Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Arquivos de Medicina
versão On-line ISSN 2183-2447
Arq Med vol.24 no.6 Porto dez. 2010
ARTIGO DE REVISÃO
Epidemiology of Cervical Cancer
Epidemiologia do cancro do colo do útero
Carla Alves 1, Luís Alves 1,2,3, Nuno Lunet1,2
1Department of Hygiene and Epidemiology, Porto University Medical School, Porto, Portugal
2Institute of Public Health – Porto University (ISPUP), Porto, Portugal
3St. André de Canidelo Health Family Unit, Vila Nova de Gaia, Portugal
ABSTRACT
Cervical cancer is the fifth most common cancer in European women. The recognition of a viral agent such as Human Papillomavirus (HPV) as a necessary cause in the development of cervical cancer implies that this disease may be prevented by effective prophylactic or therapeutic interventions against this infection. HPV vaccines conferring protection against infection with oncogenic HPV types 16 and 18, which cause the majority of the cervical cancer cases, are currently marketed, but. Continued cervical cancer screening is necessary regardless of vaccination. Organised screening programs have the highest potential to reduce cervical cancer mortality, by achieving higher levels of coverage of all population groups and higher proportions of women screened at regular intervals, with better cost-effectiveness and overall quality. Opportunistic screening, on the other hand, has a more limited impact and is more difficult to monitor and to evaluate due to its decentralized nature and lack of systematic reporting. However, opportunistic screening is still predominant in most European countries. In Portugal, cervical cancer screening has been predominantly opportunistic, except for regional organised programs in the Central Region of Portugal, in the region of Alentejo and an organised screening program is also being implemented in the North region of Portugal.
Key-words: uterine cervical neoplasm; epidemiology; screening
RESUMO
O cancro do colo do útero é o quinto cancro mais frequente em mulheres europeias. A identificação do vírus do Papiloma humano como causa necessária para o desenvolvimento do cancro do colo do útero implica que esta doença possa ser prevenida pela implementação de medidas profilácticas ou terapêuticas efectivas dirigidas a esta infecção. Existem actualmente vacinas que conferem protecção contra a infecção pelos tipos de vírus do Papiloma humano oncogénicos responsáveis pela maioria dos cancros do colo do útero. Contudo, o rastreio do cancro do colo do útero continua a ser essencial para a prevenção e controlo deste cancro, e os programas de rastreio organizados têm um maior potencial para reduzir a mortalidade por cancro do colo do útero, proporcionando níveis de cobertura mais elevados em todos os grupos da população, em intervalos regulares, com uma melhor relação custo-eficácia e qualidade. O impacto do rastreio oportunista é mais limitado, sendo a qualidade deste tipo de actividades de rastreio mais difícil de avaliar devido à sua natureza descentralizada e à falta de recolha sistemática de toda a informação necessária para a avaliação. Contudo, os rastreios oportunistas representam ainda a única prática de actividades de rastreio na maioria dos países europeus. Em Portugal, o rastreio do cancro do colo do útero tem sido predominantemente oportunista, excepto na região Centro e Alentejo, que dispõe de programas regionais de rastreio organizado e está a ser implementado o rastreio organizado também na região norte de Portugal.
Palavras-chave: cancro do colo do útero; epidemiologia; rastreio
Burden of cervical cancer worldwide
Cervical cancer is the second most common cancer and the third most important cause of cancer mortality worldwide, among women1. It accounts for approximately 12% of all cancers in women. Every year, 493,000 new cases occur and approximately 274,000 women die from cancer of the cervix1.
Since cervical cancer affects predominantly young women, it is an important cause of years of life lost (YLL). It has been estimated that cervical cancer was responsible for 2.7 million YLL in 2000 and it is the primary cause of YLL from cancer in the developing world, representing around 2% of the YLL from all causes of disease. Among women aged between 25 and 64 years, cervical cancer contributes with 2.4 million YLL in developing areas and 0.3 million in the developed countries21 .
Incidence of cervical cancer
Cervical cancer is more frequent in less-developed countries. Southern Africa, South America and south Central Asia have the highest age-standardised incidence rates, over 25 per 100,000 women1. The highest incidence rates are reported in Haiti (64 per 100,000 women), Lesotho (46 per 100,000 women) and Bolivia (42 per 100,000 women). The highest absolute number of cases estimated in 132,000 new cases/year is observed in India corresponding to more than one-fourth of the worldwide total1.
The age-standardised incidence rate (World reference population) in more developed countries is 10.3 per 100,000 women, approximately half the observed in developing regions1. In Europe, Finland reported the lowest incidence rate (6.2 per 100,000 women) followed by Malta (7.1 per 100,000 women) and Ireland (8.4 per 100,000 women)1.
Trends in cervical cancer incidence have been clearly affected by the practice of screening15. In Nordic countries, for example, age-standardised incidence rates of cervical cancer have shown a downward trend since the 1960s decade, demonstrating a decrease from 21.2 per 100,000 in 1966 to 7.6 per 100,000 in 200622. On the other hand, some sub-Saharan African regions have registered an increased incidence in recent years23,24.
Survival of cervical cancer patients
In developing countries, less than 50% of women affected by cervical cancer survive longer than 5 years, while in developed countries the 5-year survivalis about 66%25 .
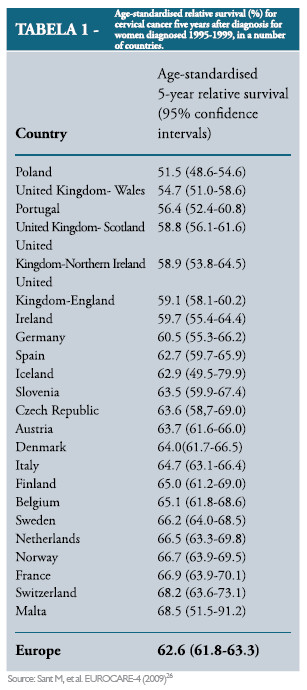
The latest data from cervical cancer survival for women diagnosed between 1995 and 1999 is available from the EUROCARE-4 project (Table 1). the European average 5-year age-standardised relative survival for cervical cancer diagnosed in 1995–1999 and followed up to december 2003 was 62.6%26, but there is a large heterogeneity across countries, with 5-year age-standardised relative survival ranging from 51.5% in Poland to 68.5% in malta (Table 1).
In the first half of the 20th century, major improvements in survival from cancer of the cervix were observed, due in part to improving stage at diagnosis, and better results of treatment, particularly as a result of advances in radiotherapy27,28. However, the most recent estimates are not substantially different from those observed in the previous periods covered by the EUROCARE projects29, as shown in Figure 1
.
