Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Análise Psicológica
versão impressa ISSN 0870-8231
Aná. Psicológica vol.33 no.4 Lisboa dez. 2015
https://doi.org/10.14417/ap.962
Psychosocial and psychopathological predictors of HIV-risk injecting behavior among drug users in Portugal
Eleonora C. V. Costa1, Carla A. Paiva1, Domingos Ferreira2, Sofia Santos3
1Portuguese Catholic University, Braga, Portugal
2School of Psychology, Applied Psychology Department, University of Minho, Portugal
3Portuguese Drug and Drug Addition Institute, Braga, Portugal
ABSTRACT
Despite the introduction of needle and syringe exchange programs (NSPs), sharing of syringes and other materials remains common among injection drug users (IDUs) worldwide. For this reason, IDUs are at high-risk of HIV transmission. This paper studies the psychosocial and psychopathological determinants of sharing among IDUs. Understanding the relationship between psychological morbidity, HIV knowledge, HIV risk perception, and sharing behaviors is important to develop campaigns to curb sharing among IDUs. We recruited 120 male (76.7%) and female (23.3%) IDUs at a public outpatient treatment service in northern Portugal whose age average was 34 (sd=7.56). They were characterized for sociodemographic, clinical, and behavioral variables, as well as for knowledge on HIV transmission and prevention, HIV risk perception, and psychopathological symptoms. Almost all patients (95.8%) were tested for HIV and 31.7% were HIV positive. Half of them had a chronic disease (50.8%) and declared to engage in sharing (51.7%). Most had accurate knowledge of HIV transmission and prevention. A great majority deemed HIV risk to be high in their communities (80.8%) but deemed their personal risk to be zero or low (72.5%). Statistical analysis showed that sociodemographic variables (female sex, lower education, living alone) and psychopathological symptoms (obsession-compulsion and somatization) predict sharing. We conclude that the development and implementation of campaigns to reduce sharing among IDUs should focus more on women, IDUs living alone, as well as early assessment and intervention on psychopathological disorders.
Key words: HIV risk injecting behavior, HIV knowledge, HIV risk perception, Psychopathology, Injection drug users (IDUs), Portugal.
RESUMO
Apesar da introdução de programas de troca de agulhas e seringas (PTS), a partilha de seringas e de outros materiais permanece comum entre os utilizadores de drogas injetáveis (UDIs) em todo o mundo. Por esta razão, os UDIs estão em elevado risco de transmissão do VIH. Este artigo estuda os determinantes psicossociais e psicopatológicos da partilha entre os UDIs. Compreender a relação entre morbilidade psicológica, conhecimentos sobre o VIH, percepção de risco face ao VIH e comportamentos de partilha é importante para desenvolver campanhas de contenção de partilha entre os UDIs. Foram recrutados 120 homens (76.7%) e mulheres (23.3%) UDIs num serviço de tratamento ambulatório público no norte de Portugal, cuja média de idade foi de 34 (dp=7.56). Os participantes foram caracterizados ao nível das variáveis sócio-demográficas, clínicas e comportamentais, bem como ao nível dos conhecimentos sobre a transmissão e prevenção do VIH, percepção de risco face ao VIH e sintomas psicopatológicos. Quase todos os pacientes (95.8%) foram testados para VIH e 31.7% testaram positivo. Metade tinha uma doença crónica (50.8%) e declarou envolver-se em comportamentos de partilha (51.7%). A maioria possuía conhecimentos corretos sobre a transmissão e prevenção do VIH. A grande maioria considera que o risco face ao VIH é elevado nas suas comunidades (80.8%), mas considera o seu risco pessoal como nulo ou baixo (72.5%). A análise estatística mostrou que as variáveis sócio-demográficas (sexo feminino, baixo nível de escolaridade, viver sozinho) e os sintomas psicopatológicos (obsessão-compulsão e somatização) predizem a partilha. Concluímos que o desenvolvimento e a implementação de campanhas para reduzir a partilha entre os UDIs deve-se concentrar mais nas mulheres, nos UDIs que vivem sós, bem como na avaliação e intervenção precoces nos distúrbios psicopatológicos.
Palavras-chave: Comportamento de risco injectável face ao VIH, Conhecimentos face ao VIH, Percepção de risco face ao VIH, Psicopatologia, Utilizadores de drogas injetáveis (UDIs), Portugal.
