Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Arquivos de Medicina
On-line version ISSN 2183-2447
Arq Med vol.24 no.4 Porto Aug. 2010
INVESTIGAÇÃO ORIGINAL
Evaluation of Delirium in Postoperative Patients
Avaliação do Delirium no Pós operatório de Cirurgia Major
Fernando José Abelha*, Miguela Botelho*, Vera Fernandes*, Alice Santos*, Isabel Dias**, Henrique Barros***
* Department of Anesthesia, Hospital de São João, Porto;
**Post Anesthesia Care Unit, Hospital de São João, Porto;
*** Department of Hygiene and Epidemiology, University of Porto Medical School, Porto
ABSTRACT
Background: Postoperative delirium is associated with increased length of stay, both in hospital and in the Post Anesthesia Care Unit (PACU), more frequent medical complications, and increased mortality. Intensive Care Delirium Screening Checklist (ICDSC) score of 4 or more correlates well with a psychiatrists clinical diagnosis of delirium with an excellent interobserver reliability between nurses and critical care physicians. The aim of this study was to translate, retranslate and validate ICDSC for use in Portuguese PACU settings.
Methods: The translation of the ICDSC was done according to the guidelines suggested by The Translation and Cultural Adaption. For the validation process we have prospectively studied its applicability in a prospective study carried out, during 1 month period, in a PACU with five intensive care beds. Research staff physicians and nurses prospectively performed daily evaluation of each patient once per day using ICDSC. Interrater reliability was calculated using kappa statistics.
Results: Research staff physicians and nurses studied 79 patients eligible for the scale rating. We did record 107 paired observations. Nine (11.4%) patients were diagnosed as having delirium by both research staff physicians and nurses. In the 107 paired observations, overall interrater reliability was very good between nurses and the research staff physician (Kappa statistics ranged 0.790 to 0.933).
Conclusion: The translation of the ICDSC showed good correlation with the original version and could therefore be applicable in Portuguese PACU settings. The interrater variability was very good and this translated version of ICDSC was suitable for delirium screening by nurses and physicians.
Key-words: postoperative; delirium; intensive care; outcome.
RESUMO
Introdução: O Delirium no pós-operatório está associado a aumento do tempo de internamento na Unidade de Cuidados Pós Anestésicos (UCPA), aumento de complicações e aumento da mortalidade. A pontuação do Intensive Care Delirium Screening Checklist (ICDSC) tem boa correlação com o diagnóstico clínico psiquiátrico do delirium, apresentando excelente concordância entre diferentes grupos de profissionais de saúde. O objetivo deste estudo foi a Tradução e validação do ICDSC para utilização em Unidades Pós Anestésicas Portuguesas.
Métodos: A traduçãodo ICDSC foi efetuada de acordo com as recomendações sugeridas pelo The Translation and Cultural Adaption Group. Para o processo de validação foi efetuado um estudo prospectivo durante 1 mês numa UPA com 5 camas de cuidados intensivos. Foi efetuada pelo médico e enfermeiros da unidade a avaliação diária da versão portuguesa do ICDSC para cada doente. A concordância entre avaliações foi calculada utilizando o valor kappa.
Resultados: Foram estudados 79 doentes incluídos no estudo e foram registadas 107 observações emparelhadas. Nove doentes (11,4%) apresentaram critérios de delirium quer pela avaliação médica quer pela dos enfermeiros. Verificou-se uma boa concordância entre avaliações realizadas pelos diferentes profissionais de saúde (valor kappa entre 0,790 e 0,933 para cada item da lista ICDSC).
Conclusão: A tradução do ICDSC evidenciou boa correlação com a versão original, podendo assim ser utilizada em UCPA portuguesas. Este trabalho revelou excelente concordância entre as diferentes avaliações. A versão traduzida do ICDSC foi adequada para avaliação do delirium pelos diferentes profissionais de saúde.
Palavras-chave: pós-operatório; delirium; cuidados intensivos; resultados.
Introduction
Postoperative delirium is associated with poor outcome, including increased length of stay in hospital and Post Anesthesia Care Unit, more frequent medical complications, and increased mortality (1-6).