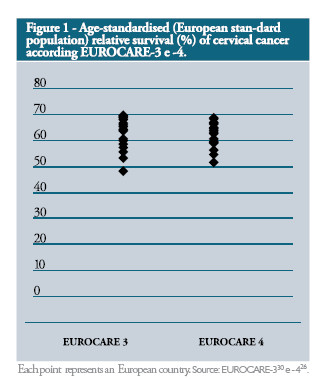
The European average 5-year age-standardised relative survival for cervical cancer diagnosed in the period 1990–1994 and followed up to 1999 was 62.1%31. In sweden, Netherlands and Norway 5-year age-standardised relative survival was significantly higher than the European mean, while Poland, Estonia and Portugal had the poorest survival for cervical cancer. In Portugal (estimates from the southern region) had particularly low survival for cervical cancer (55.6%)32 . The relative survival of patients with cervical cancer increased by 3%, from the cases diagnosed in the period 1978-1989 [EUROCARE-233] to the period 1994-1999 [EUROCARE-426]. The main determinant of cervical cancer prognosis remained the stage at diagnosis and this modest increase in survival rate has been interpreted as being due mainly to earlier diagnosis32 .
Cervical cancer mortality
Approximately 80% of all cervical cancer cases and deaths occur in less-developed countries, where cervical cancer accounts for 15% of female cancers and about 40% of cervical cancer deaths in developing countries occur in south Central Asia, a heavily populated region1. The highest mortality rates are reported in lesotho (38 per 100,000 women), Haiti (35 per 100,000 women) and tanzania (33 per 100,000 women)1. The age-standardised mortality rate (World reference population) is 11.2 per 100,000 women in less developed countries, almost three times higher than in developed regions1 (Table 2
). The lowest mortality rates in Europe are reported in southern (5.6 per 100,000 women) and in Northern Europe (5.8 per 100,000 women) (Table 2).
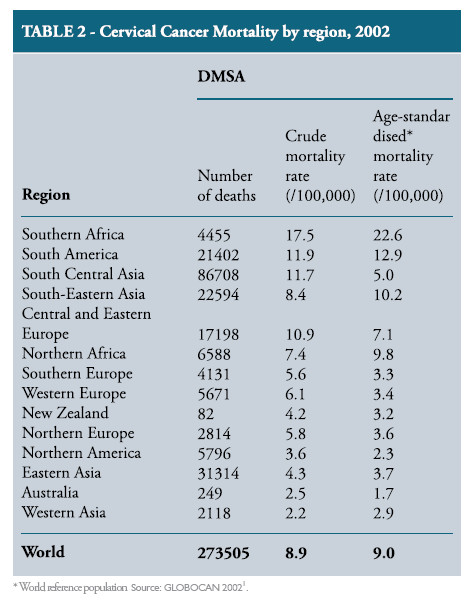
A declining trend in cervical cancer mortality is clearly observed, in developed countries where mainly cervical cytology programme exist. In European Union countries, from1993 to 2001,a gradual decrease was observed in age-standardised mortality rate, from 3.4 per 100,000 women in 1993 to 2.8 per 100,000 (World population reference)1. However, in less developed countries, this trend follows the opposite direction. In south Africa, for example, age-standardised mortality rate increased from 9.9 per 100,000 in 1993 to 13.3 per 100,000 in 20051.
Burden of cervical cancer in Portugal
Portugal presents the highest rates of cervical cancer in Western Europe, with an incidence rate of 14.8 per 100,000 women and a mortality rate of 4.9 per 100,000 women in 2001, being the fifth most common cancer among women34. Approximately 780 new cases occur and 260 women die every year34 .
Relative 5-year survival in the south of Portugal was 60%, the fourth lowest among other European countries represented in the recent publication of the Registo Oncológico Regional da Região Sul (ROR-Sul)35 .
Incidence of cervical cancer in Portugal
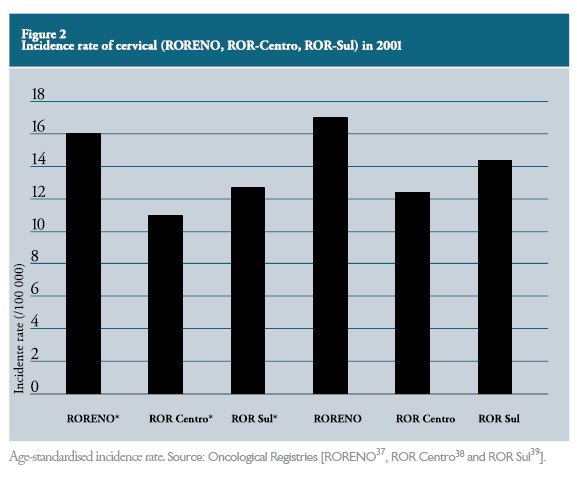
Cervical cancer incidence rates are available from three population-based Regional Cancer Registries, namely the Registo Oncológico Regional da Região Norte (RORENO), covering the Northern region (3.5 million inhabitants), ROR-Centro, covering the Central region of the country (1.7 million inhabitants), and ROR-sul, which covers the south and the Madeira islands (4.2 million inhabitants)36 .
The incidence rates for cervical cancer in the three Regional Cancer Registries (RORENO, ROR-Centro e ROR-sul) are presented in Figure 2
. The lowest age-standardised cervical cancer incidence rate was reported in the Central region.
Regarding the trends in cervical cancer incidence, there are substantial qualitative and quantitative differences in the information provided by the three Regional Cancer Registries, as depicted in Figure 3
, which impose limitations to the interpretation of the available data.

The data made available by the ROR-sul does not allow a sound interpretation of the variation of incidence over the years and in the northern region no descending trend is observed in the most recent years.
For the region covered by ROR-Centro, data is available for both invasive and in situ cervical cancer, with similar trends since 2000.
When evaluating the incidence rates for invasive and in situ cervical cancers together, peaks are observed in the mid-nineties and in 2000, which are in accordance with the variation in incidence of all cancers registered by ROR-Centro40 (Table 3
).
