Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Portuguese Journal of Nephrology & Hypertension
versão impressa ISSN 0872-0169
Port J Nephrol Hypert vol.28 no.1 Lisboa mar. 2014
ORIGINAL ARTICLE
Chronic kidney disease in patients with acute myocardial infarction without ST segment elevation: therapeutic nihilism?
Doença renal crónica em doentes com enfarte agudo do miocárdio sem elevação do segmento ST: niilismo terapêutico?
M. Teresa Santos, Rute M. Ferreira, Cristina Rosario, Liliana Carneiro, J. Maximino Costa, Ana Veloso, Cristina Gavina
Nephrology Department, Hospital Pedro Hispano, Unidade Local de Saúde de Matosinhos, EPE. Matosinhos, Portugal.
ABSTRACT
Background: Chronic kidney disease is an independent risk factor for mortality after acute coronary syndrome. Our aim was to characterize the in-hospital management and outcomes of patients with chronic kidney disease in the setting of non-ST-segment elevation myocardial infarction. Methods: This is a single centre, prospective and observational study, including 230 consecutive patients admitted with the diagnosis of non-ST-segment elevation myocardial infarction. Glomerular filtration rate was estimated using the Modification of Diet in Renal Disease Study formula and in-hospital therapies and outcomes were recorded. Results: Overall, 25.7% of patients had moderate to severe chronic kidney disease. Patients with chronic kidney disease were less likely to undergo coronary angiography (27% vs. 81%, p < 0.001) and receive less evidence-based therapies, including aspirin (86.4% vs. 98.8%, p < 0.001), clopidogrel (74.6% vs. 90.6%, p = 0.002), angiotensin-converting enzyme inhibitor and/or angiotensin II receptor blocker (54.2% vs. 90.6%, p < 0.001) or anticoagulant therapy (83.1% vs. 95.9%, p = 0.001). In addition, the in-hospital mortality was higher for patients with chronic kidney disease (15.3% vs. 2.9%; p = 0.002). Conclusion: Non-ST-segment elevation myocardial infarction patients with chronic kidney disease have higher in-hospital mortality. The underuse of evidence-based therapies and interventions can help to explain these results.
Key-words: Acute myocardial infarction; chronic kidney disease.
RESUMO
Introdução: A doença renal crónica é um fator de risco independente para mortalidade após síndrome coronário agudo. O objetivo deste estudo foi caracterizar o tratamento, complicações e mortalidade intrahospitalar dos doentes com doença renal crónica internados no contexto de enfarte agudo do miocárdio sem elevação do segmento ST. Métodos: Estudo unicêntrico, observacional e prospetivo que incluiu 230 doentes internados com o diagnóstico de enfarte agudo do miocárdio sem elevação do segmento ST. A taxa de filtração glomerular foi estimada pela fórmula Modification of Diet in Renal Disease Study e foi avaliado o tratamento, complicações e mortalidade intra-hospitalar. Resultados : Do total de doentes admitidos no estudo, 25.7% apresentavam doença renal crónica moderada a grave. Os doentes com doença renal crónica foram menos submetidos a cateterismo cardíaco (27% vs. 81%, p< 0.001) e foram menos medicados com terapêutica baseada na evidência, nomeadamente aspirina (86.4% vs. 98.8%, p < 0.001), clopidogrel (74.6% vs. 90.6%, p = 0.002), inibidor da enzima de conversão da angiotensina e/ou antagonista do receptor da angiotensina II (54.2% vs. 90.6%, p < 0.001) e anticoagulantes (83.1% vs. 95.9%, p = 0.001). Os doentes com doença renal crónica apresentaram mortalidade intra-hospitalar superior (15.3% vs. 2.9%; p = 0.002). Conclusão: Neste estudo os doentes com enfarte agudo do miocárdio sem elevação do segmento ST e doença renal crónica apresentam mortalidade intra-hospitalar superior. A subutilização de terapêutica baseada na evidência poderá ajudar a explicar estes resultados.
Palavras-chave: Doença renal crónica; enfarte agudo do miocárdio.