Delirium is often the first presenting feature of physical illness or drug toxicity, and a failure to detect this may lead to delay in diagnosing and treat the underlying cause [8]. Early recognition and treatment of delirium is the key component in reducing the duration and severity of delirium and negative outcomes (7-9).
Symptoms of acute confusion among ICU patients are still given different definitions and named in a variety of different terms. The present lack of a fully accepted definition and a homogeneous classification for mental disturbances has been an obstacle for a uniform definition.
The American Psychiatric Association published in 1994
The Diagnostic and Statistical Manual of Mental Disorders IV (DSM IV) (10) in which the concept of delirium is described by the definition of Lipowski (11). Critical care patients have life-threatening illness sometimes undergoing mechanical ventilation and experience mental impairment as a result of their sedation or other medical treatment and are in an advanced technical environment (12,13). These circumstances could bias the use of the manual from DSM IV (14).
It can be difficult for intensive care specialists and for nurses to detect delirium in the ICU as multiple factors influence a clear clinical diagnosis. Furthermore, because of the severity of illness and the lack of verbal communication in critically ill ICU patients, cognitive assessment is particularly difficult in this patient population (15).
Given the high prevalence of delirium among critical ill patients and the negative clinical outcomes associated with it, current practice guidelines recommend that ICU patients be routinely screened for delirium using a validated screening tool (16).
In 2001, Bergeron et al. (17) created the Intensive Care Delirium Screening Checklist (ICDSC). The ICDSC includes eight items based on the Diagnostic and Statistical Manual of Mental Disorders (DSM) criteria and features of delirium including: inattention; disorientation; hallucination-delusion psychosis; psychomotor agitation or retardation; inappropriate speech or mood; sleep/wake cycle disturbances; and symptom fluctuation according to a total score system from 0 to 8 points. In the same study an ICDSC score of 4 or more correlates well with a psychiatrists clinical diagnosis of delirium and has a sensitivity of 99% and a specificity of 64% with an excellent interobserver reliability among nurses and between nurses and critical care physicians.
As far aswe know, in Portugal, there is no commonly used or any single instrument/method to test the development of ICU syndrome/delirium. However, a review and examination of the literature shows that the ICDSC is a commonly used instrument for detecting delirium in international ICU settings. Thus, the ICDSC could be very useful in Portuguese ICU settings. The ICDSC was translated to Portuguese language and integrated in our daily assessment for delirium and carried out by our PACU bedside nurses regularly.
The aim of this study was to translate, retranslate and validate ICDSC for use in Portuguese ICU settings.
Methods
Translation and retranslation
After permission from Bergeron N et al., translation of the instrument was done according to the guidelines suggested by The Translation and Cultural Adaptation group. This group has proposed guidelines and a model for principles of good practice in the translation process (18).
The translation process is described as follows: preparation, forward translation, reconciliation, back translation, back translation review, harmonization, cognitive debriefing, review of cognitive debriefing results and finalization and proof reading.
Preparation
Permission to use the instrument ICDSC from the ICDSC author developer (Bergeron N) was asked and accepted.
Forward translation/reconciliation
A group of experienced intensive care nurses, the author and a professional translator, translated the source text of the English version of the ICDSC to Portuguese. This was carried out independently and then they met to compare their translations.
Reconciliation
To solve the discrepancies between original independent translations and seek for the agreement between individual preferences.
Back translation
The final Portuguese version was given to a professional translator for retranslation to English without seeing the original version.
Back translation review
The group who had made the original translation compared the retranslated version of the instruments to the original and discrepancies were identified and corrected.
Harmonization
The retranslated version was sent to Bergeron N et al. for approval and acceptance of the Portuguese version.
Cognitive debriefing
Ten experienced nurses specialized in intensive care were asked to read and examine the translated and accepted instruments to evaluate cognitive equivalence and to detect any unclear words, concepts or elements that they were unable to understand.
Review of cognitive debriefing results and finalization
The findings of the debriefing process were incorporated to improve the performance of the translation. This involved the validation process testing the applicability of the Portuguese version of the instruments used in a Portuguese PACU with 5 ICU beds.
