Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Portuguese Journal of Nephrology & Hypertension
versão impressa ISSN 0872-0169
Port J Nephrol Hypert vol.28 no.4 Lisboa dez. 2014
CASE REPORT
Lumbar spondylodiscitis with pre- and paraspinal abscess: Major complication of central venous catheter-related infection in a haemodialysis patient
Espondilodiscite lombar com abcesso pré e para vertebral: Uma complicação grave da sépsis de catéter num doente em hemodiálise
Emanuel Ferreira1, Maria Marques1, Helena Pinto1, Ana Belmira1, Carla Domingos2, Armando Carreira1, Mario Campos3
1 Department of Nephrology, Centro Hospitalar e Universitário de Coimbra – Hospital Geral.
2 Department of Neurosurgery, Centro Hospitalar e Universitário de Coimbra – Hospitais da Universidade de Coimbra.
3 Department of Nephrology, Centro Hospitalar e Universitário de Coimbra – Hospitais da Universidade de Coimbra.
ABSTRACT
Vertebral osteomyelitis has been seen with increasing frequency in haemodialysis patients. We describe a case of spondylodiscitis in a patient undergoing haemodialysis with three previous episodes of catheterrelated infections. The poor response to medical treatment and the formation of a large abscess close to the aorta led to the need for surgical intervention. We highlight the need for a multidisciplinary approach to the treatment of this serious complication of the use of central venous catheters in haemodialysis.Key words: Catheter; haemodialysis; infection; magnetic resonance imaging; multidisciplinary approach; spondylodiscitis.
RESUMO
A incidência de osteomielite vertebral tem aumentado no doente em hemodialise. Descrevemos um caso de espondilodiscite lombar numa doente em programa regular de hemodialise com três episódios prévios de sepsis de cateter. A má resposta ao tratamento medico com a formação de abcesso de grandes dimensões próximo da artéria aorta conduziu a necessidade de intervenção cirúrgica.
Destacamos a necessidade de uma abordagem multidisciplinar no tratamento desta importante complicação da utilização de acessos venosos centrais na hemodialise.
Palavras-chave: Abordagem multidisciplinar; cateter; espondilodiscite; hemodialise; infeção; ressonância magnética.
INTRODUCTION
Spondylodiscitis is an infection, usually of bacterial origin, that affects vertebral bodies and adjacent intervertebral discs1. The most common aetiology in patients on haemodialysis (HD) is haematogenous dissemination from a catheter-related infection2.
Other possible sources of infection are by direct inoculation after trauma and the contiguous spread from infected tissues adjacent to the spine3.
Spondylodiscitis has been seen with increasing frequency in HD patients4 and despite the low mortality (< 5%) it may be an important cause of neurological injury, particularly because of the formation of large abscesses5,6. The major clinical manifestation of spondylodiscitis is back or neck pain, depending on its location7. Magnetic resonance imaging (MRI) is the most sensitive radiologic technique, especially in the early stages of the disease8,9.The changes observed in MRI are essentially narrowing of the affected disc, sclerosis and erosion of adjacent vertebral endplates and inflammatory phenomena of the contiguous soft tissues, aspects that have a hypointense signal on T1-weighted images and a hyperintense signal on T2-weighted images10. MRI is also useful to demonstrate the presence of epidural and paraspinal inflammatory tissue and abscesses11.
Treatment is primarily medical and consists of antibiotics, bed rest, stabilization of the spine with orthoses for the trunk, and analgesia5. Surgical treatment is only used infrequently, mainly in cases with poor response to medical treatment5.
CASE REPORT
A 32-year-old woman with a history of unexplained congenital abnormalities that had induced phenotypic changes, cognitive impairment and motor aphasia started haemodialysis, in October 2011, due to chronic kidney disease of unknown aetiology. Her vascular anatomy was unsuitable for the construction of an arteriovenous access.