INTRODUCTION
Chronic kidney disease (CKD) and acute coronary syndrome (ACS) are highly prevalent and widespread diseases1,2. Approximately 25% to 40% of all patients with non-ST-segment elevation myocardial infarction (NSTEMI) have at least moderately reduced renal function3,4.
Chronic kidney disease is a recognized independent risk factor for early and late mortality after ACS5-7. Higher prevalence of other comorbidities, like hypertension and diabetes mellitus, diagnostic challenges because of the atypical presentation, and biological factors that promote and accelerate cardiovascular disease, are common among patients with CKD and contribute to the poor outcome of ACS in this specific population8,9. Moreover, several registries report underuse of evidence-based therapies in this population10.
The aim of the present study is to characterize the in-hospital management and outcomes of patients with CKD in the setting of NSTEMI.
METHODS
This is a single centre, prospective and observational study, including consecutive patients admitted to the emergency department of Hospital Pedro Hispano EPE, with the diagnosis of NSTEMI, between the 1st January and the 31st December 2010. Only type 1 myocardial infarctions (MI) were included. The information was collected prospectively by physicians and more than 100 variables were studied. They included baseline characteristics, ECG changes, biochemical markers, in-hospital course and coronary angiography.
Glomerular filtration rate (eGFR) was estimated using the Modification of Diet in Renal Disease (MDRD) Study formula11, which includes creatinine, age, gender and race. Creatinine measurements for the 3-12 months before admission were used for eGFR calculation.
The diagnosis of CKD was considered if the eGFR was < 60 mL/min/1.73m2 (K/DOQI stages 3 to 5)12.
Previous data of stroke, MI, congestive heart failure (HF), chronic pulmonary disease, diabetes mellitus, hypertension (HT), dyslipidaemia and chronic medications were obtained from medical records or reported by the patients or their family. Patients were treated according to the recommendations of the 2007 ACS guidelines13, but the final decision of therapeutic options was the responsibility of the attending physician.
For coronary angiography we considered all patients who underwent coronary angiography during the hospital stay, regardless if they were revascularized or not.
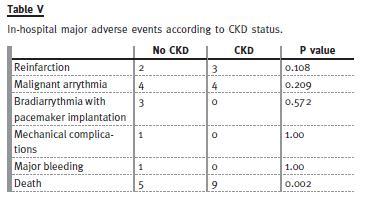
The main adverse events reported were reinfarction, malignant arrythmia, bradiarrythmia with pacemaker implantation, mechanical complications (including acute mitral regurgitation, interventricular septal rupture, cardiac tamponade and cardiac rupture), major bleeding (including intracranial, retroperitoneal or any haemorrhage requiring transfusion) and death.
Statistical analysis
Categorical variables were expressed as percentages and continuous variables as mean ± standard deviation or median and interquartile range, according to their distribution. Continuous variables were compared between groups using unpaired t-test (for normally distributed variables) or the Mann-Whitney U-test (for non-normally distributed variables).
Spearman´s rank correlation was used for the assessment of continuous variables.
Multivariable logistic regression model was used to study the association between coronary angiography and baseline characteristics and risk scores.
Variables with clinically and statistically univariate relationships with coronary angiography were included in the multivariate model.
All reported probability values are two-tailed, and p < 0.05 was considered statistically significant. Analyses were performed with the IBM®SPSS® Statistics software package (version 20.0) (SPSS Inc, Chicago, IL, USA).
The authors had access to the data and take full responsibility for the results. All authors have read and agreed to the manuscript as written.
RESULTS
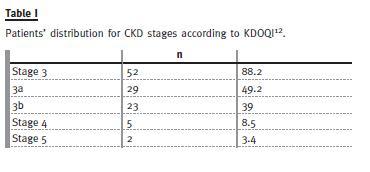
In total, 230 NSTEMI patients were included in the present analysis. Fifty nine patients (25.7%) had stages 3 to 5 CKD. The majority (88%) had stage 3 CKD (Table I). Baseline characteristics of patients with and without CKD are presented in Table II.
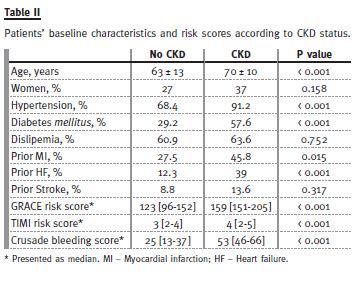
Patients with CKD were older, more often diabetic, and more frequently had previous MI or heart failure.