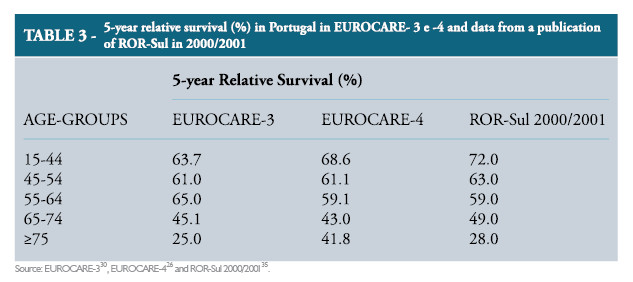
Survival of cervical cancer patients in Portugal
Population-based data on cancer survival in Portugal is available from the ROR-sul for the incident cases diagnosed in the years 1990-199430, 1995-199926 , and 2000-2001 in the southern region (approximately 40% of the Portuguese population) (Table 3
)35,40. In Portugal a slight increase in age-standardised relative survival from 55.6% in the years 1990-1994 to 60.0% in 2000/2001 was verified (Table 3).The 5-year relative survival in the southern region was 60%, placing Portugal in the forth lowest position among other European countries35 .
The most recent data from ROR-sul also shows regional differences in 5-years relative survival ranging from 55% in the region of Algarve to 72% in Alentejo.
Cervical cancer mortality in Portugal
In 1996-1998 cervical cancer was responsible for 4.2% of malignants deaths in Portuguese women75. The crude mortality rate in Portugal, according to estimates from GLOBOCAN 2002, was 7.3 per 100,000 women, preceded by Slovenia with 7.8 per 100,000 and by Denmark with 8.6 per 100,0001.
Between 1988-1990 and 1996-1998, the age-standardised (World reference population) mortality rate decreased from 6.7 per 100,000 women to 5.8 per 100,000 and in the 55-74 age group, corresponding to a -2.7% variation per annum. This variation has been interpreted unlikely to have been due to the effect of cervical screening because mortality in the 35–54 group has not decreased. Probably better access and quality treatment over the previous 10 years explained part of this decrease75 .
No overall decline in the age-standardised mortality rate of cervical cancer was observed in Portugal since 1980 (Figure 4).
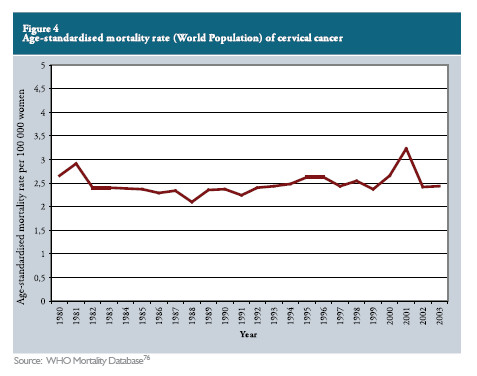
In women aged between 25 and 79 years mortality from cervical cancer has remained stable between 1980 and 2005 (annual percent change=0.0%, 95%CI: -0.5 to 0.5). The variation was 2.0%/year (95% CI: 0.8 to 3.2) in the age-group 25-44 years, 0.7%/year (95% CI: -0.3 to 1.7) in women aged between 45 and 54 years, 0.4%/year (95% CI:1.4-0.6) in the age-group 54-64 years and -1.6%/ year (95%CI: -2.4 to -0.7%) in the age-group 6579 years77 .
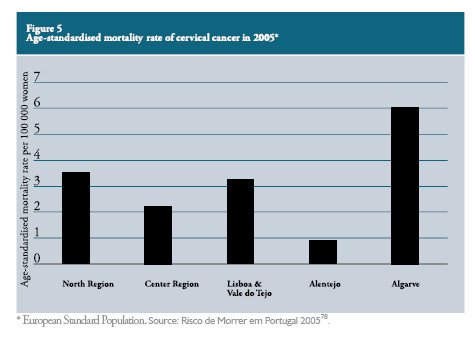
In 2005, the lowest age-standardised mortality rates were observed in Alentejo and in the Center region of Portugal with 0.9 per 100,000 women and 2.2 per 100,000 women respectively, areas where regional organised programme are implemented (Figure 5
). On the other hand, in Algarve, a region without organised cervical cancer screening it was verified the highest age-standardised mortality rates in Portugal (6.0 per 100,000 women)78 .
Risk factors for cervical cancer
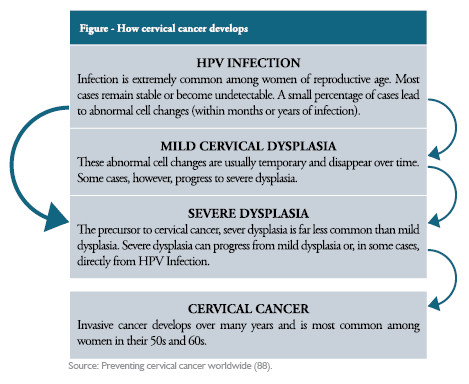
Epidemiological studies conducted over the past 4 decades have consistently shown that cervical cancer risk is strongly influenced by sexual behaviour: multiple sexual partners, early age at first sexual intercourse, and sexual habits of male partners79,80. Evidence on the causal role of some HPV infections, a sexually transmitted, in the development of cervical cancer are provided by epidemiological studies, supported by molecular technology7. thus, early age at first intercourse and multiple sex partners are associated with a higher risk of HPV infection indirectly increasing the risk of cervical cancer81. Case-control studies, case series, and prevalence surveys have unequivocally shown that HPV-DNA can be detected in 95-100% of cases, compared with a prevalence of 5-20% in cervical specimens from a women identified as suitable epidemiological controls15 and infection with a high-risk HPV type is now considered a necessary cause, though not sufficient, for cervical cancer. Factors such as the number of full-term pregnancies, tobacco smoking and long-term use of hormonal contraceptives may contribute to the progression from cervical HPV infection to cancer82 .
HPV and cervical cancer
Human papillomavirus (HPV) is the cause of genital human papillomavirus infection, a sexually transmitted disease (STD). HPV infection is the most prevalent sexually transmitted infection in the world, especially among young sexually active individuals. It is estimated that approximately 75% to 80% of the sexually active individuals will become infected in their lifetime83 . Studies among initially virginal women strongly confirm the sexually transmitted nature of HPV infection84. Sexual contact with an infected partner is necessary for transmission, but HPV infections are easily transmitted and it seems that intromissive intercourse is not strictly necessary85. HPV dNA has been detected 13% of women who have sex with women. HPV-associated squamous intraepithelial lesions occurred in women who have sex with women, who had never had sex with men85 . HPV infects basal epithelial cells, where it exists for a variable period in a non-expressed or latent state. At some point, the virus begins to replicate, by dividing epithelial cells, most commonly causing low-grade cervical lesions as well as vaginal, vulvar, penile lesions, genital warts86 . Certain types of HPV can cause abnormal cell changes, called dysplasia. Some cases regress or do not progress especially in women under age 35. If this abnormality persists over time and become severe, the cells tend to develop into cancer. Progression from HPV infection to cancer can take up 5 to 30 years; severe dysplasia can progress to cervical cancer over several years5, 6, 87 (Figure 6
).
