Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Portuguese Journal of Nephrology & Hypertension
versão impressa ISSN 0872-0169
Port J Nephrol Hypert vol.29 no.2 Lisboa jun. 2015
ORIGINAL ARTICLE
Corynebacterium species: an uncommon agent of peritoneal dialysis-related peritonitis and a challenging treatment
Corynebacterium species: um agente de peritonite raro em diálise peritoneal e um desafio terapêutico
Joel Ferreira, Fernando Teixeira e Costa, Aura Ramos
Department of Nephrology, Peritoneal Dialysis Unit, Hospital Garcia de Orta. Almada, Portugal
ABSTRACT
Introduction: Corynebacterium is a component of normal skin flora and it is responsible for an increasing incidence of nosocomial infections in the last decades. Peritonitis and exit-site infections caused by this microorganism are uncommon but have a significant clinical impact due to their high relapsing rate. The ideal therapeutic approach in these situations is not yet clearly defined. Methods: Retrospective analysis of Corynebacterium spp peritonitis in a peritoneal dialysis unit between 2006 and 2013 and characterization as to its frequency, treatment and clinical outcomes. Results: During the reporting period, nine patients (7.8%) had Corynebacterium peritonitis, accounting for a total of 18 episodes of infection caused by this microorganism. The majority of patients (55.6%) had more than one episode of Corynebacterium peritonitis, with a relapsing rate after the first episode of 22.2% and 33.3% repeat peritonitis cases. The relapsing rate was even higher after the second episode (33.3%). Five patients (55.6%) were treated with vancomycin and only one of them required antibiotic switch to linezolid because of hypersensitivity reaction; the same happened with one of four patients treated with cephalosporins. Cure was achieved in all cases and treatment duration was on average 17.9 days per episode. There was no need for catheter removal or peritoneal dialysis dropout, and we did not record any death related to peritonitis. Conclusions: The Corynebacterium peritonitis rate in our unit was high. The infection proved to be highly relapsing but with excellent response to antibiotics and without any adverse clinical outcome. Therefore, in relapsing and repeat peritonitis caused by this strain, one would recommend preservation of the dialysis catheter, and cure may be exclusively achieved with 14 to 21 days of antibiotic therapy with vancomycin or even cephalosporin.
Key -Words: Antibiotics; Corynebacterium; peritoneal dialysis; peritonitis.
RESUMO
Introdução: O Corynebacterium e um microrganismo da flora cutânea responsável por uma incidência crescente de infeções nosocomiais. As peritonites e infeções do orifício de saída do cateter de dialise peritoneal (DP) causadas por este agente sao raras, mas tem um impacto clinico significativo devido a altas taxas de recidiva. A abordagem terapêutica ideal nestas situações não esta claramente definida. Métodos: Analise retrospectiva das peritonites a Corynebacterium numa unidade de DP cronica entre 2006 e 2013 e caracterização quanto a sua frequência, tratamento e outcomes clínicos. Resultados: Durante o período analisado, 9 doentes (7,8%) apresentaram peritonite por Corynebacterium spp, registando-se um total de 18 episódios de infeção por esse microrganismo. A maioria dos doentes (55.6%) apresentou mais do que um episodio de peritonite, com uma taxa de recidiva apos o primeiro episodio de 22.2% e peritonite de repetição em 33.3% dos casos. A taxa de recidiva foi superior apos o segundo episodio (33.3%). Cinco doentes (55,6%) foram tratados com vancomicina e apenas um destes necessitou de alteração da antibioterapia para linezolide por reação de hipersensibilidade, o mesmo aconteceu com um dos quatro doentes tratados com cefalosporinas. Conseguiu -se a cura em todos os casos e a duração do tratamento foi em media de 17,9 dias/episodio. Em nenhum dos casos houve necessidade de remoção de cateter ou saída da técnica, nem se registou qualquer morte relacionada com a peritonite. Conclusões: A taxa de peritonite por Corynebacterium registada na nossa unidade foi elevada. A infeção caracterizou-se por ser frequentemente recidivante mas com excelente resposta a antibioterapia e sem outcomes clínicos desfavoráveis. Nas peritonites recidivantes e/ou de repetição causadas por este microrganismo, pode ser recomendada uma atitude mais conservadora quanto ao cateter de dialise, podendo a cura ser exclusivamente atingida com 14 a 21 dias de antibioterapia com vancomicina ou ate mesmo cefalosporina.
