Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Portuguese Journal of Nephrology & Hypertension
versão impressa ISSN 0872-0169
Port J Nephrol Hypert vol.29 no.1 Lisboa mar. 2015
ORIGINAL ARTICLE
In-centre nocturnal haemodialysis: The experience of a centre
Hemodiálise nocturna: Experiência de um centro
Isabel Mesquita, Ana Vila Lobos, Helena Viana, Joao Lopes, Teixeira e Costa, Cristina Resina, Alexandra Guerra, Aura Ramos, Francisco Remedio
Diaverum – Unidade de Entrecampos. Lisbon, Portugal
ABSTRACT
Background and Objectives: As a result of improved clinical and quality-of-life outcomes, in-centre nocturnal haemodialysis emerges as one of the alternatives to conventional haemodialysis. Even today, little is known about the flow of patients through in-centre nocturnal haemodialysis programmes or about patients survival or technique failure. This study sought to address this gap in knowledge. Materials and Methods: Retrospective, descriptive study that included all patients in in-centre nocturnal haemodialysis programme, between January 1995 and December 2011, which involved 51 patients. Descriptive data at baseline were presented as means or percentages of the total. We used Kaplan–Meier survival curves for patient survival. Results: Patients underwent for more than 5.5 hours thrice weekly sessions and remained in the technique for a mean period of 59.5 ± 73 months. The annual input and output of patients in the programme was on average of to 2.1 and 2.5 patients, respectively. Forty-three patients discontinued the technique: kidney transplantation in 24, conventional haemodialysis in 11 and peritoneal dialysis in three patients, with mean times in in-centre nocturnal haemodialysis of 37.4 ± 46.4, 85.3 ± 93 and 59.7 ± 79.7 months, respectively. Throughout the period under review, five patients died (9.8%). Unadjusted survival at 20 years was 65% in patients who remained in in-centre nocturnal haemodialysis. Conclusion: In-centre nocturnal haemodialysis is associated with a higher survival rate, notwithstanding the possibility of selection bias resulting from patients profile that opts for this modality. The relative contribution of patient selection versus effect of therapy on outcomes requires evaluation in future prospective clinical trials.
Key-words: Chronic renal disease; flow patient technique; in-centre nocturnal haemodialysis; patient survival.
RESUMO
Introdução e Objectivos: Como consequência dos resultados da sobrevida e qualidade de vida, o programa de hemodiálise nocturna em centro surge como uma alternativa à hemodiálise convencional. Ainda hoje pouco se sabe sobre o fluxo de doentes, sobrevida e abandono da técnica. Este estudo pretendeu abordar essa lacuna no conhecimento. Métodos: Estudo descritivo de desenho retrospectivo que incluiu todos os doentes em programa de hemodiálise nocturna da clínica, entre Janeiro de 1995 e Dezembro de 2011. Foram avaliados 51 doentes. Os dados descritivos foram apresentados como médias ou percentagens do total. Foram utilizadas as curvas de Kaplan-Meier para a sobrevida dos doentes. Resultados: Os doentes realizaram sessões com duração maior ou igual a 5,5 horas 3 vezes por semana e permaneceram na técnica por um período médio de 59,5 ± 73 meses. A entrada e saída anual de doentes do programa foi em média de 2,1 e 2,5, respectivamente. Quarenta e três doentes mudaram de técnica: 24 por transplante renal, 11 para hemodiálise diurna e três para diálise peritoneal, com tempos médios de permanência de 37,4 ± 46.4, 85,3 ± 93 e 59,7 ± 79,7 meses, respectivamente. Durante todo o período em análise faleceram cinco doentes (9,8%). A sobrevida não ajustada aos 20 anos foi de 65% nos doentes que permaneceram em hemodiálise nocturna. Conclusão: A hemodiálise nocturna está associada a uma aumento da sobrevida, pese embora existir um viés de selecção resultante do perfil dos doentes que optam por esta modalidade. A contribuição relativa de selecção de doentes versus o efeito da técnica sobre os resultados necessita de avaliação em ensaios clínicos prospectivos.Palavras Chave: Doença renal crónica; fluxo de doentes; hemodiálise nocturna em centro; sobrevida dos doentes.