Between August and December 2011 she had 3 episodes of methicillin-resistant Staphylococcus aureus (MRSA) catheter-related infections. The first episode was before initiation of HD, during a hospitalization for a parathyroidectomy. At that time, a central venous catheter (CVC) was placed in the right subclavian vein owing to lack of peripheral vascular accesses. Vancomycin was administered with a target trough level concentration of 10-20 mcg/mL and the subclavian catheter was replaced by a femoral catheter.
Attending to difficulty in reaching the desired vancomycin levels, with high toxic concentrations, a switch to linezolid was performed on the twentieth day of vancomycin. Linezolid was administered, at a dosage of 600 mg every 12 hours, during 7 days.
A transoesophageal echocardiogram was performed in the setting of MRSA bacteraemia to rule out infective endocarditis; it did not present signs of vegetations or valvular abnormalities. The second and third episodes of MRSA catheter-related infections arose when the patient had already started high-flux HD.
Both were treated with vancomycin, administered during the last 30-60 minutes of each dialysis session, with doses ranging 500-1000 mg to attain the aforementioned therapeutic range. In the second episode, vancomycin was administered during 4 weeks and the infected femoral catheter was replaced by a right internal jugular vein catheter. In the third episode, vancomycin was administered during 6 weeks and the infected cuffed tunneled jugular catheter was exchanged over a guidewire.
Lower back pain started in January 2012 and worsened progressively, without complaints relating to other mechanisms or systems. She was apyretic and without leukocytosis, but had C-reactive protein (CRP) of 17.6 mg/dL (reference range lower than 1 mg/dL).
Plain radiography of the lumbar spine reinforced the clinical suspicion of spondylodiscitis, later confirmed by MRI of the lumbosacral spine – spondylodiscitis process centred at L3-L4, possibly having evolved over some time (non-acute). The patient was assessed jointly with the Departments of Infectious Diseases, Neurosurgery and Physical Medicine and Rehabilitation: blood cultures were harvested, vancomycin and ceftazidime initiated empirically, opiate analgesia was administered, and the lumbar spine was stabilized with bed rest and dorso-lumbar support.
Vancomycin was administered with the same schedule treatment previously mentioned and 1000 mg of ceftazidime were administered after each HD session. The tunnelled CVC of the right internal jugular vein was exchanged over a guidewire. A transoesophageal echocardiogram was repeated and disclosed no signs of endocarditis. Since blood cultures were negative, vancomycin and ceftazidime were administered during eleven weeks. After completing the course of antibiotics, the patient was asymptomatic, showed no leukocytosis, had negative CRP and presented a slight reduction of the paraspinal component of the infectious lumbar process.
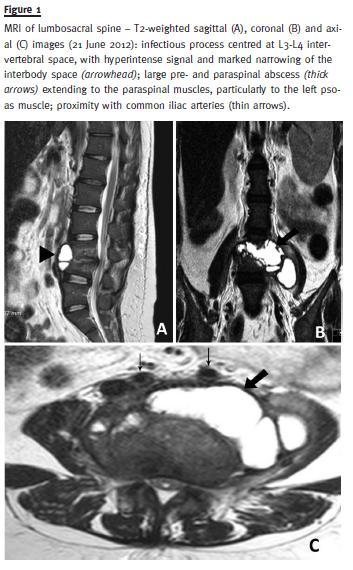
Lower back pain, fever, vomiting, prostration and anorexia started again on 28 May 2012. Analysis showed leukocytosis of 10900/uL and CRP of 34.2 mg/dL. MRI of lumbosacral spine was performed, where significant worsening of the infectious process centred at the L3-L4 intervertebral space was observed, which was mainly noted by enlargement of the pre- and paraspinal abscess that extended to the paraspinal muscles, particularly to the leftpsoas muscle. Blood cultures were taken and vancomycin and ceftazidime were reassumed with the same schedule treatment previously mentioned.