Virtually all cases of cervical cancer result from a history of persistent infection with HPV pertaining to a high risk subset of this family of viruses89. The contribution of HPV DNA in high-grade squamous intraepithelial lesions (morphological precursors of invasive cervical cancer), as indicated by cross-sectional studies of the natural history of cervical cancer, is estimated to be over 85%90 .
The strength of the association between infection of the cervix with high-risk types of HPV and invasive cervical cancer is almost unprecedented in cancer epidemiology, with odds ratios (OR) over 50 in most studies91,92.
HPV types are stratified into low-, intermediate-, and high-risk categories based on the strength of the association between infection and the occurrence of high-grade and invasive lesions. More than 100 different HPV types have been described, of which approximately 40 types infect the anogenital tract93 . Among this, about 15 types (HPV-16,-18,-31,-33,35,-39,-45,-51,-52,-56,-58,-59,-68,-73, and -82) are now considered to be of high-oncogenic-risk (HRHPV)92. The predominant low-risk types (HPV 6 and 11)94, 95 cause 90% of genital warts (condyloma acuminata). The most prevalent high-risk types (HPV 16 and 18) cause 70% of cervical cancer and cervical intra-epithelial neoplasia (CIN) and a reconsidered the most oncogenic viruses worldwide93 .
Human papillomavirus type 16 is the most common high-risk type, accounting for more than half (56%) of all cervical cancers91 .
It has now been established, based on both molecular and epidemiologic evidence, that HPV can cause high-grade cervical intraepithelial neoplasia and invasive cervical cancer, being a major discovery in human cancer aetiology96. the evidence is consistent worldwide and implies both the squamous Cell Carcinomas (SCC), the adenocarcinomas and the vast majority (i.e. > 95%) of the immediate precursors, namely High grade squamous Intraepithelial lesions (HSLL)/Cervical Intraepithelial Neoplasia 3 (CIN3)/Carcinoma insitu97 .
It is not yet clear how aging affects HPV prevalence in different populations worldwide. Many studies have reported that the highest prevalence occurs in women under 25, with a progressive linear decline after the age of 25, remaining below 5% after the age of 55 98,99.
Other risk factors for cervical cancer
Several factors may influence whether a woman with precancerous lesions develops cervical cancer or not, such as the use of tobacco81, 100, an impaired immune system, hormonal factors, the use of hormonal contraceptives, early age at first birth, high parity8, 81, 101 and Clamydia trachomatis infections102 . The effects of smoking have been studied in many case-control studies which found moderate and statistically significant associations with cervical cancer, after adjustment for the strong effects of HPV103, 104. Nicotine have been detected in the cervical mucus of smokers, strengthening the hypothesis of a synergistic action between cigarette smoking and the development of HSIL and cervical cancer105 . A linear dose-response relationship between cervical cancer and the use of hormonal contraceptives is showed in a recent meta-analysis.the relative risk of cervical cancer increased with increasing duration of oral contraceptive, being with the use of oral contraceptive approximately less than 5 years, 5-9 years and 10 years or longer, respectively,1.1(95%CI1.1-1.2),1.6(1.41.7) and 2.2 (1.9-2.4)101 .
High parity is a consistent risk factor for cervical cancer and has been found consistently in most case-control studies to be associated with both cervical cancer and carcinoma in situ. In the International Agency for Research on Cancer (IARC) multicentric study, the OR for cervical cancer in women with seven or more full-term pregnancies was fourfold higher than in nulliparous women, and the risk increased linearly with increasing number of full-term pregnancies106 . The evidence on the role of lifestyles related to diet or physical activity in cervical carcinogenesis is too limited to conclude that any aspect of food, nutrition, and physical activity directly modifies the risk of this cancer107 .
HPV vaccination
Ninety-five percent of all cervical cancers are at tributable to HPV infection in the general populatio108 . The diseases produced by the oncogenic genotypes of HPV have the potential to be eradicated109.thus, primary prevention of cervical cancer can be achieved through prevention and control of genital infection with oncogenic HPV types110 .
Recently, prophylactic vaccines have become commercially available, that are based on the recombinant expression and self-assembly of the major capsid protein, l1, into virus-like particles (VLPs) that resemble the outer capsid of the whole virus111 .
A quadrivalent HPV 16/18/6/11 vaccine was the first to be approved for use in adolescent and young women ages 9 to 26 years for the prevention of cervical cancer (HPV 16 and 18) and genital warts (HPV 6 and 11), as well as vulvar and vaginal precancerous lesions. It is administered as a 0,5 ml intramuscular injection in a three-dose immunization protocol (2 and 6 months after the first dose)112 .
A bivalent HPV 16/18 virus-like particles (VLP) vaccine is also available as a 0,5 ml intramuscular injection in a three-dose immunization protocol at 1 and 6 months after the first dose112 .
Bivalent vaccines as well as quadrivalent vaccines have been demonstrated to be safe, immunogenic and effective against type-specific HPV infection10,113.
In women who have no evidence of exposure or infection with the HPV genotypes that are present in the vaccine, both vaccines show very high efficacy, with over 90% reduction in persistent infection and greater than 98% reduction in high-grade cervical lesions102, 114, 115. Human Papillomavirus vaccines are efficacious in all age groups within the 15-26 years range116 .
The progressive development of primary prevention strategies should coexist with secondary prevention of cervical cancer, by means of redesigned screening programs, because vaccination is for pre-exposure prophylaxis; most women will continue to rely on screening117 .
Screening and vaccination, adopted in synergy, have the potential to significantly reduce cervical cancer globally. However, in an era of strained health care budgets, even resource-rich countries will have difficulty to support the extra costs of vaccination without some level of re-structuring of their screening programmes118 .
Vaccination plus screening should, in theory, prevent almost 100% of cervical cancers, but this could only apply in countries with organized screening programmes, allowing, ensuring an equal coverage fall population groups116 .
The gradual extension of vaccination will progressively reduce the costs of the diagnosis and treatment of lesions detected by screening of vaccinated cohorts109 . At the beginning of 2008, HPV vaccination had not been implemented in all countries of the European Union. CzechRepublic, France, Germany, Greece and Italy had implemented HPV vaccine in the national immunization programme since 2007 and the target populationis, respectively, 12-15,14-25,12-17,12-15 years. In 2008, Luxembourg, Portugal, Spain and United Kingdom introduced the vaccine in the national immunization programme for girls with 12-18, 13, 12 and 12-13years respectively2.