The CKD patients also had higher pre-treatment risk scores of death/MI (TIMI risk score; GRACE risk score) and bleeding (CRUSADE bleeding score) (Table II).
In-hospital treatment
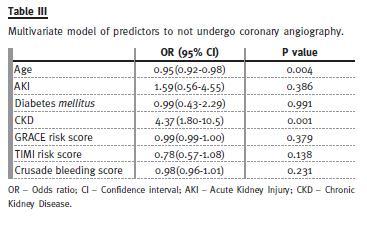
Patients with CKD were less likely to undergo coronary angiography (27% with CKD vs. 81% without CKD, p < 0.001).
After adjustment for age, presence of diabetes mellitus, acute kidney injury and risk scores, CKD was an independent predictor for not submitting to coronary angiography (p = 0.001) (Table III).
Patients with CKD were also less likely to receive in-hospital evidence-based medical therapies, such as aspirin (p < 0.001), clopidogrel (p = 0.002), angiotensin-converting enzyme inhibitor and/or angiotensin II receptor blocker (p < 0.001) or anticoagulant therapy (p = 0.001) (Table IV).
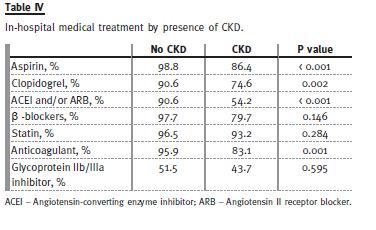
For patients who underwent coronary angiography, the rates of the use of glycoprotein IIb/IIIa inhibitors were similar among those with and without CKD
In-hospital outcomes
There were no differences between groups concerning the major adverse events pre-defined in this study (Table V).
In the 154 patients who underwent coronary angiography, there were six cases (3.9%) of iodinated contrast induced nephropathy (CIN), five of which in patients with CKD (p < 0.001). In none of these five patients dialysis was needed.
Fourteen patients died during hospitalization due to cardiovascular events. In-hospital mortality was higher for patients with CKD [nine (15.3%) vs. 5 (2.9%); p = 0.002].
DISCUSSION
Globally, 25.7% of patients had moderate to severe CKD in this study, which is consistent with the findings in the more contemporary data using MDRD equation14.
Patients with CKD had more comorbidities than patients without CKD, and higher risk scores of reinfarction, death and bleeding. Despite their higher risk, CKD patients were less likely to receive evidencebased therapies and the presence of CKD was an independent predictor for not undergoing coronary angiography. This seems to be a paradox in the management of CKD patients with NSTEMI.
The lesser use of coronary angiography in CKD patients may be justified by the fear of worsening kidney function, but several authors have demonstrated that the benefit overcomes the risk4,15-17.
Furthermore, the most recently published guidelines by the American College of Cardiology/American Heart Association for management of NSTEMI state that an early invasive strategy is a reasonable strategy in patients with mild and moderate CKD18.
We found the same rates of CIN described in the literature19 and these patients did not experience major adverse events, suggesting that CIN is not a valid reason to avoid iodinated contrast media investigations in this group of patients.
Some previous studies have demonstrated the underuse of evidence-based medical therapies in CKD patients4,14 and have suggested that it could contribute to the higher mortality observed in this population.
On the other hand, a recent publication1 concludes that treatment disparities related to CKD are most evident at top-performing hospitals, and the reasons for those findings need to be explored.
Our CKD patients also had underuse of all evidence-based therapies, but this was more evident with antithrombotic agents. We found a significantly decreased use of aspirin, clopidogrel and anticoagulant in CKD patients. Given that CKD patients also have higher risk scores for bleeding, one possible explanation for these differences is physicians perception of bleeding risk in these patients, making them withhold antithrombotics prescription. The increased risk of bleeding in CKD patients may be related to intrinsic platelet dysfunction20 and excessive dosing of medications21.
Similarly, we found an underuse of ACEI and/or ARB. That could be explained by the higher rate of acute kidney injury at hospital admission in CKD patients (39% vs. 6.4%) and, once more, by the concern that these medications can deteriorate kidney function, even though benefits of ACEI and/or ARB are well documented in patients with reduced left ventricular ejection fraction18.