INTRODUCTION
The significant morbidity and mortality among longterm haemodialysis (HD) patients1,2 has increased the interest in more intensive dialysis regimens3. The Hemodialysis (HEMO) Study failed to show a significant benefit of high dialysis doses three times per week4.
These results renewed interest in the contribution of dialysis time (i.e., treatment duration) to outcomes in haemodialysis5,6. Home nocturnal haemodialysis (HNHD) and short-daily haemodialysis (SDHD) are the most extensively studied forms of intensified dialysis, although the actual cardiovascular and quality of life benefits of these modalities remain controversial7-10.
In-centre nocturnal haemodialysis (INHD) has emerged as a potential in-between SDHD and HNHD therapy by providing more flexibility for patients during the day and offering some of the shortcomings attributed to both SDHD and HNHD10. The INHD, which is typically administered thrice weekly for more than 5.5 hours (generally about 8 hours) per session in the dialysis unit during the overnight hours5,6, has emerged as a viable mechanism for the administration of intensified dialysis. It offers the theoretical advantages of prolonged dialysis with the benefits of nursing supervision and the non-disruption of productive daytime hours10.
In the last few years, better laboratory and patient outcomes have been observed in INHD compared with three times per week conventional haemodialysis (CHD)3,6,11-17.
In-centre nocturnal haemodialysis was instituted in our clinic in 1983 as a pioneer of this technique in Portugal. Even today, little is known about the flow and survival of patients in INHD programmes. This study sought to address this gap in knowledge.
MATERIALS AND METHODS
This is a retrospective study of all patients who participated in the INHD programme in our clinic, from January 1995 until December 2011, which included 51 patients.
The INHD programme performed HD using the Gambro AK 100 HD machine and, subsequently, AK 200. Treatment sessions were administered for more than 5.5 hours thrice weekly, with a dialysate flow rate (Qd) of 600 ml/min and a prescribed blood flow rate (Qb) of 300 ml/min.
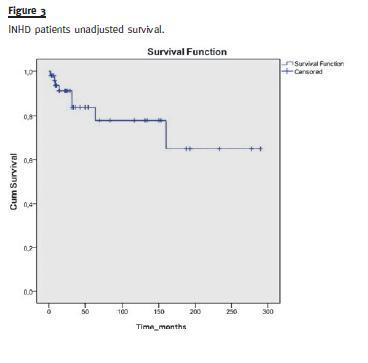
Descriptive data at baseline were presented as means or percentages of the total. We used Kaplan–Meier survival curves for patient survival.
RESULTS
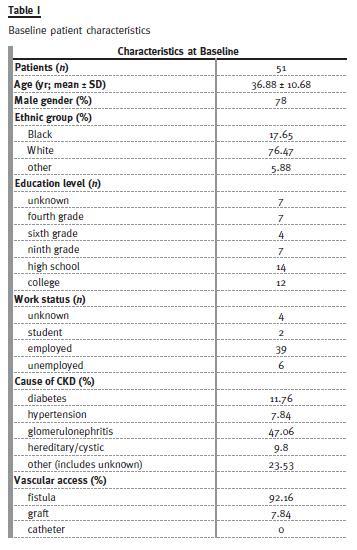
The study cohort included 51 patients who were treated by INHD in our facilities during the study period. The patients characteristics at admission in INHD are shown in Table I.
During the study period, the movement of patients coming in and out of the technique over the years was constant, with an average of incoming and outgoing of 2.1 and 2.5 patients, respectively (Fig. 1).
A mean of 9.6 patients per year remained in the programme. Forty-three of the total 51 patients discontinued the technique: 24 patients underwent kidney transplantation, 11 switched for conventional HD and three changed for peritoneal dialysis (PD). From patients transferred to conventional haemodialysis, one chose home haemodialysis and two needed hospital haemodialysis.