Cervical cancer screening
Cervical cancer is both preventable and curable and is the malignant neoplasic disease for which public health prevention initiatives have had the greatest success119 .
Precancerous changes in cervical tissue can persist for years. However, if they are identified and successfully treated early, the lesions will not develop into cervical cancer. Thus, screening women for precancerous changes and treating tissue abnormalities seems to protect women from developing cervical cancer, ultimately decreasing its mortality119 .
Screening methods
Cervical cancer screening started with the introduction of Papanicolaou test into developed countries and it is largely responsible to the remarkable success achieved in cervical cancer prevention. The cervical cytology is a laboratory test Developed in the 1940s to detect abnormal cell changes and screening with this method is still considered an integral part of womens preventive health care in many settings120 .
In most routine settings, cervical cytology has a wide range in sensivity in detecting cervical neoplasia. In reviews of several studies the sensivity to detect high-grade CIN lesions ranged from 47-62% and the specificity from 91-96%121-123. In studies in developing countries the sensivity of cervical cytology ranged from 31 to 78 percent and the specific from 91-96%124.This low sensivity has been attributed to a combination of poor sample collection (5%-10% of all slides), incorrect slide preparation and laboratory interpretation errors121, 125. False-negative results occur even in optimized screening programs and cannot be entirely eliminated126 .
However, conventional cervical cytology test screening has the potential to reduce the risk of developing cervical cancer by 60% to 90% within three years127 , and reduction in cervical cancer incidence and mortality in the US and other developed countries has been accomplished despite the relatively low sensivity of conventional cytology123 .
In England, invasive cervical cancer incidence and mortality rates decreased by approximately 50% from 1988 to 1997, after the introduction of an organised screening program. A similar trend was observed in Norway immediately after the introduction of a national cancer cytology program (cervical cytology test) in 1995127. The extent of this decrease is not generally verified in countries where screening is population-based15 .
Liquid-based cytology (LBC) was developed primarily to improve the quality of cervical samples128, 129.This process aims to potentially reduce two important deficiencies observed in conventional cytology: the relatively small and potentially non-representative sample of cells and the effect of other material, including mucous, blood, and other non-cervical cells, on the readability of theslide124. As LBC is more expensive than conventional cytology and requires additional instrumentation, it may not be feasible to implement LBC in low-resource settings124 .
Testing cervical specimens for DNA of oncogenic (high-risk) types of human papillomavirus (HPV) has entered clinical practice, but this test is used mainly to triage for colposcopy those women with cervical cytology tests categorized as atypical squamous cells of undetermined significance (ASCUS)130, 131. HPV testing is more sensitive than cervical cytology testing for identifying cervical cancer and its precursors in population screening.this test is already being incorporated into some screening programs, generally in addition to existing Pap smear screening132-135. HPV testing combined with conventional cytology is more sensitive, yet less specific than cytology alone for both the management of ASCUS136 and in primary screening137, 138.
Although cervical cancer screening, primarily with the cervical cytology smear test, has reduced the incidence of this cancer in industrialized countries, cervical cancer remains the second most common cause of death from cancer in women worldwide, because the developing world has lacked resources to implement widespread, high-quality screening programmes. Countries with low-resource settings perform others screening tests, as visual inspection with acetic acid (VIA) or with lugols iodine (VIII), also known as schillers test. Visual inspection with acetic acid involves swabbing the cervix with an acetic acid and precancerous cells turn white temporally. Applying iodine to the cervix makes precancerous lesions appear well defined, thick, with yellow or brown shaded areas. Recent data show that visual screening with lugols iodine may have higher accuracy than screening with acetic acid139. Although adequate training of health providers is required, these tests comprise important advantages because of the relatively simple application, low-cost and rely on little infrastructure139 .
Organised versus opportunistic cervical cancer screening
Organised cervical cancer screening accelerated the decline in cervical cancer incidence, in comparison with the trend in areas relying on opportunistic screening140 . The term organised screening programme is used for screening programmes organised at national or regional level, with an explicit policy, a team responsible for organisation and for health care and a structure for quality assurance141. Organised programmes comprise personal invitation to screening to all women in the target age groups at regular time intervals, and all services are provided free of charge19. On the other hand, the term opportunistic screening refers to cervical cytology testing in asymptomatic women following a recommendation made during a routine medical consultation or a consultation for an unrelated condition for example, on the basis of a possibly increased risk for developing cancer or by self-referral141, outside the schedule of an organised programme. Organised screening provides an equitable distribution of benefits to all women119. Strategies must incorporate the needs and perceptions of socially disadvantaged women, and increase their access to screening. It is of extreme importance to provide good quality screening and treatment services that reach women who are at risk142 .
A good and organized prevention program for cervical cancer must reach a high proportion of women at risk of the disease, also covering the high-risk groups, effectively test these women, treat or manage those who test positive, ensure they are followed-up, monitor and evaluate program impact143 .
There is strong evidence that well-organised screening with cytology can reduce the incidence and mortality up to 80%15. Besides reducing incidence and mortality, increased participation in screening for cervical cancer would also reduce demand for services, thereby reducing the waiting times for cancer services. In countries where wide cervical cancer screening coverage has been achieved cervical cancer incidence and death rates have fallen by more than 50%, being proved as a model for successful cancer prevention.
In the Nordic countries, following the introduction of nationwide screening in the 1960´s, cumulative mortality rates of cervical cancer showed a falling trend. Iceland had observed the greatest fall (84% from 1965 to 1982)144. In Finland age-standardised (world standard population) mortality rates decreased over 80% from the level of 7.0 deaths per 100,000 women in early 1960s to 1.2 deaths per 100,000 women in the 1990s22, 145. In Sweden and Denmark the decline was 34% and 27% between 1965 and 1982, respectively. In Norway, after the introduction of a national cervical cancer cytology program in 1995, age-standardised (World standard population) mortality rates decreased from the level of 3.0 deaths per 100,000 women in 1995 to 1.9 deaths per 100,000 women in 200622 .
In England after the introduction of an organized screening program in 1988, the cervical cancer incidence and mortality decreased around 50 from 1988 to 1997127 .
In Turin, Italy, a decrease of 20%, from 1992 to 1998, on fully invasive cervical cancer incidence was observed after the introduction of an organised programme in an area where opportunistic screening was previously conducted146 .