No difference was seen between patients with or without CKD, concerning the rates of major in-hospital adverse events, except death. Indeed we did not register any episodes of major bleeding in CKD patients. The small number of patients and the small number of adverse events observed contribute for that fact.
The highest rates of in-hospital mortality observed in patients with CKD, when compared with those observed in patients without CKD, are concordant with previous reports4,16,22. Given our small sample, we can only speculate that the underuse of evidence based medications and procedures could be responsible for the higher in-hospital mortality in CKD patients.
Strengths and Limitations
The major strength of the present study includes the use of a Portuguese prospective cohort that reflects the reality of NSTEMI management in our country.
Furthermore, because of the organizational structure of this hospital unit, we had easy access to the previous creatinine determinations, so it was possible to ascertain more accurately the patients actual renal function.
However, certain limitations are notable. This being a single centre analysis with a relatively small number of patients, it precludes definite conclusions about outcomes.
Finally, as we used MDRD Study formula that underestimates GFR in individuals with measured GFR ≥ 60 ml/min/1,73m223, and as we did not have information about other markers of kidney damage except for serum creatinine, we could not identify patients with CKD stages 1 and 2. Especially, we did not have information on albuminuria and proteinuria known as risk markers of cardiovascular events24.
CONCLUSIONS
Chronic kidney disease patients presenting with NSTEMI have more comorbidities and higher risk scores of death and bleeding.
Data from this study suggests that patients with CKD receive fewer evidence-based therapies and have substantially higher in-hospital mortality rates. However, further research is warranted to define the relevance of undertreatment for the higher mortality seen in patients with CKD after NSTEMI.
References
1. Patel UD, Ou FS, Ohman EM, et al. Hospital performance and differences by kidney function in the use of recommended therapies after non-ST-elevation acute corornary syndromes. Am J Kidney Dis 2009;53(3):426-437. [ Links ]
2. Shroff GR, Frederick PD, Herzog CA. Renal failure and acute myocardial infartion: clinical characteristics in patients with advanced chronic kidney disease, dialysis, and non-chronic kidney disease. A collaborative project of the United States Renal Data System/National Institutes of Health and the National Registry of Myocardial Infarction. Am Heart J 2012;163(3):399-406. [ Links ]
3. Santopinto JJ, Fox KA, Goldberg RJ, et al. on behalf of the GRACE Investigators. Creatinineclearance and adverse hospital outcomes in patients with acute coronary syndromes: findings from the global registry of acute coronary events (GRACE). Heart 2003;89(9):1003-1008. [ Links ]
4. Fox CS, Muntner P, Chen AY, et al. Use of evidence-based therapies in short-term outcomes of st-segment elevation myocardial infarction and non-st-segment elevation myocardial infarction in patients with chronic kidney disease: a report from the National Cardiovascular Data Acute Coronary Treatment and Intervention Outcomes Network registry. Circulation 2010;121(3):357-365. [ Links ]
5. Shlipak MG, Heidenreich PA, Noguchi H, Chertow GM, Browner WS, McClellan MB. Association of renal insufficiency with treatment and outcomes after myocardial infarction in elderly patients. Ann Intern Med 2002;137(7):555-562. [ Links ]
6. Reddan DN, Szczech L, Bhapkar MV, et al. Renal function, concomitant medication use and outcomes following acute coronary syndromes. Nephrol Dial Transplant 2005;20(10):2105-2112. [ Links ]
7. Al Suwaidi J, Reddan DN, Willias K, et al. Prognostic implications of abnormalities in renal function in patients with acute coronary syndromes. Circulation 2002;106(8):974-980. [ Links ]