Introduction
There are about 14 million people who inject drugs, while 1.6 million live with HIV/AIDS worldwide (United Nations Office on Drugs and Crime, 2013). In Europe, about 2.2 million people were living with HIV in 2012 (World Health Organization, 2013). Joint United Nations Program in HIV/AIDS (UNAIDS) and WHO estimates are indicative that in that year about 48 000 people in Portugal were living with HIV (UNAIDS, 2012; WHO, 2013). These cases were associated with sexual via of transmission in heterosexual couples (63.1%) and homosexual men (24.1%), and in 10% of the new cases the transmission was related with drug use, according with the estimates of National Health Institute Doutor Ricardo Jorge (INSA, 2013). According with the European Monitoring Centre for Drugs and Drug Addition (EMCDDA), in Portugal the prevalence of infectious diseases among drug users in the year 2011 was 16.5% for HIV, 4.3% for acute Hepatitis B (HBV) and 79.7% for Hepatitis C (HCV) infection (EMCDDA, 2012).
The association between injecting drug use and HIV exposure seems to result from higher risk behaviors for HIV, including sharing syringes and other objects used in intravenous drug consumption, as well as sexual risk behaviors (Degenhardt, Mathers, Vickerman, Rhodes, Latkin, & Hickman, 2010). Through multiple exposure ways to HIV infection, IDUs constitute a high risk group for the transmission of HIV and other blood borne infectious diseases, representing a major public health concern and a burden to socio-economic systems (Mathers et al., 2010; Seeman et al., 2011).
Preventive interventions directed to this at-risk group have been a priority in order to control this epidemic (AIDS Alert, 2010; AIDS Policy Law, 2013; Des Jarlais & Seeman, 2008; Meijerink, van Crevel, & van der Ven, 2013; Semaan et al., 2011), and in general they include needle and syringe programmes (NSPs), other drug treatment and/or opioid substitution therapy (OST), anti-retroviral therapy (ART), HIV serostatus testing and counseling, and promotion of condom use, according with the reference group from the United Nations (UN) on HIV and IDU (Mathers et al., 2010). Adopting the European strategy, the 2005-2012 Portuguese National Plan Against Drugs and Drug Addiction (Diário da República, Law of the Portuguese Republic, 2006; vide Resolution of the Council of Ministers nr 115/2006, 18th September), is a sign of an integrative systemic view of interventions, including individual and socio-structural factors.
Scientific evidence reports that NSPs may reduce risks associated with injecting drugs, like infectious diseases and mortality (Aspinall et al., 2013; Semaan et al., 2011). Education about risk behaviors is generally accepted as an effective way to prevent HIV/AIDS infection (Des Jarlais & Semaan, 2008) and there is evidence of a significant reduction of risk behaviors associated with syringe sharing among high risk IDUs who had a peer education intervention about HIV risk behaviors (Go et al., 2013; Mackesy-Amiti et al., 2013). Other authors argue that education alone is not sufficient in reducing risk among IDUs (Madray & van Hulst, 2000), because HIV transmission among IDUs still happens, and also because risk taking behaviors among IDUs in some studies were not influenced by knowledge about HIV transmission and prevention, educational status or history of HIV testing or serostatus (Sarkar et al., 1995).
HIV risk perception is a core element of prevailing health behavior theories such as the “Health Action Process Approach” (HAPA) (Schwarzer, 1999) and the “Health Belief Model” (Janz & Becker, 1984). Theoretically, higher HIV risk perception should make individuals adopt precaution measures. In fact, one common strategy used in HIV prevention interventions is raising awareness of risk (Crisp et al., 1993). Essien and col. (2008) found a statistically significant decrease in HIV risk perception among IDUs compared with non-IDUs. This result suggests an inverse correlation between actual risk of HIV infection and HIV risk perception. Therefore, targeting HIV risk perception, which is a significant determinant of behavior change, is essential to reduce the prevalence of HIV infection. In the study of Tsui, Lau, Xiang, Gu and Wang (2012) with 377 IDUs, the authors assessed risk perceptions (HIV transmission via unprotected sex and via syringe sharing) and behavioral intention to adopt protective risk behaviors (condom use and avoid syringe sharing totally), and their results corroborate the motivational hypothesis that risk perceptions motivate one to adopt protective behaviors.