Palavras-Chave: Antibioticos; Corynebacterium; dialise peritoneal; peritonite.
INTRODUCTION
Peritonitis is a common complication of peritoneal dialysis (PD) and it is also a contributing factor to death in 16% of deaths related with PD1. Historically, coagulase - negative staphylococci, including Staphylococcus epidermidis, were considered one of the most frequent agents of peritonitis, and those episodes were generally related to connection or tubing contamination2. Improvements have been made, like use of Y systems or flush before fill, and this has substantially reduced the incidence of peritonitis caused by this kind of microorganism3.
The genus Corynebacterium includes a large group of mostly facultative anaerobes and gram-positive rods4. Non-diphtheria corynebacteria, like coagulase-negative streptococci, are major components of skin flora, and they are predominantly located deep in the hair follicle. Until recently, this agent was considered as non -pathogen in humans and was thought to be only a contaminant. However, in the past few decades there has been an increasing incidence of clinically significant infections caused by this microorganism, most of them were nosocomial and occurred not only in immunocompromised patients.
These include septicaemia, endocarditis, osteomyelitis, genitourinary and lower respiratory tract infections5.
Some of these infections are related mainly to the presence of medical devices, such as intravascular catheters, mechanical and biological valves, central nervous system drainage devices or orthopaedic prostheses6. On the other hand, there seems to be a seasonal variation in Corynebacterium peritonitis rate with a peak incidence in winter, possibly due to a decline in immune function that typically occurs in the general population in this season7.
Corynebacterium peritonitis and exit-site infections are uncommon, but have a relevant clinical impact as it has been associated with high recurrence rates, antibiotics resistance and need for catheter removal8.Data published to date in this area are scarce, and the optimal therapeutic strategy is not clearly defined. Herein we report the cases of Corynebacterium peritonitis registered in our PD unit and we have investigated their frequency, treatment, and major clinical outcomes.
SUBJECTS AND METHODS
We performed a retrospective analysis of all cases of Corynebacterium peritonitis in our peritoneal dialysis unit from 1 January 2006 to 31 December 2013.
Collected data included demographics (age and gender), chronic kidney disease aetiology, comorbidities, time from PD initiation until the first Corynebacterium peritonitis episode, previous history of other peritonitis, recent antibiotic therapy (≤ 3 months), laboratory data at presentation, effluent microbiology and treatment.
Peritonitis diagnosis was established according to standard criteria including clinical findings (abdominal pain and cloudy effluent), dialysate leukocytosis (> 100 cells/μL and > 50% neutrophils) and isolation of Corynebacterium from dialysate culture.
Peritonitis episodes were treated according to our unit protocol until bacteria were isolated in dialysate culture. It included: loading dose of intravenous (iv) 1g cefazolin plus 1g ceftazidime, followed by maintenance dose of intraperitoneal (ip) 125 mg/L cefazolin + 125 mg/L ceftazidime.
Antibiotic treatment was adjusted according to patient clinical response. We maintained cephalosporins in cases with favourable clinical and laboratory evolution; we changed it to vancomycin in the absence of improvement. Antimicrobial therapy was switched to linezolid in cases of hypersensitivity to vancomycin. Subsequent episodes (relapsing and repeat peritonitis) were treated with the same antibiotic that had successfully treated the first episode.
Antibiotics were administered intraperitoneally, according to the 2010 International Society for Peritoneal Dialysis guidelines on antimicrobial dosing recommendations: cefazolin 125 mg/L ip, in all exchanges, for continuous ambulatory peritoneal dialysis (CAPD) patients, and 20 mg/kg ip every day in long dwell for those on automated peritoneal dialysis (APD); loading dose of 30 -35 mg/kg of ip vancomycin, followed by maintenance dose of 15 mg/kg in long dwell every 3 to 5 days, according to vancomycin serum levels (target of > 15μg/mL). Linezolid was administered 200 mg q.d. orally. Treatment duration was empirical and conditional on each patient clinical course, but there was a trend to increase the duration of treatment in the third episode.
Analysed outcomes included incidence of relapsing and repeat peritonitis, peritonitis-related hospitalization, need for catheter removal, temporary or permanent haemodialysis transfer and patients death.