Patients and validation into Portuguese icu setting
The institutional review board of Hospital de São João approved the study and informed consent was obtained preoperatively from each study patient. This prospective study was carried out in the multidisciplinary Post-Anaesthesia Care Unit with five intensive care beds, at the Hospital São João, an 1100-bed community teaching hospital in Porto, Portugal. All consecutive Portuguese-speaking, adult patient, admitted to the 5 ICU beds of the PACU, who underwent major scheduled or emergency non-cardiac surgery, between 1 february 2009 and 3 March 2009 (31 days) and who are expected to remain in the hospital postoperatively for more than 48 hours were eligible to the study.
Patients who did not provide or were incapable of providing informed consent, had a disease of the central nervous system, had been admitted for neurological or cardiac surgery, had Parkinsons disease, alcoholism, drug dependence or were admitted with a diagnosis of delirium or had antipsychotic medication were excluded.
Delirium evaluation
Research staff physicians and nurses prospectively performed a neurologic evaluation of each patient once per day using the translated Portuguese version of the Intensive Care Delirium Screening Checklist (ICDSC).
Each admitted patient had their chart reviewed and was evaluated for their duration of stay or up to a maximum of 5 days. The checklist was administered within 24 hours of admission and daily. The information utilized included information from the last 24 hours collected from the patient, the primary nurses evaluation, and the chart. The first author of this article performed all the observations recorded, but the observer nurse could vary from time to time depending on who was caring for the patient. After finishing the test the instrument was completed independently and separately by the first author as a staff PACU physician and by the observer nurse.
According to ICDSC, a patient was defined as a delirium-positive if their test score was 4 or more points.
Statistical method
Descriptive analyses of variables were used to summarize data and the Mann-Whitney U test was used to compare continuous variables between two groups of subjects and Fishers exact test was used to compare proportions between groups of subjects.
The homogeneity of the questionnaire was evaluated by calculating Cronbachs alpha homogeneity coefficients.
Interrater reliability was calculated using kappa statistics for each feature in the instrument. Cohens kappa and weighted kappa were used to estimate the agreement rates. The strength of agreement of the kappa statistics refers to the guidelines from Landis and Koch (19).
SPSS sotware version 15.0 (SPSS inc., Chicago, IL) was used in the statistic analyses.
Results
Patient characteristics
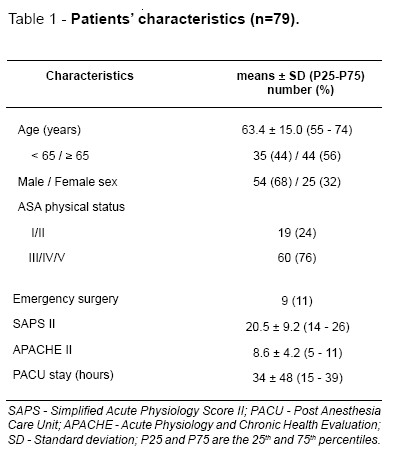
Research staff physician (the first author) and nurses completed evaluations in ninety-one patients over 145 patient evaluation days representing 94% of PACU occupation. Eleven were excluded because their level of consciousness did not allow for evaluation according to the ICDSC definition. One patient was excluded because he was admitted on antipsychotic medication for schizophrenia. Seventy-nine patients were studied and considered eligible for the scale rating. For these patients we had 107 paired observations. The characteristics of the population are described in Table 1.
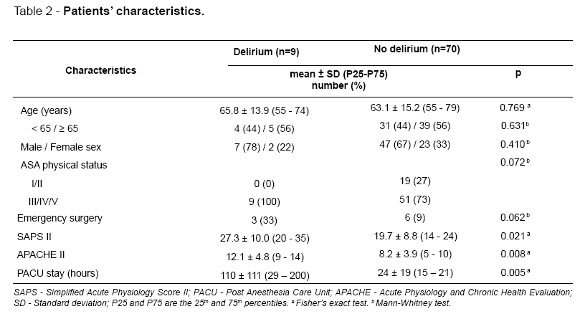
Nine (11.4%) patients were diagnosed as having delirium by both research staff physician and nurses.
Patients with delirium were more severely ill (median SAPS II was 31 versus 18, p=0.021 and median APACHE II was 12 versus 8, p=0.008) and stayed longer in the PACU (median length of stay in the PACU was 84 hours versus 18 hours, p=0.005) (Table 2).
