Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Portuguese Journal of Nephrology & Hypertension
versão impressa ISSN 0872-0169
Port J Nephrol Hypert vol.28 no.4 Lisboa dez. 2014
ORIGINAL ARTICLE
Very elderly patients on haemodialysis: Evolution and its relation with comorbidities
Doentes muito idosos em hemodiálise: Evolução e sua relação com as comorbilidades
Claudia Bento, Monica Fructuoso, Rui Costa, Rui Castro, Teresa Morgado
Department of Nephrology, Centro Hospitalar de Tras‑os‑Montes e Alto Douro. Vila Real, Portugal.
ABSTRACT
Introduction: The population ageing has conditioned a progressive increase of very old patients on haemodialysis. These patients present multiple comorbidities that worsen the prognosis in dialysis and have an impact on their quality of life. Material and Methods: A retrospective observational study was performed, analysing all patients over 80 years of age that started regular haemodialysis between January 2004 and December 2011. The comorbidities were stratified using the Charlson score and correlated with mortality. Survival analysis was performed with Kaplan-Meier curves. Results: Fifty-nine patients were included, 35 females and 24 males, with a mean age of 84 ± 3 years. At the start of dialysis, the estimated glomerular filtration rate calculated using the modification of diet in renal disease (MDRD) formula was 10.8 ± 2.5 mL/min /1.73 m2. The initial Charlson score was 8 ± 3 and became higher at the end of follow-up (11.5 ± 2.9; p < 0.01). A Charlson score ≥ 8 was associated with more hospitalization days (878 vs. 360; p < 0.005). The survival rate was 56 % at 12 months and 31% at 24 months. The mortality rate at the end of follow-up (20.4 ± 15.7 months) was 55.9%, with a mortality rate of 27.3% at 3 months. The patients with early death presented a higher Charlson score (13.0 ± 1.7 vs. 6.4 ± 1.2; p < 0.01) at the beginning of dialysis. Conclusion: The benefits of dialysis in survival and quality of life in very elderly patients have been questioned. In our series, more than 1/4 of the patients died in the first 3 months of dialysis, corresponding to higher comorbidity scores. The use of comorbidity scores like the Charlsons may assist in the assessment of the short-term prognosis, but the individualized decision should prevail in all cases.
Key-Words: Charlson score; chronic renal disease; comorbidities; elderly patients; haemodialysis; survival.
RESUMO
Introdução: O envelhecimento populacional tem condicionado um aumento progressivo de doentes muito idosos em hemodialise. Estes doentes apresentam multiplas comorbilidades que agravam o prognostico em dialise e que tem impacto na sua qualidade de vida. Material e Métodos: Estudo observacional retrospetivo de doentes integrados em programa regular de hemodialise com idade igual ou superior a 80 anos entre janeiro/2004 e dezembro/2011. As comorbilidades foram estratificadas utilizando o score de Charlson e relacionadas com a mortalidade. Na analise de sobrevida foram utilizadas as curvas de Kaplan-Meier. Resultados: Foram avaliados 59 doentes, 35 do sexo feminino e 24 do sexo masculino, com 84 ± 3 anos. A data de inclusao em programa regular de hemodialise a taxa de filtracao glomerular calculada pela formula MDRD era de 10,8 ± 2,5 ml/minuto. O score inicial de Charlson era de 8 ± 3 e aumentou no final do follow-up para 11,5 2,9; p < 0,01. Um score de Charlson igual ou superior a 8 associou-se a maior numero de dias de internamento (878 vs. 360; p < 0,005) e a uma sobrevida de 56% aos 12 meses e 31% aos 24 meses. A mortalidade ate ao final do follow-up (20,4 15,7 meses) foi de 55,9 %, com uma mortalidade precoce (< 3 meses) de 27,3 %. Este ultimo grupo apresentava um score de Charlson mais elevado no inicio de dialise (13,0 ± 1,7 vs. 6,4 1,2; p < 0,01). Conclusão: Os beneficios da dialise na sobrevida e qualidade de vida dos doentes muito idosos tem sido questionados . Na nossa serie, mais de ¼ dos doentes faleceram nos primeiros 3 meses, correspondendo a scores de comorbilidade mais elevados. Indices de comorbilidade como o de Charlson podem auxiliar na determinacao do prognostico vital a curto prazo, mas a decisao individualizada deve sempre prevalecer.