Blood cultures were again negative. After 3 weeks of antibiotic therapy and despite clinical and analytical improvement, the control MRI revealed enlargement of the abscess (Fig. 1). The patient was reassessed by neurosurgery and general surgery which, given the size of the abscess and its proximity to the aorta, decided to drain it surgically on the 28th June, and harvest the purulent material for microbiology. The procedure consisted of puncture and aspiration of the pre- and paraspinal abscess using a fluoroscopically guided retroperitoneal approach followed by debridement of inflamed intramuscular and perisomatic tissues. In addition, an intracavity microcatheter was left for the post-operative irrigation of the abscess cavity and the rest of the surgical site with antibiotics. The chosen route of approach did not produce spinal instability and it was, therefore, not necessary to carry out any spine stabilization procedure.
The culture of the purulent exudate identified MRSA sensitive to vancomycin and linezolid, and initiation of linezolid was chosen due to progression of the disease despite long treatment with vancomycin. Linezolid was administered at a dosage of 600mg every 12 hours, but was suspended after 3 weeks of treatment due to thrombocytopenia, with a count of 28000/uL. Vancomycin was reassumed.
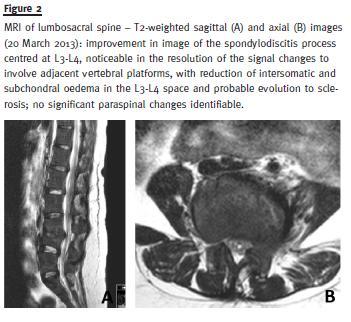
The follow-up MRI after surgery showed significant improvement in the size of the abscess, even though the infectious process was still not completely resolved on the 12th July 2012. The patient was discharged after 72 days of hospitalization (3rd August 2012) clinically asymptomatic, showing no leukocytosis and having negative CRP. Antibiotic therapy with vancomycin was maintained until the 1st February 2013, and an MRI performed on the 20th March that year showed resolution of signal abnormalities on T2-weighted images (Fig. 2).
Currently, about 16 months since the last hospital admission, she remains asymptomatic and shows no evidence of recurrence of the spondylodiscitis.
DISCUSSION
The incidence of spondylodiscitis has increased in recent years due to population ageing and the increasing use of immunosuppressive therapy and intravascular devices1,2,8. This case documents the typical clinical presentation of lumbar spondylodiscitis in a patient on haemodialysis - fever and back pain in a patient using CVC, with a history of infection related to it. Despite early diagnosis and prompt treatment with regard to onset symptoms, the first MRI of the lumbosacral spine showed an infectious process that had been developing for some time, an aspect that emphasizes the importance of a high index of clinical suspicion in these patients, because the initial symptoms of spondylodiscitis can be insidious and non-specific4.
The empirical antibiotic treatment of choice was vancomycin and ceftazidime, targeting the commonest aetiological agents: Staphylococcus aureus and gram-negative bacilli7,9. Because the microorganisms were not isolated in the first blood culture, the first treatment cycle was maintained for 11 weeks, as recommended in the most severe cases of illness5.
Surgical treatment of spondylodiscitis is indicated in cases of: a) poor response to medical treatment; b) need to harvest material for culture in a sterile medium; c) epidural abscess with spinal cord compression; d) abscess which volume impedes the action of antibiotics; e) impossible image-guided drainage due to anatomical location; f) biomechanical spinal instability or deformity caused by the collapse of the vertebral bodies affected12-14. In our case, the poor response to medical treatment with recurrence of symptoms and radiological worsening, the need to harvest material in sterile medium for culture, and proximity to the aorta were the reasons that led to surgical treatment.
Regarding the maintenance of the second course of antibiotic therapy for 28 weeks, it should be noted that even though an average duration of 6 to 12 weeks is advocated, there have been no randomized controlled studies to clarify the duration of antibiotic therapy, particularly in severe cases of disease3,5.
The usefulness of MRI for monitoring therapeutic efficacy has also been questioned, and so the duration of the antibiotic therapy should bear in mind the clinical evolution and analytical parameters of the infection11,15. In this case, progression of disease, despite initial treatment with 11 weeks of empirical antibiotic therapy, the severity of the disease and the need to keep the CVC influenced the extended duration of the antibiotic therapy.
Our case highlights the importance of a multidisciplinary approach in the treatment of spondylodiscitis.