The item reliability of the checklist calculated by alpha-homogeneity coefficients (Cronbach alpha) ranged from 0.884 to 0.967.
For the checklist interrater reliability were calculated, for each item, as a total score and for patients scored 4 or more points. In the 107 paired observations performed, overall interrater reliability for each ICDSC item and for the total score was considered very good between nurses and the research staff physician represented by the first author. For the total ICDSC score Cohens kappa and weighted kappa were respectively 0.77 (0.66-0.88) and 0.92 (0.73-1.0). For the diagnosis of delirium (score of 4 or more points) agreement was complete (kappa=1) (Table 3).
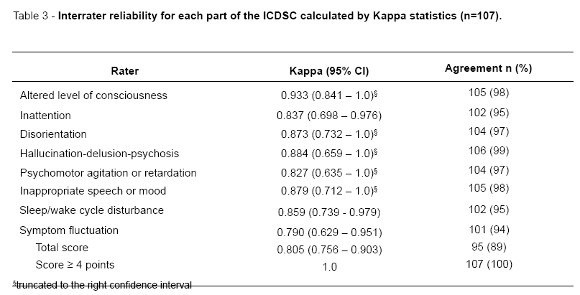
The absolute agreement between nurses and staff research physicians observed for each item range between 94 and 99%. For the total score agreement was 89% and there was total agreement for patients evaluated with a score of 4 or more.
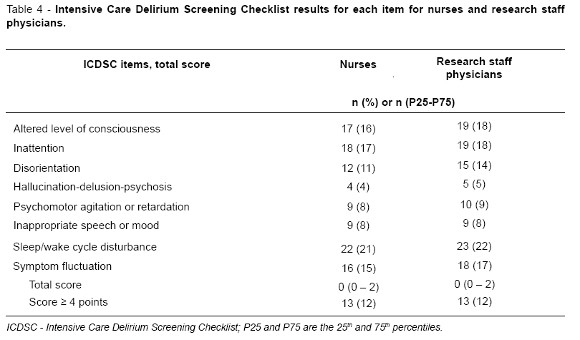
Table 4 describes each item score and median with quartiles total score obtained by patients when they were observed by nurses or research staff physicians.
Translation process
The translation process was done as described in the Methods section. This process was uneventful and the ICDSC was successfully translated to Portuguese and its final version accepted by the original author as required. After that, the ICDSC was evaluated in the described series of adult PACU patients.
The Portuguese translation group met several times, at weekly intervals, to allow for reflection and a consensus was reached on the instruments contents and structure. Bergeron N et al. accepted the Portuguese retranslated version of the ICDSC.
According to the team involved in the process the cognitive debriefing and reading of the checklist there were no unclear words that they were unable to understand.
Discussion
The incidence of postoperative delirium in the PACU was 11.4% a similar result that was observed in a recent published study by Radtke et al. (20) in postoperative patients after major surgery.
In our study patients that developed delirium in postoperative period were more severely ill and stayed longer in the PACU what is also in accordance with which is currently known and has yet been published about delirium in postoperative patients (20-23). Conversely, age also known to be an important risk factor for delirium, was not higher for patients that developed delirium what may be explained by the higher mean age of our sample population.
Intensive Care Delirium Screening Checklist has been proved to be a high sensitive screening test to detect delirium and since Bergeron et al. (17) published his results in evaluating this diagnostic tool for delirium others have used this questionnaire in the postoperative period and after major surgery (24,25).
This study showed a high reliability using the translated ICDSC that was successfully used in the clinical trial.
The ICDSC was translated by a group of researchers, experienced nurses in intensive care and a professional translator and this experience was very important in the process of translation because the meaning of the words and concepts were specifically used in the context of the PACU with intensive care beds.
We had used the generic guidance in the area of translation and cultural adaptation promoted by ISPOR TCA task force (18) and completed all steps and critical components recommended.
In our study comparisons with gold standard tool for delirium diagnostic were not done but we rely on the studies made by others (17) in the original version of ICDSC. In our sample we and have calculated the Cronbach alpha for internal consistency; the values observed for the test were satisfactory to estimate the reliability of the scale in what concernes that analysis.