Accurate knowledge on HIV/AIDS is a necessary but not a sufficient condition for the consistent adoption of protective behaviors. If the lack of such information contributes to an increased vulnerability to HIV/AIDS in many contexts (Goncalez et al., 2010), the lack of correct information about HIV transmission may contribute to fewer people being tested, to misperceptions about one’s level of risk, and to increased likelihood of AIDS optimism, denial, and stigmatization, among other adverse psychosocial influences (Vermeer, Bos, Mbwambo, Kaaya, & Schaalma, 2009). Bertoni and col. (2011) assessed drug users’ knowledge of HIV/AIDS and its possible association with HIV testing, and found that drug users had an increased vulnerability to HIV infection compared with the general population. Their findings also suggest that possessing inaccurate HIV/AIDS knowledge could be a barrier to HIV testing. In another study, Zafar, Brahmbhatt, Imam, Ul Hassan and Strathdee (2003) found that extremely low levels of HIV/AIDS awareness and high HIV risk behaviors were evident among drug users.
Another pathway of explanation for risk injecting behaviors among IDUs is related with high morbidity of psychiatric disorders besides drug addiction (Buckley, 2006; Santucci, 2012). Psychiatric disorders including other substance abuse, major depression disorder, anxiety, posttraumatic stress disorder, antisocial personality disorder, borderline personality disorder, and psychosis are commonly found comorbid with drug addiction (Braitstein et al., 2005; Buckley, 2006; Compton, Cottler, Shillington, & Price, 1995; Disney et al., 2006; Kirdorf et al., 2004; Mackesy-Amiti, Donenberg, & Ouellet, 2012).
Furthermore, some evidence pointed out that among IDUs, those with psychiatric morbidity have greater HIV risk behaviors (Compton et al., 1995; Disney et al., 2006; Kirdorf et al., 2004). More risk behaviors for acquiring HIV/AIDS, such as more sharing of syringes and needles in IDUs, were found among individuals with a history of suicide attempt (Sarin, Singh, Samson, & Sweat, 2013), antisocial personality disorder (Comptom, Cottler, Ben-Abdallah, Cunningham-Williams, & Spitznagel, 2000; Disney et al., 2006) and major depression (Disney et al., 2006; Kidorf et al., 2004; Wisniewski et al., 2005), these higher on women than in men, and more evident on women who inject drugs and are infected with HIV/AIDS (Wisniewski et al., 2005). Other complications, such as more somatic complaints, as fatigue symptoms and worse quality of life were also found among IDUs, and even more in those infected with HIV and HCV (Tavakkoli, Ferrando, Rabkin, Marks, & Talal, 2013). Social exclusion and discrimination were also common factors associated with HIV infection and injecting drug behaviors and related with more HIV risk behaviors (March, Oviedo-Joekes, & Romero, 2006, 2007).
This study aims to determine the main predictors of HIV risk injecting behavior in a sample of IDUs in the northern region of Portugal. Sociodemographic factors, knowledge about HIV transmission and prevention, HIV risk perception and psychopathological symptoms were the considered predictors.
Method
Sample
The sample consisted of 120 participants, 92 males and 28 females with an age average of 34 (sd=7.56), ranging between 18 and 56 years old. In terms of marital status, the vast majority of the participants were single (71.7%), and the rest were divorced (15.8%), married (2.5%) and t he remaining lived in marital union, but were not married (6.7%). Regarding the professional situation, 75.8% were unemployed, 16.7% had a job, 5% were studying and 2.5% were retired. Most of the participants (67.5%) lived with their parents or relatives, 11.7% with their husband or partner, 5.8% with friends, 9.2% alone, and 5.8% don’t have a place to live or lived in institutions (e.g., Red Cross).
Regarding the level of education, 3.3% of participants did not have qualifications, 5% had the 1st cycle of studies (4 years), 32.5% had the 2nd cycle (6 years), 35.8% had the 3rd cycle (9 years), 20.8% had secondary education (12 years) and 2.5% higher education (16 years and more). In terms of consumption, all participants consume or consumed tobacco, 85% alcoholic beverages, 92.5% cocaine, 87.5% heroin, 88.3% hashish, 52.5% LSD, 54.2% amphetamines, 55% tranquilizers and 54.2% ecstasy. The start age of consumption was, in average, 15 years (sd=3.16) and in mean its duration was 19 years (sd=6.86).