Throughout the period under review five patients died. Figure 2 shows motives for dropping out during the study years. The causes to move from the programme to peritoneal dialysis were: vascular access failure in two patients and the wish for greater autonomy in the other patient. About the two patients who went to hospital haemodialysis, one returned to the hospital unit (where he had previously been on haemodialysis) by non-adaptation to INHD because discomfort and consequent insomnia. The other patient required hospital haemodialysis for clinical deterioration. Desire of a more flexible schedule was the main reason for the patient who chose home haemodialysis. In the case of the eight patients who switch from INHD to conventional HD, the motives were: insomnia in two, indiscipline and disturbance of other patients in one and psychosocial causes in five (patients choice, family convenience, geographic relocation to a region where INHD was not offered, nocturnal work/change for the night shift, retirement).
The global mean time on INHD was 59.5 ± 73 months (median 32 months) during the follow-up period. Table II illustrates the mean time to discontinuing INHD in accordance to patients destination.
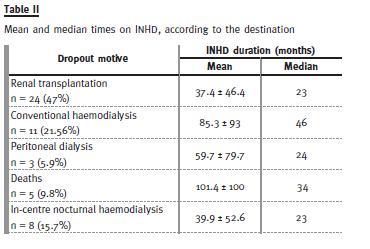
Regarding the survival of patients who remained in INHD, Kaplan–Meier unadjusted survival curve (Fig.3 ) indicates 20 years patient survival rate of 65%. Patients were censored upon changing modality.
DISCUSSION
The characteristics of patients treated by INHD at baseline revealed that they were young (36.9 years), fistula was the preferential vascular access (92.2%) and only 12% were diabetic, aspects quite different when compared with the national registration of patients on HD, with a mean age of dialysis patients of 66.9 years, 70.7% of fistulae and 28.2% of diabetics18.
Patients movement over the study years was constant and there was no significant increase in the INHD programme. The main reason for abandoning the technique was kidney transplantation. The switch of dialysis technique was recorded in 15 patients (11 to CHD and three to PD) after a long period of stay in INHD. Vascular access failure; desire for greater self-sufficiency and flexible schedule; discomfort and insomnia, and psychosocial factors were the most common reasons for patient dropout. Our data are according to the literature, in which trouble sleeping either due to the uncomfortable chair or from insomnia and missing being at home with their relatives are the most frequent motives for abandoning INHD11.
Twenty years patient unadjusted survival rate of 65% obtained in our study was an excellent outcome, especially when compared with the national18 and international19,20 registration of patients on haemodialysis, the former with an annual global mortality of 12%.
Several studies have analysed patient survival on INHD. In Tassin, French patients have been prescribed a regimen of 8-hour sessions, thrice weekly. The results showed improved survival, with an unadjusted survival for all patients at 10 years of 54% on INHD compared to 31% on CHD (21-23). These exceptional outcomes have been the drive for prolongation of dialysis above conventional session durations10. Ok et al.17 performed a prospective multicentre cohort study that matched 247 INHD patients with 247 period-prevalent CHD patients, which found a 72% relative risk reduction for mortality in the INHD cohort.
The U.S. Fresenius Medical Care dialysis network developed the largest study of INHD patients reported to date. An initial study compared 655 prevalent INHD recipients with 15,334 patients on CHD5. One year unadjusted mortality was lower in INHD patients, although after adjustment for case mix and vascular access type this association was no longer obvious.
The significant dilution of the association between INHD and survival in the adjusted analysis underlined the presence of considerable confounding factors, like medical opinion and patient self-selection5. To overcome this limitation, the authors matched 746 patients who converted to INHD to 2,062 CHD recipients using a propensity score-based matching. The results showed that INHD was associated with a significant reduction in all-cause mortality6.
In a simplistic way, extending the mean treatment time differentiates CHD (≥ 12 hours per week) from INHD (≥ >16.5 hours per week). Longer treatment time has been associated with improved outcomes, with a better survival in short daily haemodialysis with length of time of ~15 hours versus approximately 10.5 hours9,24,25. The first direct effect was a marked increase in urea clearance, represented by eKt/V, that overcomes the dialyzers with less surface area, lower blood and dialysate flow rates5,6.