Agreement between the treating critical care physicians and psychiatrist occurred and was already reported for ICDSC by the author that first described the checklist [26]. In the same study Bergeron N et al. declares that in their study nurses and physicians were strikingly homogeneous in terms of patient assessment. Others using different tools to assess delirium had concluded that ICU nurses can detect delirium reliably and with a great degree of sensitivity and specificity (27).
In our study we have used a process improvement project promoted in a systematic fashion via the identification of essential characteristics for the effective implementation of this tool. We had promoted a planning, baseline and education phases with a great involvement of all the PACU staff in order to discuss all the relevant aspects of the project. Our aim was to improve all the aspects of evaluation using the ICDSC for screening of delirium in the PACU.
The results of our study are similar to nursing studies that have evaluated the effect of educational efforts focused on use of validated delirium screening tools [28].
With minimal training, the compliance of nurses using sedation and delirium instruments has been noted to be excellent. In the study of Pun BT et al. (29) the authors concluded that the agreement of data from bedside nurses and a reference-standard rater was very high for the delirium assessment. In our study the same physician observed all the patients and recorded one of the paired observations. The other paired observations were done by the nurses of the PACU staff that had been trained to use ICDSC and we had achieved a high level of agreement between the paired observations in what concerns each of the individual item of ICDSC and for clear cut decision for the presence or absence of delirium for which the agreement was complete.
A limitation of our study was that lack of delirium diagnostic using DSMIV criteria and for the same reason we were not able to compare our observations (made by nurses and research staff physicians) with this considered gold standard for delirium diagnostic. As a matter of fact because of that limitation we were not able to calculate the sensitivity and specificity of the translated ICDSC.
Conclusion
The Translation of the ICDSC showed good correlation with the original version and could be applicable to a Portuguese ICU setting. The interrater reliability between nurses and the medical staff was very good in the performed observations item by item and for the screening of delirium.
References
1-Shehabi Y, Riker RR, Bokesch PM, Wisemandle W, Shintani A, Ely EW; SEDCOM (Safety and Efficacy of Dexmedetomidine Compared With Midazolam) Study Group. Delirium duration and mortality in lightly sedated, mechanically ventilated intensive care patients. Crit Care Med 2010;38:2311-8. [ Links ]
2 -Leslie DL, Zhang Y, Holford TR, Bogardus ST, Leo-Summers LS, Inouye SK. Premature death associated with delirium at 1-year follow-up. Arch Intern Med 2005;165:1657-62. [ Links ]
3 -Olin K, Eriksdotter-Jönhagen M, Jansson A, Herrington MK, Kristiansson M, Permert J. Postoperative delirium in elderly patients after major abdominal surgery. Br J Surg 2005;92:1559-64. [ Links ]
4 -Thomason JW, Shintani A, Peterson JF, Pun BT, Jackson JC, Ely EW .Intensive care unit delirium is an independent predictor of longer hospital stay: a prospective analysis of 261 non-ventilated patients. Crit Care 2005;9:R375-81. [ Links ]
5 -Zakriya K, Sieber FE, Christmas C, Wenz JF Sr, Franckowiak S. Brief postoperative delirium in hip fracture patients affects functional outcome at three months. Anesth Analg 2004;98:1798-802. [ Links ]
6 -Aakerlund LP, Rosenberg. Postoperative delirium: treatment with supplementary oxygen. Br J Anaesth 1994; 72:286-90. [ Links ]
7 -Johnson J. Identifying and recognizing delirium. Dement Geriatr Cogn Disord 1999;10:353-8. [ Links ]
8 -Milisen K, Foreman MD, Abraham IL,et al. A nurse-led interdisciplinary intervention program for delirium in elderly hip-fracture patients. J Am Geriatr Soc 2001;49:523-32. [ Links ]