We also analysed changes in peritoneal transport pattern based on peritoneal equilibration tests, dialysis adequacy based on Kt/V, and changes in mesothelial cells mass by effluent Cancer Antigen 125 measurement and calculation of CA125 appearance rate. We considered the definitions established by the 2010 ISPD guidelines on peritoneal dialysis-related infections. We considered the peritonitis episode as cured after antibiotic therapy when the patient was symptom -free, the effluent remained clear and the episode was not followed by relapse, catheter removal or ended in patients death. We considered peritonitis -related death when it was directly attributable to peritonitis according to clinical criteria of the treating nephrologist.
RESULTS
During the analysed period, 116 patients were treated in our unit, and there were 102 episodes of peritonitis (0.41 episodes per patient -year). Nine patients (7.8%) had Corynebacteriumperitonitis with a total of 18 episodes of infection by this agent.
Baseline characteristics
The summary of the characteristics of the studied population is shown in Table 1. Patients were predominantly male (55.6%) with a mean age of 45.3 years (21 to 68 years). The aetiologies of chronic kidney disease were: autosomal dominant polycystic kidney disease (ADPKD) (two patients), nephroangiosclerosis (one), focal segmental glomerulosclerosis (FSGS) (one), chronic glomerulonephritis (one), reflux nephropathy (one), and unknown in three patients.
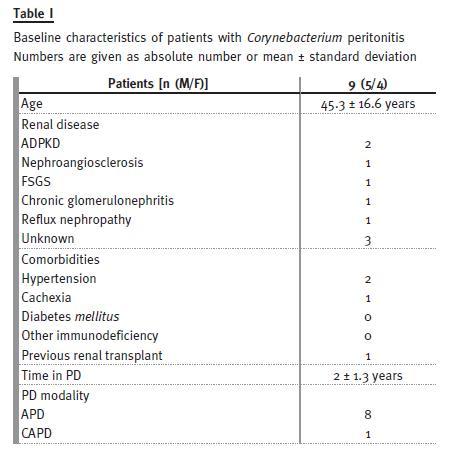
No patient was diabetic, two were hypertensive and one had had a previous kidney transplant. One had malnutrition in the context of chronic neurologic disease. With respect to dialysis modality, most of the patients were on APD. Patients were in dialysis for 0 to 4.3 years (one patient had an episode of peritonitis before the beginning of treatment, after catheter placement).
Clinical and laboratory data
Four patients (44.4%) had a previous history of peritonitis less than 3 months before the onset of Corynebacterium infection. Therefore, these four patients had been treated with antimicrobials within the last 3 months: two were treated with cefazolin because of taphylococcus epidermidis peritonitis; one with ciprofloxacin plus ceftazidime for Pseudomonas aeruginosa peritonitis; and one with ceftazidime plus cefazolin because of sterile peritonitis. Moreover, another patient experienced a Corynebacterium exit-site infection about 2 months before the occurrence of peritonitis and he was treated with 26 days of vancomycin with complete resolution of the infection.
Clinical presentation was totally non-specific since, in all cases, patients complained of abdominal pain, fever and cloudy effluent. The leukocyte count was an average of 7.3x109/L (4.8 to 10.3x109/L), C –reactive protein had an average value of 9.3 mg/dL (1.6 to 21.1) and the cell count in the peritoneal effluent averaged 2447/mm3.
Corynebacterium species has not been specified in most cases (66.7%). Three peritonitis were attributed to Corynebacterium striatum, 2 to Corynebacterium jeikeium and 1 to group G Corynebacterium. Antimicrobial susceptibility testing is not usually performed for these bacteria in our microbiology laboratory.Treatment and relapses
After establishing peritonitis diagnosis, all patients started antibiotics, according to the unit protocol, with cefazolin and ceftazidime for a variable number of days until obtaining the results of dialysate culture.
The performed treatment and clinical response are shown in Fig. I. Most patients (55.5%) showed more than one episode of Corynebacterium peritonitis, corresponding to a relapsing rate of 22.2% (n = 2) after the first episode and repeat peritonitis in 33.3% of cases (n = 3). Five patients had a second episode of peritonitis caused by this agent and the relapsing rate after second episode was even higher (33.3%, n = 3), with only one patient presenting repeat peritonitis. Relapsing and repeat peritonitis occurred respectively on average 23 ± 5.4 and 126 ± 94.6 days after the previous episode. The mean time to diagnosis of relapsing peritonitis did not change significantly after the first and second episode of peritonitis (21.5 versus 24 days).
Three patients continued therapy with cephalosporins and one of them had to switch to linezolid because of presumed hypersensitivity reaction. Based on the results of Szeto et al.9 who recommended the use of vancomycin instead of cephalosporins as treatment of choice, the other five patients were treated with vancomycin and one has needed switching to linezolid because of pruriginous skin rash, which was interpreted as an adverse allergic reaction to vancomycin.