Palavras-Chave: Comorbilidades; doença renal cronica; hemodialise; pacientes idosos; score de Charlson; sobrevida.
INTRODUCTION
The ageing of the population has conditioned a progressive increase of elderly patients on dialysis.
In Portugal, 61.6% of the incident dialysis patients, in 2012, were over 65 years and the mean age of the prevalent patients was 66.8 years1. According to the Portuguese Ministry of Health, in 2010 36% of the prevalent dialysis patients were aged over 74 years2. Elderly patients present multiple comorbidities that worsen the prognosis in dialysis and have an impact on their quality of life. Age per se is a strong predictor of mortality3,4 and the mortality rate is considerably higher for elderly patients on dialysis than for elderly patients who are not4-7.
Therefore, it is often a challenge to decide whether starting dialysis is the best option for those patients.
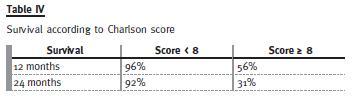
Assessment of the overall comorbidities may be helpful to identify the patients whose condition will probably evolve poorly. The Charlson score, an index of comorbidity that includes age, has proven to correlate well with survival and is divided into four groups according to punctuation: low (< 3 points), moderate (4-5 points), high (6-7 points) and very high (≥ 8 points)8. The survival probability will be lower with higher scores (with a score ≥ 8, the survival probability at 12 months is 64% and 35% at 24 months)8.
Our study intends to analyse the evolution of a group of elderly patients (≥ 80 years) with chronic kidney disease after starting haemodialysis (HD), according to the Charlson score.
MATERIALS AND METHODS
A retrospective, observational study was performed, analysing all patients aged 80 years or more at the start time of regular haemodialysis, between January 2004 and December 2011, in our Nephrology Department. The information was obtained through consultation of the hospital and dialysis centers records. The follow-up period was 20.4 ± 15,7 months [1.3 – 70.6]. The comorbidities were stratified using the Charlson score at HD beginning and at the end of follow-up and were related with mortality. Statistical analysis was performed using the t-test for quantitative variables, Chi squared for qualitative variables and Kaplan-Meier curves for survival analysis.
RESULTS
We evaluated 59 patients, 35 female and 24 male, with a mean age of 84 ± 3 years [80-93] at dialysis start. The prevalence of diabetes was 37.7% and the main aetiology of chronic kidney disease (CKD) was diabetic nephropathy (37.7%). The vast majority of patients had been previously followed by a nephrologist (91.5%).
At the time of HD beginning, the glomerular filtration rate calculated using the Modification of Diet in Renal Disease (MDRD) formula was 10.8 ± 2.5 mL/min/1.73 m2. The criteria for starting haemodialysis were uremic symptoms in 47 cases (79.7%) and hypervolemia or refractory hiperkaliemia in the remaining (20.3%). Analysing the vascular access type at the first dialysis session, 32 patients (54%) started haemodialysis with a central venous catheter (CVC) and an arteriovenous fistula (AVF) in the remainder. In the group of patients that started haemodialysis with a CVC, the vasculature was not appropriate for the creation of an autologous vascular access in 28%, 18% were waiting arteriovenous fistula maturation and 8% were not previously followed by a nephrologist. The vast majority of our patients (71%) had some dependence on the daily activities routine (29% were totally dependent for daily living activities and 42% had partial dependence).
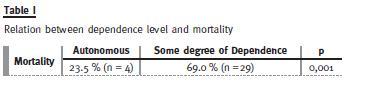
The results of our study demonstrate a high prevalence of dependence among these elderly patients.
We also observed a high rate of mortality in this population, with a positive correlation between mortality and level of dependence (those with a higher grade of dependence had higher mortality during follow-up) – Table I, which is in accordance with other published studies.
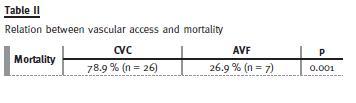
The use of a catheter as a vascular access was higher (mentioned above) and like other studies it was observed a relationship between central venous catheter and a higher risk of mortality – Table II.