In terms of clinical and behavioral characterization of the sample, the vast majority of the participants (95.8%) have been tested for HIV and 31.7% were HIV positive. 19.2% of the HIV positive think that they got the virus by sharing material used in drug consumption and 11.7% think they got it through sexual interaction. In what concerns other diseases, 50.8% of the participants have a chronic disease, 35.8% have hepatitis C and 11.7% have hepatitis B. With regard to current consumption, the vast majority of the participants (90%) currently consume drugs, with most of them currently using intravenous drugs.
Regarding the use of condoms during sexual intercourse, 22.5% of the participants always use condoms, 62.5% use sometimes and 15% never used condoms in their sexual encounters. Half of the participants (50%) had an overdose in the past, 32.5% have already been arrested and from those 8.3% shared materials for consumption while in prison. With regard to sharing material, 51.7% of the participants have shared materials for drug use, 37.7% shared syringes and 37.5% have shared other materials like bottle caps, cotton and spoons.
Measures and procedure
Study participants were IDUs attending attending an urban clinic of the Portuguese Drug and Drug Addition Institute in northern Portugal (Centros de Respostas Integradas do Instituto da Droga e da Toxicodependência). Most patients were referred by the medical staff and after reporting injecting drugs and other materials. Patients attending medical visits during May and June 2013 were asked by the medical staff in the clinic if they would participate in a brief interview. Participants were also informed that the investigators were trying to understand the factors involved with HIV-risk injecting behavior among drug users in Portugal to improve prevention efforts. Additionally, they were told that the information shared was confidential. The study was approved by the Portuguese Drug and Drug Addition Institute Review Board and by its ethics Board as well as by the Portuguese Catholic University Board. One hundred fifty patients were approached for interviews and thirty refused to participate.
Participants completed several self-report questionnaires that had been previously adapted and validated to Portugal. Socio-demographic and clinical features, HIV knowledge, AIDS risk perception and psychopathological symptoms were assessed. The measures and their psychometric properties in this sample are described below.
AIDS-related Knowledge was assessed by fourteen questions adapted from the 1988 Public Health Service AIDS Information Survey (Hobfoll, 2000; Hobfoll et al., 2002; U.S. Public Health Service, 1988, cit. in Hobfoll, Jackson, Lavin, Britton, & Sheperd, 1994) and subsequently translated and validated into Portuguese (Costa, 2006; Costa & McIntyre, 2002). They assess one’s knowledge of HIV transmission and prevention, and have been shown to accurately measure safe-sex knowledge (Hobfoll, Jackson, Lavin, Britton, & Sheperd, 1993). The items have a 3-option response format: “wrong”, “right” and “don’t know”. The percentage of correct answers was used as summary score (higher values indicate higher knowledge). The Cronbach α internal consistency reliability for the 14 item scores was high (α=0.89). Eight of these 14 items measure knowledge of HIV transmission and produced a Cronbach’s α of 0. 82. Six items assess knowledge of how to prevent HIV infection during sexual activities (Cronbach’s α=0.83).
AIDS risk perceptions. Two items from the Women’s Health Study (Costa, 2006; Hobfoll et al., 2002; Schroder, Hobfoll, Jackson, & Lavin, 2001, adapted to Portuguese by Costa & McIntyre, 2002) assessed whether the participants’ heterosexual contacts in general, and their sexual behavior in particular, placed them at risk of HIV infection, response format being a Likert 4-point scale (1 to 4: none, low risk, moderate, higher risk). A question asked whether the participants discussed HIV/AIDS danger and prevention with their partners, response format being a Likert 3-point scale (1 to 3: with every partner, with some partners, never).