Cancer screening in europe
In most European countries cervical cancer screening started as an opportunistic activity, and it is still predominant in most European countries. Despite the relatively good level of resources, few national well-organised and documented programs are implemented147. A recent report on the state of the art of cancer control structures in European Union countries, Iceland, Norway and Switzerland shows that 8 countries have no organised programs (Bulgaria, Cyprus, Germany, Greece, Latvia, Luxembourg, Malta and Switzerland). Among the remaining, 14 have programmes with national coverage. Participation rate ranges between 10% and 80%, approximately. In Austria, Belgium, France Ireland, Italy, Portugal, Romania and Spain, organised programmes were implemented, but not with national coverage. A heterogeneity of age target population and in screening interval (years) is also observed. The Papanicolaou test is the most frequently used test2,148.
The first countries with organised programme were Finland in 1963, now presenting a national coverage of 97.5%, and a proportion of participation of 71%, followed by sweden with a 70% participation and 100% of national coverage and by Austria with a regional organised programme launched in 1970 with a participation of 75% of women aged between 20 and 49 years and 50% of women aged 50-69 years2.
European guidelines recommend three to five years screening intervals. the most commonly recommended interval between normal cytological tests is three years15. The interval of screening varies among European countries, most of them having programmes with three-year intervals between screening tests, except for Estonia, Finland, Neverthlands and Romania that use five years as interval. Sweden and United Kingdom perform 3/5 years screening intervals2.
Cervical cancer screening in Portugal
Cervical cancer screening in Portugal has been predominantly opportunistic and its practice has increased, especially since the early 1990s, mainly by indication from general practitioner or by demand149. Population screening programs on a national scale do not exist. Never the less, there are regional organised programs in the Central Region of Portugal, since 1990, in the region of Alentejo, since early 2008, and recently (February2009) in the North region of the country. The screening Programme of the Central Region of Portugal is performed by the general practitioners. the cytological smears are collected in the Health Centres and sent to the cytopathology laboratory of the Coimbra Cancer Institute149 .
The programme being conducted in Alentejo uses liquid based cytology. According to the Administração Regional de Saúde do Alentejo, more than 13,500 women were screened since January 2008150 .
In the North the cervical cancer screening programme began initially with a pilot phase in Centro de Saúde do Castelo da Maia (February 2009) using the liquid based cytology preceded by HPV testing as methods of screening. This screening programme aims to screen at least 70% of the eligible population20 .
Conclusion
The epidemiology of cervical cancer worldwide is strongly influenced by the existence of effective screening programmes. Cervical cancer incidence and mortality rates have decreased in countries with effective programmes. Furthermore, high incidence and mortality rates are observed in developing countries, which lack nationwide prevention programmes.the removal of incident cases through detection and treatment of pre-malignant lesions and the diagnosis of invasive lesions, at earlier and more curable stages, provide an opportunity to prevent or delay progression to invasive cancer, leading to a reduction in mortality from cancer of the cervix. The identification of oncogenic HPV infections as a necessary cause of cervical cancer has provided new directions for research and two HPV vaccines have been developed. However, early detection will remain the key-element in reducing cervical cancer since vaccination is presently only indicated for pre-exposure prophylaxis and, thus, most women will continue to rely on screening. Primary and secondary prevention strategies should coexist in order to maximize the decrease in cervical cancer incidence and mortality.
References
1. Ferlay J, Bray F, Pisani P, Parkin DM. Cancer Incidence, mortality and PrevalenceWorldwide. GLOBOCAN 2002 IARC CancerBase No 5 version 20. 2004. [ Links ]
2. The state of the art of cancer control structures in European countries in January 2008 department of Hygiene and Epidemiology, Porto University medical school, Portugal National Coordination for the Oncological diseases, Portugal 2008. [ Links ]
3. Curado MP, Edwards, B., Shin. H.R., Storm. H., Ferlay. J., Heanue. M., Boyle. P. Cancer Incidence in Five Continents, Vol. IX lyon: IARC scientific Publications No. 160; 2007. [ Links ]
4. Idotta R, Fiorino MT, Surace P, Arena F, Scopelliti I. Gynecological screening for HPV infection. Clin Exp Obstet gynecol. 2007;34(4):242-3. [ Links ]
5. Koutsky L. Epidemiology of genital human papillomavirus infection. Am J med. 1997/05/05 ed; 1997. p. 3-8. 6. [ Links ]
6. Tranbaloc P. [Natural history of precursor lesions of cervical cancer]. gynecol Obstet Fertil. 2008 Jun;36(6):650-5.
7. Bosch FX, Lorincz A, Munoz N,Meijer CJ, Shah KV. The causal relation between human papillomavirus and cervical cancer. J Clin Pathol. 2002 Apr;55(4):244-65. [ Links ]
8. Baseman Jg, Koutsky lA. The epidemiology of human papillomavirus infections. J Clin Virol. 2005 mar;32 suppl 1:s16-24. [ Links ]
9. Lowy DR, Cchiller JT. Prophylactic human papillomavirus vaccines. J Clin Invest. 2006 may;116(5):1167-73. [ Links ]
10. Paavonen J, Jenkins d, Bosch FX, Naud P, Salmeron J, Wheeler CM, et al. Efficacy of a prophylactic adjuvanted bivalent L1 virus-like-particle vaccine against infection with human papillomavirus types 16 and 18 in young women: an interim analysis of a phase III double-blind, randomised controlled trial. Lancet. 2007 Jun 30;369(9580):2161-70. [ Links ]
11. Harper dm, Paavonen J. Age for HPV vaccination.Vaccine. 2008 mar 14;26 suppl 1:A7-11. [ Links ] 2010;24[6]: 266-77
12. Moscicki AB. HPV Vaccines: today and in the Future. J Adolesc Health. 2008 Oct;43(4 suppl):s26-40. [ Links ]
13. Stanley M. Human papillomavirus vaccines versus cervical cancer screening. Clin Oncol (R Coll Radiol). 2008 Aug;20(6):388-94. [ Links ]
14. Bollen LJ, Tjong AHSP, Vander Velden J, Mol BW, Boer K, Ten Kate FJ, et al. Clearance of cervical human papillomavirus infection by treatment for cervical dysplasia. Sext Tansm Dis.1997sep;24(8):456-60. [ Links ]
15. IARC Handbooks on Cancer Prevention Cervix Cancer screening. World Health Organization; 2005. [ Links ]
16. Peto J, Ggilham C, Fletcher O, Matthews FE. The cervical cancer epidemic that screening has prevented in the UK. Lancet. 2004 Jul 17-23;364(9430):249-56. [ Links ]
17. Miles A, Cockburn J, Smith RA, Wardle J. A perspective from countries using organized screening programs. Cancer. 2004 sep 1;101(5 suppl):1201-13. [ Links ]
18. Sankaranarayanan R, Budukh AM, Rajkumar R. Effective screening programmes for cervical cancer in low-and middle-income developing countries. Bull World Health Organ. 2001;79(10):954-62. [ Links ]
19. Lynge E, Clausen LB, Guignard R, Poll P. What happens when organization of cervical cancer screening is delayed or stopped? J med screen. 2006;13(1):41-6. [ Links ]
20. Programas de rastreio da Região Norte. ARs Norte; 2009 [updated 2009; cited 23.07.2009]; Available from: http://portal.arsnorte.minsaude.pt/portal/page/portal/ARsNorte/Conte%C3%BAdos/Not%C3%Adcias/Programas%20de%20rastreio%20na%20Regi%C3%A3o%20Norte%20%20apresenta%C3%A7%C3%A3o.pdf
21. Yang BH, Bray FI, Parkin DM, Sellors JW, Zhang ZF. Cervical cancer as a priority for prevention in different world regions: an evaluation using years of life lost. Int J Cancer. 2004 Apr 10;109(3):418-24. [ Links ]
22. Engholm G, Ferlay, J. , Christensen, N., Bray, F., Gjerstorff, ML., Klint,A., Køtlum, JE., Ólafsdóttir, E., Pukkala, E., Storm, HA. NORdCAN: Cancer Incidence, mortality and Prevalence in the Nordic Countries, Version 3.4. Association of Nordic Cancer Registries. Danish Cancer society. (http://www.ancr.nu). 2009 [cited.