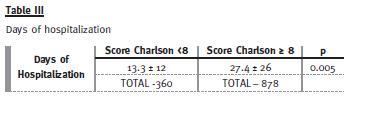
The Charlson score at HD start was 8 ± 3, with 54% of the patients having a score equal or greater than 8. At the end of follow-up, the score was significantly higher (11.5 ± 2.9 [6-17]; p < 0.01).
The global mortality rate in our study was 55.9% until the follow-up end. The mortality rate in the first 3 months after HD start was 27.3% and at 12 months was 45.4%. The patients that survived less than 3 months on dialysis presented a higher Charlson score (13.0 ± 1.7 vs. 6.4 ± 1.2; p < 0.01). Patients with a very high score (≥ 8) had a survival rate of 56 % at 12 months and 31 % at 24 months- Fig. 2/Table IV.

DISCUSSION
The benefits of dialysis in terms of survival and quality of life in very old patients with chronic kidney disease have been questioned, mainly because of the high morbidity and mortality of these patients9-11.
This morbidity may be increased by additional burdens imposed by dialysis like time spent on dialysis, loss of autonomy, neurological impairment, complications of the vascular access (mainly infection), pain and hospitalization days. Although patients may live longer with dialysis, the extension of lifetime may be associated with a poor quality of life and degradation of its basal state.
Some studies have demonstrated that the survival of elderly patients on dialysis may actually be considerably reduced, compared to that of the population at the same age4-7. One study showed that the survival advantage of dialysis in patients over 75 years with multiple comorbidities is unlikely to be more than four months12 and more recently Murtagh et al. reported that dialysis might not offer a survival benefit in patients over 75 years with multiple comorbidities, especially in those with ischemic heart disease10,13,14. On the other hand, Munshi et al. reported a mortality rate at one year of 46.5% in patients over 75 years, being hospitalized 20% of these days15.
Based on this reality, some authors consider that dialysis may not be of benefit for all elderly patients and the conservative approach may be the best option in some cases14.
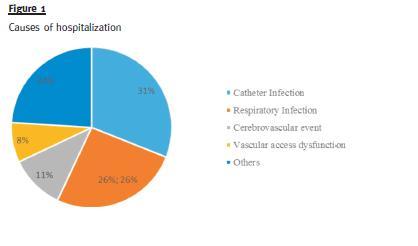
In our study, we found a significant raise in the comorbidities score between the beginning of dialysis and the end of follow-up. It is possible that the dialysis procedure itself or its complications, like vascular access-related infections (the main cause of hospitalization) may have contributed. This may reflect a functional decline and a disability increase, higher levels of dependence and quality of life deterioration.
It is well known that the use of an AVF provides better quality of life, improved blood flows, results in fewer hospital admissions for access failure or related infections, and is associated with better survival and reduced health care costs than central venous catheters16. As demonstrated in our study, CVC is a clinically and statistically significant variable associated with mortality and it is a potentially modifiable independent predictor of mortality.
About 1/4 of our patients died in the first 3 months and in 45% the life expectancy was inferior to 12 months, as described in other studies8,17. Like in other reports8,9,18,19 we demonstrated that survival and hospitalizations correlated with the Charlson score.
The individualized decision should always prevail but the use of a comorbidity index score may assist in the assessment of prognosis at the short term and help identify the patients that would benefit from dialysis. A more complete score that includes: Charlson score, level of dependence for daily activities in association with modifiable independent predictors of early mortality on dialysis (presence of CVC, lack of attendance at a nephrology) should be thought.