Psychopathological symptoms. Psychopathological symptoms were assessed with the Brief Symptom Inventory (BSI) (Derogatis, 1992, Portuguese version translated and adapted by Canavarro, 1995) which includes 53 items and provides nine sub-scale scores measuring a range of psychological symptoms and somatic complaints. This instrument assesses nine dimensions of psychopathology along with three global indexes that offer a summary evaluation of emotional disorders and the participant describes the degree in which each problem has affect him in the last week. The dimensions assessed were somatization, obsession-compulsion, interpersonal sensitivity, depression, anxiety, hostility, phobic anxiety, paranoid ideation and psychoticism and higher values indicate higher psychopathology. Although the General Severity Index (GSI) is the most used measure of the Brief Symptom Inventory, we used the nine sub-scales to assess the diversity of psychopathological symptoms because one of our goals is to analyze the psychopathological dimensions that better predict HIV-risk injecting behavior among drug users. The original scale shows a Cronbach α between .70 and .80. In this study the α value was .96 for the total scale, which shows an excellent internal consistency and the Cronbach α for each subscale ranges between .70 and .85: somatization (α=.80), obsession-compulsion (α=.80), interpersonal sensitivity (α=.77), depression (α=.84), anxiety (α=.83), hostility (α=.85), phobic anxiety (α=.78), paranoid ideation (α=.77) and psychoticism (α=.70).
Statistical analysis
Data were analyzed using the IBM® SPSS® (19.0 version). Internal consistency of responses to the questionnaires was assessed using Cronbach Alpha. A correlation analysis was conducted using two-tailed Pearson Correlation Test to study the relation between indicators of HIV sharing risk behaviors and potential predictor variables, with post-hoc correction test Bonferroni for p values. With regard to predictors of sharing, we develop a common model of predictors. All predictors were patronized to solve the problems of collinearity and distribution. For our current model the VIF values were all well below 10 and the tolerance statistics all well above 0.2; therefore, we can safely conclude that there is no collinearity within our data. Hierarchical linear regression analysis (enter method) were conducted to identify significant predictors of syringe sharing. The social demographic variables were included in the first step, AIDS-related Knowledge was entered in the second step and psychopathological symptoms were added to the model at last.
Results
In terms of HIV transmission knowledge the results show that most of participants (n=102, 85%) knew that sharing syringes is an effective transmission way, and had correct HIV risk knowledge about working near someone with HIV (n=91, 75.8%), eating at a restaurant in which the cooker has HIV (n=76, 63.3%), shaking hands, touch or kiss the face of someone with HIV (n=82, 68.3%), using public bathrooms (n=71, 59.2%), and being cough or sneezed by someone with HIV (n=74, 61.7%). In general participants reported accurate information regarding HIV transmission, nevertheless, incorrect information was found in some individuals that considered sharing plates, forks or glasses with someone with HIV (n=36, 30%) and risk of infection by mosquitoes or other insects infected with HIV (n=56, 46.7%) as HIV transmission ways.
In terms of HIV prevention knowledge, most of participants have correct knowledge about the prevention power of using condoms (n=112, 93.3%), having only one sexual partner without HIV (n=83, 69.2%) and consider the use of gel, foam or spermicide cream (n=65, 54.2%) as effective preventive practices. Less accurate information regarding HIV prevention knowledge was found for abstinence (n=52, 43.3%) and interrupted coitus (n=55, 45.8%).
With regard to AIDS risk perceptions, almost all participants declared that their community had some risk, with 16 participants (13.3%) believing that their community has low risk of HIV infection, 52 (43.3%) believing that their community has moderate risk of HIV infection, and 45 (37.5%) believing that their community has high risk of HIV infection. Only 7 (5.8%) believed that their community has no risk of HIV infection. In terms of personal risk, the majority of the participants believed that their behavior doesn’t put them at risk for HIV infection, with 39 (32.5%) believing being at low risk, 17 (14.2%) believing being at moderate risk, and 16 (13.3%) believing being at high risk of HIV infection. The remaining 48 participants (40%) believed that their behavior does not present any risk of HIV infection. With regard to HIV/AIDS communication, only 33 participants (27.5%) speak with all partners about HIV/AIDS. Most of the sample rarely, or never, speaks with partners about HIV/AIDS (n=57, 47.5%), or does not speak with all their partners about it (n=30, 25%).
Correlational results
In order to understand the relationship between the potential predictor variables (socio demographic variables, consumption, AIDS-related knowledge, AIDS risk perceptions and psychopathological symptoms) and general sharing behaviors, syringe sharing behaviors and sharing behaviors of other materials we performed a Pearson correlation analysis (see Table 1). Results show that general sharing behavior in the context of drug use occurs more frequently in women, in participants with low educational level, among those living alone, with early age of initiation of drug use, and with more psychopathological symptoms in all the BSI scales.