Interaction between the different medical and surgical specialties is important and, for our patient, this was reinforced by the seriousness of the disease and the abscess site close to central neurological and vascular structures.
References
1. Ramirez-Huaranga MA, Sanchez de la Nieta-Garcia MD, Anaya-Fernandez S, et al. Spondylodiscitis, nephrology departments experience. Nefrologia 2013;33(2):250-255. [ Links ]
2. Cervan AM, Colmenero Jde D, Del Arco A, Villanueva F, Guerado E. Spondylodiscitis in patients under haemodyalisis. Int Orthop 2012; 36(2):421-426. [ Links ]
3. Cebrian Parra JL, Saez-Arenillas Martin A, Urda Martinez-Aedo AL, Soler Ivanez I, Agreda E, Lopez-Duran Stern L. Management of infectious discitis. Outcome in one hundred and eight patients in a university hospital. Int Orthop. 2012; 36(2):239-244. [ Links ]
4. Garcia-Garcia P, Rivero A, del Castillo N, et al. Infectious spondylodiscitis in hemodialysis. Semin Dial 2010;23(6):619-626. [ Links ]
5. Sexton JD, McDonald M. Vertebral osteomyelitis and discitis. Uptodate. 2013. Available at: site www.uptodate.com/contents/vertebral-osteomyelitis-and-discitis?source=search_result&search=vertebralosteomyelitis&selectedTitle=1~57. Acess at 20/12/2013. [Updated 2013 May 21]
6. Heyde CE, Boehm H, El Saghir H, Tschoke SK, Kayser R. Surgical treatment of spondylodiscitis in the cervical spine: a minimum 2-year follow-up. Eur Spine J 2006; 15(9):1380-1387. [ Links ]
7. Faria R, Borges C, Carrondo H, Banza MJ. Espondilodiscite – que etiologia? Acta Med Port 2011;24(6):1059-1064. [ Links ]
8. Valero R, Castaneda O, de Francisco AL, Pinera C, Rodrigo E, Arias M. Clinical suspicion of vertebral osteomielitis: back pain in patients with hemodyalisis by catheter related infection. Nefrologia 2004;24(6):583-588. [ Links ]
9. Tanaka N, Kasahara H, Yoshie T, Hora K, Kiyosawa K. Back pain out of the blue in a haemodialysis patient. Nephrol Dial Transplant 1999;14(7):1792-1794. [ Links ]
10. Gasbarrini AL, Bertoldi E, Mazzetti M, et al. Clinical features, diagnostic and therapeutic approaches to haematogenous vertebral osteomyelitis. Eur Rev Med Pharmacol Sci 2005;9(1):53-66. [ Links ]
11. Miller JC, Phil D. Vertebral Osteomyelitis. Radiology Rounds. 2006 November/December; 411. [ Links ]
12. Korovessis P, Repantis T, Hadjipavlou AG. Hematogenous pyogenic spinal infection: current perceptions. Orthopedics. 2012;35(10):885-892. [ Links ]
13. Vaccaro AR, Basil MH, Madigan L. Spinal infections, pyogenic osteomyelitis and epidural abcess. In: Principles and Practice of Spine Surgery. Mosby: 2002; 165-174. [ Links ]
14. Greenberg MS. Vertebral osteomyelitis. In: Handbook of Neurosurgery. Thieme, New York, USA: 2010; 380-383. [ Links ]
15. Kowalski TJ, Berbari EF, Huddleston PM, Steckelberg JM, Osmon DR. Do follow-up imaging examinations provide useful prognostic information in patients with spine infection? Clin Infect Dis 2006;43(2):172-179. [ Links ]
Dr. Emanuel Filipe Eufrasio Ferreira
Department of Nephrology Centro Hospitalar e Universitario de Coimbra – Hospital Geral.
Quinta dos Vales, S. Martinho do Bispo,
3041-853 Coimbra, Portugal
E-mail: emanuelfeferreira@gmail.com
Conflicts of interest statement: None declared.
Received for publication: 07/06/2014
Accepted in revised form: 06/08/2014














