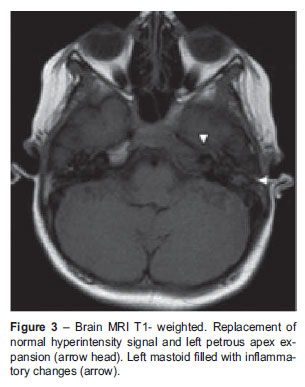
On CSF, Staphylococcus capitis was isolated and interpreted as a probable contaminat; Herpes simplex virus 1,2 and Enterovirus were negative. Polymerase chain reaction for Mycobacterium tuberculosis and Streptococcus pneumoniae and Borrelia burgdoferi serology were negative. Blood culture proved sterile and ear pus culture revealed commensal flora. Adenosine deaminase serum levels and Interferon-gamma release assay were within normal ranges. Tuberculin test was negative and chest x-ray showed no pathological signs. A second MRI was performed after three weeks of initial symptoms, showing the left mastoid filled with inflammatory changes, left petrous apex expansion and adjacent pachymeningeal enhancement, features suggestive of apical petrositis (Figure 3). Inflammatory changes had no apparent extension to the cavernous sinus or Gasser ganglion cistern. These findings confirmed Gradenigo syndrome.
The child received thirty-three days of intravenous ceftriaxone and vancomycin, with clinical and radiological improvement. There was a gradual improvement of the abducens paresis. By the time she was discharged her left eye abduction was still impaired to about one third of total width (Figure 4). Cefuroxime axetil (30 mg/kg) was continued for eight weeks along with eyealternating occlusion, initiated on admission. Full recovery of the strabismus was achieved by the time she ended antibiotic therapy and no hearing loss was noticed. Immunoglobulin IgA, IgG, IgM, IgE, specific IgG antibody levels for Pneumococcal capsular polysaccharide and Tetanus toxoid were normal. HIV test was negative. During the 4-month follow-up period, no further complications occurred.
DISCUSSION
Gradenigo syndrome affects about two in every 100.000 children with otitis media.(5) It can, however, be fatal.(3,4) The petrous apex contains a pneumatized cell system that communicates with the middle ear; when inflammation occurs, its mucosa becomes thickened causing petrous apex obstruction. Inflammation spread can lead to meningitis, empyema, brain abscess, venous thrombosis, cranial nerve paralysis and internal carotid artery stenosis.(3-8) Time lapse between otological symptoms and cranial nerve dysfunction varies from 1 to 12 weeks.(2,7) Radiologic imaging is essential to petrositis diagnosis, allowing staging and exclusion of other diagnosis, namely septic sinus thrombosis, tumours or aneurisms.(4,7) Therefore, any child presenting with acute otitis media with suspected intracranial complication, should undergo imaging testing.(7) CT scan is the first choice of imaging, since it is widely available and detects changes in bone structures, including destruction of trabecular bone and erosion of the petrous apex.(4,9) MRI is more sensitive in detecting dural thickening and enhancement as well as intracranial complications. An MRI angiography may be performed to rule out signs of sinus thrombosis.(9)
In this case, anamnesis and imaging studies revealed consistent findings of acute petrositis. The time interval between otitis onset and cranial nerves dysfunction (left facial pain and VI pair paresis) was seven days. As reported in the literature, this period probably reflected the infection extension into meninges and apex.(2,7) Despite thorough workup no agent was identified. Exclusion of meningeal tuberculosis and Lyme disease was paramount, because of cranial nerve involvement and meningitis without significant CSF growth. The fact that an apparently healthy child developed such a serious and rare complication is surprising. Reviewing Gradenigos cases recently described in the literature it appears that affected children had either unremarkable previous medical history or previous recurrent ear infections only.(2-8) This child was investigated for immunodeficiency and no abnormalities were found. HIV infection was also excluded.