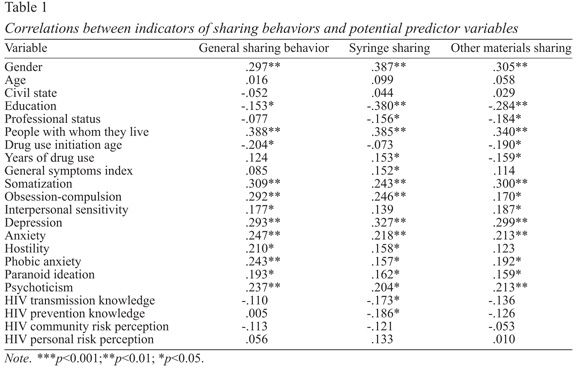
As we can see on Table 1, syringe sharing behavior in the context of drug use occurs more among women, in participants with lower education, unemployed, living alone, with a longer time of drug use, and with more psychopathological symptoms in almost all of the BSI scales (except interpersonal sensitivity), and lower knowledge about HIV transmission and prevention. Similarly, sharing of other materials in drug injection was significantly correlated with gender (females), participants with low educational level, unemployed, living alone, with chronic and long-term drug use, and more psychopathological symptoms in almost all of the BSI scales (except hostility).
Predictors of sharing injecting materials
Hierarchical linear regression analyses were conducted to estimate the relationship between gender, education, professional status, years of consumption, HIV transmission and prevention knowledge, and psychopathological symptoms as potential predictors of the dependent variable: (a) general sharing, (b) syringe sharing and (c) other materials sharing.
Regarding general sharing behavior in the context of drug use, the hierarchical linear regression model with all mentioned predictors explains 31.7% of variance of general sharing behaviors [R²=.317, F(16,103)=2.98, p<.001]. As can be seen in Table 2, females and individuals who live alone were those who display more sharing behaviors. Furthermore, 20.8% of the variance of general sharing is explained only by socio-demographic variables, and the inclusion of knowledge variables in step 2 (∆R2=.006, p>.05) and of psychopathological symptoms in step 3 (∆R2=.103, p>.05), don’t improve the model significantly.

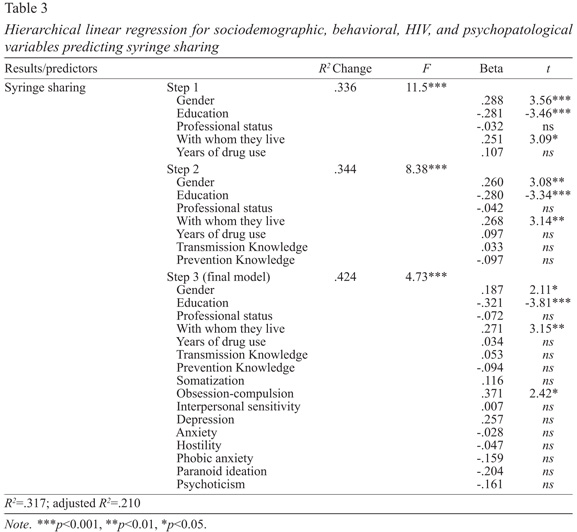
Results of the hierarchical linear regression analysis for the prediction of syringe sharing are displayed in Table 3. The final model explains 42.4% of variance of syringe sharing [R²=.424, F(16,103)=4.73, p<.001]. The analysis of individual predictors showed that gender (females), lower educational level, living alone, high obsession-compulsion symptoms were the statistically significant predictors of syringe sharing. Nevertheless, at step 1, only socio-demographic predictors explain 33.6% of the syringe sharing, and the addition of knowledge variables don’t improve significantly the model (∆R2=.008, p>.05), neither does the inclusion of psychopathological symptoms (∆R2=.080, p>.05).