Clinical outcomes
Cure was achieved in all cases and the duration of treatment was on average 17.9 days per episode.
There was no need for catheter removal or peritoneal dialysis dropout in any case. We only recorded one death unrelated to peritonitis and due to cachexia, which had also conditioned the single hospitalization in this set of patients. We did not record any major complication arising from the prolonged antibiotherapy and especially from the use of broad-spectrum antibiotics. Indeed, no patient presented any subsequent infection caused by a resistant strain or related to changes in commensal flora (e.g., pseudomembranous colitis or fungal infection).
We also reviewed the available data related to 7 peritoneal equilibration tests performed in five patients. In this small sample of patients, we did not identify any trend regarding changes in peritoneal transport pattern, dialysis adequacy, and mesothelial cell mass that could be related to these prolonged course infections.
DISCUSSION
Non-diphteria corynebacteria are relatively unusual agents of peritonitis in patients on chronic peritoneal dialysis. The rate of peritonitis recorded in our unit during the analysed period was high (8.8%) and higher than that described in other previous studies.
In a retrospective study performed in Hong Kong, over a period of 7 years and regarding 1485 episodes of peritonitis, only 1.8% was caused by Corynebacterium9.
A similar percentage of peritonitis caused by this agent (2.3%) was also identified in the ANZDATA registry database8.
Our sample was not large enough to allow any analysis of predictors of Corynebacterium infection.
In their study, Barraclough et al. have only identified a high body mass index as a predictor of peritonitis caused by this agent8. It was also suggested that the Corynebacterium tended to colonize the skin and became pathogenic after courses of broad spectrum antibiotics5. In our sample, less than half of the patients had been on antibiotics less than 3 months before the first episode of peritonitis, and vancomycin was used in only one case. There also seems to be no specific clinical or analytical data that could suggest infection by this strain.
Corynebacterium infection proved to be highly relapsing and the primary response rate was 44.4%.
No cure was achieved on the second episode. These results are inferior to those found in other studies, but the final cure rate was 100% exclusively with antibiotic treatment. Moreover, in contrast to other studies, relapse or repeat peritonitis appeared to be independent of the duration and type of antibiotics used. Indeed, Szeko et al. observed that relapse was more frequent after a 2-week course of antibiotics compared with a 3 week - course of intraperitoneal vancomycin9. These results were not confirmed in the Australian study, in which a 14 day-course of antibiotic appeared to be sufficient8. The mean duration of antibiotic therapy performed in our sample (17.9 days per episode) is consistent with this range of 2 to 3 weeks.
Like recurrent peritonitis caused by some other bacteria, these repeated episodes of Corynebacterium peritonitis raise the question of the possible role of biofilm in the occurrence of these infections. However, previous isolated reports have not confirmed the existence of biofilm on catheters removed from affected patients10, 11.
Given that, in most cases, the involved Corynebacterium species has not been specified, we cannot draw conclusions about the specific response to treatment of each one. However, it is known that the antibiotic susceptibility of Corynebacterium can vary, so an antimicrobial sensitivity testing is essential to determine the best treatment in each case12.
In a review on the identification and antibiotic sensitivity of 415 corynebacterial isolates in samples from hospitalized patients, Riegel et al. have demonstrated that many of the species were sensitive to ampicillin, cefotaxime and vancomycin13. In another review, vancomycin was shown to be the most active antibiotic against corynebacteria, and most strains had minimal inhibitory concentrations (MIC) below 1 mg/mL6. However, the C. jeikeium proved to be the most resistant species. In general, in the various types of Corynebacterium infection, the drug of choice seems to be vancomycin, since all corynebacteria are sensitive to this drug13. Interestingly cefazolin is not included within the cephalosporins, which have been tested in these various studies.
However, according to the results observed in our sample and data from the ANZDATA registry, cefazolin was found to be a good antibiotic for empirical and directed treatment in Corynebacterium peritonitis and its use, at the expense of vancomycin, may be beneficial in avoiding the emergence of resistant strains.
With regard to the main clinical outcomes in our sample, there were no hospitalizations, no need for catheter removal, PD dropout or peritonitis-related death. This demonstrates the indolent nature of this type of infection when treated properly. Data from other studies that focused on larger samples are not so positive. There are reports of 70% of hospitalizations, 21% of catheters removed because of refractory peritonitis, 7% and 15% of respectively temporary or permanent transfer to haemodialysis, and 2% of deaths8.