Therapeutic management of Gradenigo syndrome is controversial and challenging. Antibiotics will usually treat the infection before dural involvement, hence Gradenigos cases are currently rare.(2,3,7,10) Although early reports advocate the need for radical surgery, recent cases have shown positive results with a conservative approach, with medical treatment and minimal surgical intervention (namely antibiotics, steroids and myringotomy with ear tube placement).(2-4,7,8) Medical treatment should include broad-spectrum intravenous antibiotics, targeted at common agents involved in bacterial mastoiditis (Staphylococcus aureus, Streptococcus pneumoniae, Streptococcus pyogenes and Pseu- domonas aeruginosa); anaerobic organisms can also be considered.(9,10) Aggressive surgery (mastoidectomy) is recommended when conservative therapy fails, despite suitable antibiotic therapy; when there is an obvious middle ear chronic pathology or within the presence of potentially fatal complications.(2,3,7)
In this case, a conservative approach was proposed and the patient was managed with broad-spectrum intravenous antibiotics and myringotomy with timpanostomy tube placement. There was a clinical and analytical favourable outcome and absence of coalescence or bone resorption. Although an optimal treatment duration has not yet been established, in recent cases the treatment period ranged from 3 to 5 weeks.(3,4,7) Our patient showed immediate pain relief and fever resolution after surgery and antibiotic therapy was started. Abducens palsy showed slow improvement, therefore antibiotic therapy was sustained until she fully recovered.
REFERENCES
1. Gradenigo G. Über die paralyse des nervus abducens bei otitis. Arch Ohrenheilk 1907; 774:149-87. [ Links ]
2. Marianowski R, Rocton S, Ait-Amer JL, Morisseau-Durand MP, Manach Y. Conservative management of Gradenigo syndrome in a child. Int J Pediatr Otorhinolaryngol 2001; 57:79-83. [ Links ]
3. Finkelstein Y, Marcus N, Mosseri R, Bar-Sever Z, Garty BZ. Streptococcus acidominimus infection in a child causing Gradenigo syndrome. Int J Pediatr Otorhinolaryngol 2003; 67:815-7. [ Links ]
4. Gibier L, Darrouzet V, Franco-Vidal V. Gradenigo syndrome without acute otitis media. Pediatr Neurol 2009; 41:215-9. [ Links ]
5. Goldstein NA, Casselbrandt ML, Bluestone CD, Kurs-Lasky M. Intratemporal complications of acute otitis media in infants and children. Otolaryngol Head Neck Surg 1998; 119:444-54. [ Links ]
6. Dorn M, Liener K, Rozsasi A, Keck T. Prolonged diplopia following sinus vein mimicking Gradenigos syndrome. Int J Pediatr Otorhinolaryngol 2006; 70:741-3. [ Links ]
7. Guedes V, Gallegos P, Ferrero A, García-Minúzzi M, Casanovas A, Georgetti B, et al. Gradenigos syndrome: a casereport. Arch Argent Pediatr 2010; 108:e74-e75. [ Links ]
8. Kong SK, Lee IW, Goh EK, Park SE. Acute otitis mediainduced petrous apicitis presenting as the Gradenigo syndrome: successfully treated by ventilation tube insertion. Am J Otolaryngol 2011; 32:445-7. [ Links ]
9. Luntz M, Brodsky A, Nusem S, Kronenberg J, Keren G, Migirov L, et al. Acute mastoiditis the antibiotic era: a multicenter study. Int J Pediatr Otorhinolaryngol 2001; 57:1-9. [ Links ]
10. Jacobsen CL, Bruhn MA, Yavarian Y, Gaihede M. Mastoiditis and Gradenigos Syndrome with anaerobic bacteria. BMC Ear, Nose and Throat Disorders 2012; 12:10. [ Links ]
Endereço para correspondência
Ana Catarina Barbedo Mendes
Centro Hospitalar do Porto
Largo Professor Abel Salazar
4099-001 Porto, Portugal
E-mail: catarinamendes@gmail.com
Recebido a 08.01.2013 | Aceite a 30.06.2013