Our study design is observational and with no control population, which is a strong limiting factor that does not allow proving any causation. Moreover, there are several characteristics that may predispose patients to self-select nocturnal therapy, such as being educated, well-informed and working. The majority of our patients (64.7%) had an education level equal to or greater than ninth grade and 76.5% were working active patients. These features may predispose better outcomes per se5,6,10 and, in association with a patients younger age, could also explain the elevated transplantation rate observed in our INHD patients. Nevertheless, it is also possible that extended survival may have contributed for the larger number of renal transplants5,6.
To date, observational studies demonstrated an association between INHD and improved survival.
However these results should be interpreted with caution because patients who are on INHD are a selected (or self-selected) group10.
The published data provide an overview of INHD therapy in comparison with CHD, that established associations but are not conclusive5,6. Additional studies are needed, preferably prospective and randomized, to evaluate this therapeutic option. Such a trial is unlikely to happen, as has already been shown by recruitment sample size failure of the randomized Frequent Hemodialysis Network (FHN) Nocturnal Trial8. It is understandable that when faced with hypotheses that implicate two diametrically opposed dialysis schedules, both with large implications on lifestyle, most patients are reluctant to leave this decision to the trial allocation10.
In summary, patient willingness and logistical issues will still continue to guide patient´s selection for INHD. The characteristics of patients who opt for INHD are not representative of the general CHD population, such that the relative contributions of patient selection versus effect of therapy on outcomes remain to be explained.
References
1. Collins AJ, Foley R, Herzog C, et al. Excerpts from the United States Renal Data System 2007 annual data report. Am J Kidney Dis 2008; 51[Suppl 1]: S1-320. [ Links ]
2. Sarnak MJ, Levey AS, Schoolwerth AC, et al. Kidney disease as a risk factor for development of cardiovascular disease: A statement from the American Heart Association Councils on Kidney in Cardiovascular Disease, High Blood Pressure Research, Clinical Cardiology, and Epidemiology and Prevention. Circulation 2003; 108(17): 2154-2169. [ Links ]
3. Bugeja A, Dacouris N, Thomas A, et al. In-center nocturnal hemodialysis: another option in the management of chronic kidney disease. Clin J Am Soc Nephrol 2009; 4(4):778-783. [ Links ]
4. Eknoyan G, Beck GJ, Cheung AK, et al. with the Hemodialysis (HEMO) Study Group. Effect of dialysis dose andmembrane flux in maintenance hemodialysis. N Engl JMed 2002; 347(25): 2010-2019. [ Links ]
5. Lacson E Jr, Wang W, Lester K, Ofsthun N, Lazarus JM, Hakim RM. Outcomes associated with in-center nocturnal hemodialysis from a large multicenter program. Clin J Am Soc Nephrol 2010; 5(2):220-226. [ Links ]
6. Lacson E Jr, Xu J, Suri RS, et al. Survival with three-times weekly in-center nocturnal versus conventional hemodialysis. J Am Soc Nephrol 2012; 23(4):687-695. [ Links ]
7. Culleton BF, Walsh M, Klarenbach SW, et al. Effect of frequent nocturnal hemodialysis vs conventional hemodialysis on left ventricular mass and quality of life: a randomized controlled trial. JAMA 2007; 298(11):1291-1299. [ Links ]