23. Wabinga HR, Parkin DM, Wabwire-mangen F, Nambooze S. Trends in cancer incidence in Kyadondo County, Uganda, 1960-1997. Br J Cancer. 2000 may;82(9):1585-92. [ Links ]
24. Moodley M, Moodley K. Trends of histopathology of cervical cancer among women in durban, South Africa. Eur J Gynaecol Oncol. 2009;30(2):145-50. [ Links ]
25. Franco E, Rohant. Cancer precursors : epidemiology, detection, and prevention. New York: springer; 2002. [ Links ]
26. Sant M, Allemani C, Santaquilani M, Knijn A, marchesi F, Capocaccia R. EUROCARE-4. survivalofcancerpatientsdiagnosedin1995-1999.Resultsandcommentary. EurJCancer.2009Apr;45(6):931-91. [ Links ]
27. Ponten J, Adami HO, Bergstrom R, Dillner J, Friberg Lg, Gustafsson L, et al. Strategies for global control of cervical cancer. Int J Cancer. 1995 Jan 3;60(1):1-26. [ Links ]
28. Sparen P, Gustafsson L, Friberg Lg, Ponten J, Bergstrom R, Adami HO. Improved control of invasive cervical cancer in sweden over six decades by earlier clinical detection and bettertreatment. J Clin Oncol. 1995 mar;13(3):715-25. [ Links ]
29. Verdecchia A, Guzzinati S, Francisci S, De Angelis R, Bray F, Allemani C, et al. survival trends in European cancer patients diagnosed from 1988 to 1999. Eur J Cancer. 2009 Apr;45(6):1042-66. [ Links ]
30. EUROCARE Working group. EUROCARE-3: Survival of cancer patients cases diagnosed in 1990-94. Ann. Oncol. 14 (suppl 5). 2003. [ Links ]
31. Coleman MP, Gatta G, Verdecchia A, Esteve J, Sant M, Storm H, et al. EUROCARE-3 summary: cancer survival in Europe at the end of the 20th century. Ann Oncol. 2003;14 suppl 5:v128-49. [ Links ]
32. Sant M, Aareleid T, Berrino F, Bielska Lasota M, Carli PM, Faivre J, et al. EUROCARE-3: survival of cancer patients diagnosed 1990-94-results and commentary. Ann Oncol. 2003;14 suppl 5:v61-118. [ Links ]
33. Berrino F, Capocaccia, R., Estève, J., gatta, g., Hakulinen, t., micheli, A., sant, m., Verdecchia, A. survival of Cancer Patients in Europe: the EUROCARE-2 study. France: IARC scientific Publications nº.151; 1999. [ Links ]
34. Registo Oncológico Nacional 2001 Instituto Português de Oncologia Francisco Gentil, Porto,2008. 35. [ Links ]
35. Top 10 Os 10 tumores mais frequentes na população portuguesa adulta na região sul de Portugal, no período 2000/2001. Lisboa, Portugal: Registo Oncológico Regional sul, IPOFG-EPE; 2008. [ Links ]
36. Pinheiro Ps, Tyczynski JE, Bray F, Amado J, Matos E, Parkin Dm. Cancer incidence and mortality in Portugal. Eur J Cancer. 2003 Nov;39(17):2507-20. [ Links ]
37. Registo Oncológico Regional do Norte. Instituto Português de Oncologia de Francisco gentil Centro Regional de Oncologia do Porto; 2001.
38. Registo Oncológico Regional do Centro. 2001.
39. Incidência e mortalidade 2000-2001. Lisboa: Registo Oncológico Regional do sul; 2001. [ Links ]
40. PNs em Foco. Lisboa: ministério da saúde Alto Comissariado da saúde Boletim Informativo Nº4; 2009. [ Links ]
41. Registo Oncológico Regional do Norte. Instituto Português de Oncologia de Francisco gentil Centro Regional de Oncologia do Porto; 1992.
42. Registo Oncológico Regional do Norte. Instituto Português de Oncologia de Francisco gentil Centro Regional de Oncologia do Porto; 1988.
43. Registo Oncológico Regional do Norte. Instituto Português de Oncologia de Francisco gentil Centro Regional de Oncologia do Porto; 1989.
44. Registo Oncológico Regional do Norte. Instituto Português de Oncologia de Francisco gentil Centro Regional de Oncologia do Porto; 1990.
45. Registo Oncológico Regional do Norte. Instituto Português de Oncologia de Francisco gentil Centro Regional de Oncologia do Porto; 1991.
46. Registo Oncológico Regional do Norte. Instituto Português de Oncologia de Francisco gentil Centro Regional de Oncologia do Porto; 1993.
47. Registo Oncológico Regional do Norte. Instituto Português de Oncologia de Francisco gentil Centro Regional de Oncologia do Porto; 1994.
48. Registo Oncológico Regional do Norte. Instituto Português de Oncologia de Francisco gentil Centro Regional de Oncologia do Porto; 1995.
49. Registo Oncológico Regional do Norte. Instituto Português de Oncologia de Francisco gentil Centro Regional de Oncologia do Porto;
50. Registo Oncológico Regional do Norte. Instituto Português de Oncologia de Francisco gentil Centro Regional de Oncologia do Porto; 1997.