In the first cases of Corynebacterium peritonitis recorded in our PD unit, after the second episode of infection, it was decided not to remove the dialysis catheter, as advocated by Szeto et al.9. Since there were no relapses after the third episode and in the absence of complications related to repeated courses of antibiotherapy, the remaining patients were treated similarly.
CONCLUSIONS
In conclusion, Corynebacterium is a relatively uncommon cause of peritonitis but infections caused by this organism may have a significant clinical impact. The cure can be achieved in almost all cases exclusively with antibiotic treatment. However, prolonged therapy may be needed if there is occurrence of relapse or repeat peritonitis so we can preserve the peritoneal catheter. According to our experience, a 14 to 21 days course of antibiotherapy with vancomycin or even with a cephalosporin, such as cefazolin, is sufficient. An effort should be made in systematically identifying the involved Corynebacterium at species level and conducting antimicrobial susceptibility testing in all cases in order to optimize treatment response.
References
1. Li PK, Szeto CC, Piraino B, et al. with the International Society for Peritoneal Dialysis. Peritoneal dialysis -related infections recommendations: 2010 update. Perit Dial Int 2010; 30(4): 393 -423. [ Links ]
2. Piraino B, Bernardini J, Brown E, et al. ISPD position statement on reducing the risks of peritoneal dialysis-related infections. Perit Dial Int 2011; 31(6): 614 -630. [ Links ]
3. Grutzmacher P, Tsobanelis T, Bruns M, Kurz P, Hoppe D, Vlachojannis J. Decrease in peritonitis rate by integrated disconnect system in patients on continuous ambulatory peritoneal dialysis. Perit Dial Int 1993;13(Suppl 2):S326 -S328. [ Links ]
4. Schiffi H, Mucke C, Lang SM. Exit -site infections by non-diphteria corynebacteria in CAPD. Perit Dial Int 2004;24(5):454 -459. [ Links ]
5. Babay HA, Kambal AM. Isolation of coryneform bacteria from blood cultures of patients at a University Hospital in Saudi Arabia. Saudi Med J 2004;25(8):1073 -1079.
6. Lee PP, Ferguson DA Jr, Sarubbi FA. Corynebacterium striatum: an underappreciated community and nosocomial pathogen. J Infect 2005;50(4):338 -343. [ Links ]
7. Cho Y, Badve SV, Hawley CM, et al. Seasonal variation in peritoneal dialysis –associated peritonitis: a multi-centre registry study. Nephrol Dial Transplant 2012;27(5):2028-2036. [ Links ]
8. Barraclough K, Hawley CM, McDonald SP, et al. Corynebacterium peritonitis in Australian peritoneal dialysis patients: predictors, treatment and outcomes in 82 cases. Nephrol Dial Transplant 2009;24(12):3834-3839. [ Links ]
9. Szeto CC, Chow KM, Chung KY, Kwan BC, Leung CB, Li PK. The clinical course of peritoneal dialysis-related peritonitis caused by Corynebacterium species. Nephrol Dial Transplant 2005;20(12):2793-2796. [ Links ]
10. De Wit D, Mulla R, Burns A, Phelps RG. Tenchkoff catheter -associated peritonitis caused by Corynebacterium group I2. J Infect 1993;26(3):341-343. [ Links ]
11. Morris AJ, Henderson GK, Bremner DA, Collins JF. Relapsing peritonitis in a patient undergoing continuous ambulatory peritoneal dialysis due to Corynebacterium aquaticum. J Infect 1986;13(2):151-156. [ Links ]
12. Funke G, Von Graevenitz A, Clarridge JE 3rd, Bernard KA. Clinical microbiology of coryneform bacteria. Clin Microbiol Rev 1997;10(1):125159. [ Links ]
13. Riegel P, Ruimy R, Christen R, Monteil H. Species identities and antimicrobial susceptibilities of corynebacteria isolated from various clinical sources. Eur J Clin Microbiol Infect Dis 1996;15(8):657-662. [ Links ]
Dr. Joel Ferreira
Nephrology Department, Hospital Garcia de Orta
Avenida Torrado da Silva, 2801-951 Almada Portugal
E-mail: joel-ferreira@sapo.pt
Conflict of interest s tatement: None declared.
Received for publication: 27/07/2014
Accepted in revised form: 3/03/2015