8. McCullough PA, Maynard RC. Treatment disparities in acute coronary syndromes, heart failure, and kidney disease. Contrib Nephrol 2011;171:68-73. [ Links ]
9. Rodrigues FB, Bruetto RG, Torres US, Otaviano AP, Zanetta DM, Burdmann EA. Effect of kidney disease on acute coronary syndrome. Clin J Am Soc Nephrol 2010;5(8):1530-1536. [ Links ]
10. Komajda M, Follath F, Swedberg K, et al. and the Study Group on Diagnosis of the Working Group on Heart Failure of the European Society of Cardiology. The EuroHeart Failure Survey programme – a survey on the quality of care among patients with heart failure in Europe, Part 2: treatment. Eur Heart J 2003;24(5):464-474. [ Links ]
11. Levey AS, Bosh JP, Lewis JB, Green T, Rogers N, Roth D. Modification of Diet in Renal Disease Study Group. A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Ann Intern Med 1999;130(6):461-470. [ Links ]
12. K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Am J Kidney Dis 2002;39(2 Suppl 1):S1-S266. [ Links ]
13. Anderson JL, Adams CD, Antman EM, et al. ACC/AHA 2007 Guidelines for the management of patients with unstable angina/non-ST-elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation 2007;116(7):e-148-e304. [ Links ]
14. Hanna EB, Chen AY, Roe MT, Wiviott SD, Fox CS, Saucedo JF. Characteristics and inhospital outcomes of patients with non-ST-segment elevation myocardial infarction and chronic kidney disease undergoing percutaneous coronary intervention. JACC Cardiovasc Interv 2011;4(9):1002-1008. [ Links ]
15. Szummer K, Lundman P, Jacobson SH, et al. for SWEDEHEART. Influence of renal function on the effects of early revascularization in non-ST-elevation myocardial infarction. Circulation 2009;120(10):851-858. [ Links ]
16. Charytan DM, Wallentin L, Lagerqvist B, et al. Early angiography in patients with chronic kidney disease: a collaborative systematic review. Clin J Am Soc Nephrol 2009;4(6):1032-1043. [ Links ]
17. Yu J, Ooi SY, Sergie Z, Baber U. Is there attenuation of benefit of invasive therapy in patients with chronic kidney disease? Results from randomized trials and registry data. Curr Cardiol Rep 2012;14(4):521-527. [ Links ]
18. 2012 ACCF/AHA Focused update of the guideline for the management of patients with unstable angina/non-ST-elevation myocardial infarction (updating the 2007 guideline and replacing the 2011 focused update): a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation 2012;126(7):875-910. [ Links ]
19. Solomon RJ, Natarajan MK, Doucet S, et al. and the Investigators of the CARE Study. Cardiac Angiography in Renally Impaired Patients (CARE) Study: a randomized doubleblind trial of contrast-induced nephropathy in patients with chronic kidney disease. Circulation 2007;115(25):3189-3196. [ Links ]
20. Moscucci M, Fox KA, Cannon CP, et al. Predictors of major bleeding in acute coronary syndromes: the Global Registry of Acute Coronary Events (GRACE). Eur Heart J 2003;24(20):1815-1823. [ Links ]
21. Alexander KP, Chen AY, Roe MT, et al. and the CRUSADE Investigators. Excess dosing of antiplatelet and antithrombin agents in the treatment of non-ST-segment elevation acute coronary syndromes. JAMA 2005;294(24):3108-3116. [ Links ]
22. Anavekar NS, McMurray JJ, Velásquez EJ, et al. Relation between renal dysfunction and cardiovascular outcomes after myocardial infarction. N Eng J Med 2004;351(13):1285-1295. [ Links ]
23. Stevens LA, Coresh J, Greene T, Levey AS. Assessing kidney function – measured and estimated glomerular filtration rate. N Engl J Med 2006;354(23):2473-2483. [ Links ]
24. Hui X, Matsushita K, Sang Y, Ballew SH, Fülöp T, Coresh J. CKD and cardiovascular disease in the Atherosclerosis Risk in Communities (ARIC) Study: interactions with age, sex, and race. Am J Kidney Dis 2013;62(4):691-702. [ Links ]
Drª Maria Teresa Santos
Nephrology Department
Hospital Pedro Hispano,
Unidade Local de Saúde de Matosinhos, EPE
Rua Dr. Eduardo Torres, 4454-509, Matosinhos
Portugal
E-mail: teresamsantos@gmail.com
Conflict of interest statement: None declared.
Received for publication: 03/10/2013
Accepted in revised form: 04/02/2014