51. Registo Oncológico Regional do Norte. Instituto Português de Oncologia de Francisco gentil Centro Regional de Oncologia do Porto; 1999.
52. Registo Oncológico Regional do Norte. Instituto Português de Oncologia de Francisco gentil Centro Regional de Oncologia do Porto; 2000.
53. Registo Oncológico Regional do Norte. Instituto Português de Oncologia de Francisco gentil Centro Regional de Oncologia do Porto; 2002.
54. Registo Oncológico Regional do Centro. 1990.
55. Registo Oncológico Regional do Centro. 1991.
56. Registo Oncológico Regional do Centro. 1992.
57. Registo Oncológico Regional do Centro. 1993.
58. Registo Oncológico Regional do Centro. 1994.
59. Registo Oncológico Regional do Centro. 1995.
60. Registo Oncológico Regional do Centro. 1996.
61. Registo Oncológico Regional do Centro. 1997.
62. Registo Oncológico Regional do Centro. 1998.
63. Registo Oncológico Regional do Centro. 1999.
64. Registo Oncológico Regional do Centro. 2000.
65. Registo Oncológico Regional do Centro. 2002.
66. Registo Oncológico Regional do Centro. 2003.
67. Registo Oncológico Regional do Centro. 2004.
68. Registo Oncológico Regional do Centro. 2005.
69. Registo Oncológico Regional do Centro. 2006.
70. Incidência e mortalidade. Lisboa: Registo Oncológico Regional do sul 1992.
71. Incidencia e mortalidade. Lisboa: Registo Oncológico Regional do sul 1989.
72. Incidência e mortalidade. Lisboa Registo Oncológico Regional do sul; 1991.
73. Incidência e mortalidade. Lisboa: Registo Oncológico Regional do sul 1993.
74. Incidência no ROR-sul. Lisboa: Registo Oncologico Regional do sul; 1998-1999.
75. Pinheiro Ps, Tyczynski JE, Bray F, Amado J, Miranda AC, Limbert E. Cancer in Portugal = Cancro em Portugal. Lyon, France: International Agency for Research on Cancer technical Publisher nº38; 2002. [ Links ]
76. Ferlay J. WHO mortality database Journal [serial on the Internet]. 2008 date.
77. Gonçalves J, Lunet N. Evolução da mortalidade por Cancro do Colo Uterino em Portugal (1980-2005). VI Congresso Português de Epidemiologia; Porto, 23 a 24 de Outubro de 2008. [ Links ]
78. Risco de morrer em Portugal. Direcção geral de saúde; 2005. [ Links ]
79. schiffman mH, Brinton lA. The epidemiology of cervical carcinogenesis. Cancer. 1995 Nov 15;76(10 suppl):1888-901. [ Links ]
80. Franco El, Duarte-Franco E, Ferenczy A. Cervical cancer: epidemiology, prevention and the role of human papillomavirus infection. CmAJ. 2001 Apr 3;164(7):1017-25. [ Links ]
81. Kufe D, Bast R, Hait W, Hong W, Polack R, Weichselbaum R, et al. Cancer medicine 7. Hamilton, Ont.; lewiston, Ny [distributor]: American Cancer society BC decker; 2006.
82. Munoz N, Castellsague X, de Gonzalez AB, GissmannL. Chapter 1: HPV in the etiology of human cancer. Vaccine. 2006 Aug 31;24 suppl 3:s3/1-10. [ Links ]
83. Weaver BA. Epidemiology and natural history of genital human papillomavirus infection. J Am Osteopath Assoc. 2006 mar;106(3 suppl 1):s2-8. [ Links ]
84. Kjaer sK, Chackerian B, van den Brule AJ, svare EI, Paull g, Walbomers Jm, et al. High-risk human papillomavirus is sexually transmitted: evidence from a follow-up study of virgins starting sexual activity (intercourse). Cancer Epidemiol Biomarkers Prev. 2001 Feb;10(2):101-6. [ Links ]
85. Marrazzo JM, Koutsky LA, Kiviat NB, Kuypers JM, Stine K. Papanicolaou test screening and prevalence of genital human papillomavirus among women who have sex with women. Am J Public Health. 2001 Jun;91(6):947-52. [ Links ]
86. Cox Jt. Epidemiology of cervical intraepithelial neoplasia: the role of human papillomavirus. Baillieres Clin Obstet gynaecol. 1995 mar;9(1):1-37. [ Links ]
87. Shepherd J, Peersman G, Weston R, Napuli I. Cervical cancer and sexual lifestyle: a systematic review of health education interventions targeted at women. Health Educ Res. 2000 dec;15(6):681-94. [ Links ]
88. Ashford l, Collymore Y. Preventing cervical cancer worldwide. Washington, DC.: Population Reference Bureau; 2005. [ Links ]
89. Walboomers JM, Jacobs MV, Manos MM, Bosch FX, Kummer JA, Shah KV, et al. Human papillomavirus is a necessary cause of invasive cervical cancer worldwide. J Pathol. 1999 sep;189(1):12-9. [ Links ]
90. Smith JS, Lindsay L, Hoots B, Keys J, Franceschi S, Winer R, et al. Human papillomavirus type distribution in invasive cervical cancer and high-grade cervical lesions: a meta-analysis update. Int J Cancer. 2007 Aug 1;121(3):621-32. [ Links ]
91. Clifford gm, smith Js, Plummer m, Munoz N, Franceschi S. Human papillomavirus types in invasive cervical cancer worldwide: a meta-analysis. Br J Cancer. 2003 Jan 13;88(1):63-73. [ Links ]
92. Munoz N, Bosch FX, de Sanjose S, Herrero R, Castellsague X, Shah KV, et al. Epidemiologic classification of human papillomavirus types associated with cervical cancer. N Engl J Med. 2003 Feb 6;348(6):518-27. [ Links ]
93. de Villiers Em, Fauquet C, BrokertR, Bernard HU, zur Hausen H. Classification of papillomaviruses. Virology. 2004 Jun 20;324(1):17-27. [ Links ]
94. Franco El, Villa ll, Sobrinho JP, Prado JM, Rousseau MC, Desy M, et al. Epidemiology of acquisition and clearance of cervical human papillomavirus infection in women from a high-risk area for cervical cancer. J Infect dis. 1999 Nov;180(5):1415-23. [ Links ]
Nuno Lunet
Serviço de Higiene e Epidemiologia, Faculdade de Medicina da Universidade do Porto. Al. Prof. Hernâni Monteiro 4200-319 Porto, Portugal. Email: nlunet@med.up.pt