9 -Lundstrom M, Edlund A, Karlsson S, Brännström B, Bucht G, Gustafson Y. A multifactorial intervention program reduces the duration of delirium, length of hospitalization, and mortality in delirious patients. J Am Geriatr Soc 2005; 53:622-8. [ Links ]
10 -Association, A.P., Diagnostic and statistical manual mental disorders IV (DSM IV). p. 4th edition. Washington. [ Links ]
11 -Lipowski ZJ, Delirium. 1990: p. New York: Oxford University Press. [ Links ]
12 -Granberg A, Bergbom Engberg I, Lundberg D. Patients experience of being critically ill or severely injured and cared for in an intensive care unit in relation to the ICU syndrome.PartI.Intensive CritCare Nurs1998;14:294-307. [ Links ]
13-Granberg Axèll AI,MalmrosCW,BergbomIL,Lundberg DB. Intensive care unit syndrome/delirium is associated with anemia, drug therapy and duration of ventilation treatment. Acta Anaesthesiol Scand 2002;46:726-31. [ Links ]
14 -Tucker GJ. The diagnosis of delirium and DSM-IV. Dement Geriatr Cogn Disord 1999;10:359-63. [ Links ]
15 -Pisani MA, McNicoll L, Inouye SK. Cognitive impairment in the intensive care unit. Clin Chest Med 2003;24:727-37. [ Links ]
16 -Jacobi J, Fraser GL, Coursin DB, et al. Clinical practice guidelines for the sustained use of sedatives and analgesics in the critically ill adult. Crit Care Med 2002;30:119-41. [ Links ]
17 -Bergeron N, Dubois MJ, Dumont M, Dial S, Skrobik Y. Intensive Care Delirium Screening Checklist: evaluation of a new screening tool. Intensive Care Med 2001;27:859-64. [ Links ]
18 -Wild D, Grove A, Martin M, et al. Principles of Good Practice for the Translation and Cultural Adaptation Process for Patient-Reported Outcomes (PRO)Measures:reportofthe ISPOR Task Force for Translation and Cultural Adaptation. Value Health 2005;8:94-104. [ Links ]
19 -Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics 1977;33:159-74. [ Links ]
20 -Radtke FM, Franck M, MacGuill M, et al. Duration of fluid fasting and choice of analgesic are modifiable factors for early postoperative delirium. Eur J Anaesthesiol 2010;27:411-6. [ Links ]
21 -Inouye SK, PA Charpentier. Precipitating factors for delirium in hospitalized elderly persons. Predictive model and interrelationship with baseline vulnerability. JAMA 1996;275:852-7. [ Links ]
22 -Leung JM. Postoperative delirium: are there modifiable risk factors? Eur J Anaesthesiol 2010;27:403-5. [ Links ]
23 -Ouimet S,Kavanagh BP, Gottfried SB, Skrobik Y.Incidence, risk factors and consequences of ICU delirium. Intensive Care Med 2007;33:66-73. [ Links ]
24 -Watts G, Roberts BL, Parsons R. Delirium in the intensive care unit: searching for causes and sources. Crit Care Resusc 2007;9:26-9. [ Links ]
25 -Plaschke K, von Haken R, Scholz M, et al. Comparison of the confusion assessment method for the intensive care unit (CAM-ICU) with the Intensive Care Delirium Screening Checklist (ICDSC) for delirium in critical care patients gives high agreementrate(s).Intensive Care Med 2008;34:431-6. [ Links ]
26 -Bergeron N, Dubois MJ, Dumont M, Dial S, Skrobik Y. Intensive Care Delirium Screening Checklist: evaluation of a new screening tool. Intensive Care Med 2001;27:859-64. [ Links ]
27-Ely EW, Margolin R, Francis J, et al. Evaluation of delirium in critically ill patients: validation of the Confusion Assessment Method for the Intensive Care Unit (CAM-ICU). Crit Care Med 2001;29: 1370-9. [ Links ]
28 -Devlin JW, Marquis F, Riker RR, et al. Combined didactic and scenario-based education improves the ability of intensive care unit staff to recognize delirium at the bedside. Crit Care 2008;12:: p. R19. [ Links ]
29 -Pun BT, Gordon SM, Peterson JF, et al. Large-scale implementation of sedation and delirium monitoring in the intensive care unit: a report from two medical centers. Crit Care Med 2005;33:199-205. [ Links ]
Dr. Fernando José Abelha
Departamento de Anestesiologia Hospital de São João, Alameda Prof. Hernâni Monteiro, 4200-319 Porto. E-mail: abelha@mail.telepac.pt