8. Rocco MV, Lockridge RS Jr, Beck GJ, et al. The effects of frequent nocturnal home hemodialysis: the Frequent Hemodialysis Network Nocturnal Trial. Kidney Int 2011; 80(10):1080-1091. [ Links ]
9. Chertow GM, Levin NW, Beck GJ, with the FHN Trial Group. In-center hemodialysis six times per week versus three times per week.[Erratum appears in N Engl J Med 2011 Jan 6;364(1):93]. N Engl J Med 2010; 363(24):2287-2300. [ Links ]
10. Jakubovic BD, Yan AT, Wald R. In-center nocturnal hemodialysis. Semin Dial 2014; 27(2):179-187. [ Links ]
11. Troidle L,Hotchkiss M, Finkelstein F. A thrice weekly in-center nocturnal hemodialysis program. Adv Chronic Kidney Dis 2007; 14(3): 244–248. [ Links ]
12. Cravedi P, Ruggenenti P, Mingardi G, Sghirlanzoni MC, Remuzzi G. Thrice-weekly incenter nocturnal hemodialysis: An effective strategy to optimize chronic dialysis therapy. Int J Artif Organs 2009; 32(1): 12-19. [ Links ]
13. David S, Kümpers P, Eisenbach GM, Haller H, Kielstein JT. Prospective evaluation of an in-centre conversion from conventional haemodialysis to an intensified nocturnal strategy. Nephrol Dial Transplant 2009; 24(7): 2232-2240. [ Links ]
14. Koch BC, Hagen EC, Nagtegaal JE, Boringa JB, Kerkhof GA, TerWee PM. Effects of nocturnal hemodialysis on melatonin rhythm and sleep-wake behavior: An uncontrolled trial. Am J Kidney Dis 2009; 53(4): 658-664. [ Links ]
15. Powell JR, Oluwaseun O, Woo YM, et al. Ten years experience of in-center thrice weekly long overnight hemodialysis. Clin J Am Soc Nephrol 2009; 4(6): 1097-1101. [ Links ]
16. Troidle L, Finkelstein F, Hotchkiss M, Leypoldt JK. Enhanced solute removal with intermittent, in-center, 8-hour nocturnal hemodialysis. Hemodial Int 2009; 13(4): 487-491. [ Links ]
17. Ok E, Duman S, Asci G, et al. with the Long Dialysis Study Group. Comparison of 4-and 8-h dialysis sessions in thrice-weekly in-centre haemodialysis: A prospective, case-controlled study. Nephrol Dial Transplant 2011; 26(4): 1287-1296. [ Links ]
18. SPN Sociedade Portuguesa de Nefrologia: Relatório do Gabinete de Registo – Tratamentosubstitutivo renal da doença renal crónica estadio V em Portugal, em 2013. www.spnefro.pt/comissoes_gabinetes/Gabinete_registo_2013/default_IRCT.aspLinks
]19. Canadian Institute for Health Information 2013: Annual Report-Treatment of End-Stage Organ Failure in Canada, 2002-2011. Ottawa, CIHI, 2013. [ Links ]
20. U.S. Renal Data System: USRDS 2013 Annual Data Report: Atlas of Chronic Kidney Disease and End-Stage Renal Disease in the United States. National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases. Bethesda, MD, 2013. [ Links ]
21. Charra B, Chazot C, Jean G, et al. Long 3 x 8 hr dialysis: A three-decade summary. J Nephrol 2003; 16[Suppl 7]: S64-S69. [ Links ]
22. Charra B. Is there a magic in long nocturnal dialysis? Contrib Nephrol 2005; 149:100-106. [ Links ]
23. Innes A, Charra B, Burden RP, Morgan AG, Laurent G. The effect of long, slow haemodialysis on patient survival. Nephrol Dial Transplant 1999; 14(4):919-922. [ Links ]
24. Lacson E Jr, Lazarus M. Dialysis time: Does it matter? A reappraisal of existing literature. Curr Opin Nephrol Hypertens 2011; 20(2): 189-194. [ Links ]
25. Kjellstrand C, Buoncristiani U, Ting G, et al. Survival with short daily hemodialysis: Association of time, site, and dose of dialysis. Hemodial Int 2010; 14(4): 464-470. [ Links ]
Drª Isabel Mesquita
Diaverum – Investimentos e Serviços, Lda – Unidade de Entre Campos
Av. das Forças Armadas, 49 – R/c 1600-076 Lisboa, Portugal
E-mail: imesquita@sapo.pt
Conflict of Interest Statement:None declared.
Received for publication: 11/07/2014
Accepted in revised form: 27/10/2014