References
1. Macario F. Relatorio Gabinete de Registo da SPN. Tratamento Substitutivo Renal da Doenca Renal Cronica Estadio V em Portugal. 2013. [ Links ]
2. Norma da Direcao – Geral da Saude. Tratamento Conservador Medico da Insuficiencia Renal Cronica Estadio 5. Norma No 017/2011 de 28/09/2011. 28/09/2011. [ Links ]
3. Goodkin DA Young EW, Kurokawa K, Prutz KG, Levin NW. Mortality among hemodialysis patients in Europe, Japan, and the United States: case-mix effects. Am J Kidney Dis 2004;44(5 Suppl 2):16-21. [ Links ]
4. Kurella M, Covinsky KE, Collins AJ, Chertow GM. Octogenarians and nonagenarians starting dialysis in the United States. Ann Intern Med 2007;146(3):177-183. [ Links ]
5. Wright S. Chapter 20: Hemodialysis in Elderly Patients. Geriatric Nephrology Curriculum. American Society of Nephrology 2009. [ Links ]
6. Go AS, Chertow GM, Fan D, McCulloch CE, Hsu CY. Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N Engl J Med 2004;351(13):1296-1305. [ Links ]
7. OHare AM, Choi AI, Bertenthal D, Bacchetti P, Garg AX, Kaufman JS, et al. Age affects outcomes in chronic kidney disease. J Am Soc Nephrol 2007;18(10):2758-2765. [ Links ]
8. Beddhu S, Bruns FJ, Saul M, Seddon P, Zeidel ML. A simple comorbidity scale predicts clinical outcomes and costs in dialysis patients. Am J Med 2000;108(8):609-613. [ Links ]
9. Smith C, Da Silva-Gane M, Chandna S, Warwicker P, Greenwood R, Farrington K. Choosing not to dialyse: evaluation of planned non-dialytic management in a cohort of patients with end-stage renal failure. Nephron Clin Pract 2003;95(2):c40-46. [ Links ]
10. Murtagh FE, Marsh JE, Donohoe P, Ekbal NJ, Sheerin NS, Harris FE. Dialysis or not? A comparative survival study of patients over 75 years with chronic kidney disease stage
5. Nephrol Dial Transplant 2007;22(7):1955-1962.
11. OConnor NR, Corcoran AM. End-stage renal disease: symptom management and advance care planning. Am Fam Physician 2012;85(7):705-710. [ Links ]
12. Isles C, Robertson S, Almond A, Donaldson K, Clark D. The challenges of renal replacement therapy and renal palliative care in the elderly. J R Coll Physicians Edinb 2011;41(3):238-243. [ Links ]
13. Davies SJ, Phillips L, Naish PF, Russell GI. Quantifying comorbidity in peritoneal dialysis patients and its relationship to other predictors of survival. Nephrol Dial Transplant 2002;17(6):1085-1092. [ Links ]
14. Dasgupta I, Rayner HC. Dialysis versus conservative management of elderly patients with advanced chronic kidney disease. Nat Clin Pract Nephrol 2007;3(9):480-1. [ Links ]
15. Munshi SK, Vijayakumar N, Taub NA, Bhullar H, Lo TC, Warwick G. Outcome of renal replacement therapy in the very elderly. Nephrol Dial Transplant 2001;16(1):128-133. [ Links ]
16. McQuillan R, Trpeski L, Fenton S, Lok CE. Modifiable risk factors for early mortality on hemodialysis. Int J Nephrol 2012;2012:435736. doi:10.1155/2012/435736 [ Links ]
17. Chae JW, Song CS, Kim H, Lee KB, Seo BS, Kim DI. Prediction of mortality in patients undergoing maintenance hemodialysis by Charlson Comorbidity Index using ICD-10 database. Nephron Clin Pract 2011;117(4):c379-384. [ Links ]
18. Di Iorio B, Cillo N, Cirillo M, De Santo NG. Charlson Comorbidity Index is a predictor of outcomes in incident hemodialysis patients and correlates with phase angle and hospitalization. Int J Artif Organs 2004;27(4):330-336. [ Links ]
19. Frenkel WJ, Jongerius EJ, Mandjes-van Uitert MJ, van Munster BC, de Rooij SE. Validation of the Charlson Comorbidity Index in acutely hospitalized elderly adults: a prospective cohort study. J Am Geriatr Soc 2014;62(2):342-346 [ Links ]
Dra Claudia Bento
Department of Nephrology, Centro Hospitalar de Tras-os-Montes e Alto Douro.
Avenida da Noruega, 5000-508 Lordelo,Vila Real Portugal
E-mail: claudiaqbento@gmail.com
Conflict of interest statement: None declared
Received for publication: 11/06/2014
Accepted in revised form: 7/11/2014