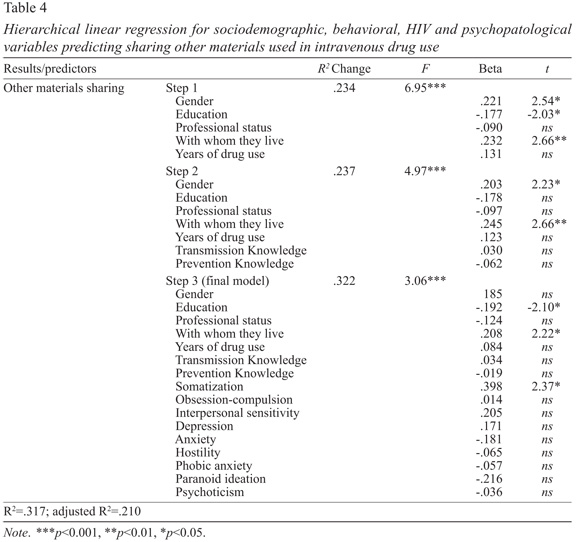
Considering the prediction of sharing other materials, all the analyzed predictors explain 32.2% of the variance of this variable [R²=.322, F(16,103)=3.06, p<.001]. As we can see in Table 4, this model shows that among individual statistically significant predictors, lower educational level, living alone, and higher somatization were related with other materials shared in injecting drug use. Socio-demographics explain 23.4% of the variance, and neither the addition of knowledge variables in step 2 (∆R2=.003, p>.05), nor the psychopathological symptoms improve significantly the final model (∆R2=.086, p>.05).
Discussion
Our findings show that three in each four participants were males, and had an average age of 34 years old, a result consistent with other community surveys and clinical samples in Portugal (EMCCDA, 2012). The majority were single, unemployed, and reported a chronic use of illicit substances starting in adolescence. Corroborating other authors findings on HIV risk behaviors among IDUs (Disney et al., 2006; Kirdorf et al., 2004; Mackesy-Amiti et al., 2012), our results showed a pattern of multiple substance abuse (e.g., tobacco, alcohol, cocaine, heroin, etc.), loss of control of drug use and deviant behaviors – half of the sample had an overdose, some individuals had been arrested and most of these shared materials while in prison. These results show the social repercussions of drug addiction, and early age of drug use initiation suggests the need to design primary prevention interventions beginning in adolescence.
Besides de social disintegration, drug addiction constitutes also a public health concern. In the last decades, worldwide and also in Portugal (Barros, 2012; WHO, 2013), maybe due to awareness of injecting harmful behaviors for HIV exposure, there has been a reduction of HIV among IDUs, however, something is still missing. In our sample about one in each three persons were HIV infected, and most of them believed that sharing materials in drug use was the main via of transmission. This result shows how our sample is indeed an at risk group for HIV infection and transmission, and for this reason, it is important to determine the main correlates of HIV-risk sharing behaviors in order to design effective preventive interventions. Besides, other blood borne infections were also found, as it is common in this at risk population, but in our sample the comparative percentage with general statistics (EMCDDA, 2012; INSA, 2013) was substantially inferior for HCV (35.8%), and superior for HIV (31.7%) and HBV (11.17%).
Almost all the participants in our sample had greater adherence to HIV testing and this seems to indicate that HIV testing campaigns are targeting this at risk group. Furthermore, they showed accurate knowledge about HIV transmission and prevention, but for a significant part of the sample sharing injecting materials still happens. These results did not corroborate the notion that the lack of accurate information about HIV transmission and prevention increases the vulnerability to the infection (Goncalez et al., 2010) or less HIV serostatus testing (Bertoni et al., 2011). In fact, almost all the participants in the current study were tested for HIV, and 85% of them know that “they can be infected with HIV by sharing syringes with someone with HIV”, but about a third shared syringes or other materials, and half of them shares materials in general. This suggests that other factors, besides HIV transmission and prevention knowledge, are involved in the adherence to HIV preventive measures (e.g., safe injecting practices). Most of the IDUs in this sample had accurate HIV transmission and prevention knowledge, nevertheless, behavioral change is not occurring for some IDUs that are at risk for HIV infection and for that reason cognitive behavioral interventions addressing specific skills and targeting HIV/AIDS risk behaviors are recommended. Additionally, a great majority deemed HIV risk to be high in their communities but deemed their personal risk to be zero or low. Since they have accurate HIV/AIDS knowledge we would expect that they would perceive themselves to be more at risk for HIV, once they have risk behaviors (syringe sharing and unprotected sex). Possibly, this lack of personal risk perception is interfering with the adoption of precaution measures and the common strategy used in HIV interventions of raising awareness of risk (Crisp et al., 1993; Tsui, Lau, Xiang, Gu, & Wang, 2012) should be integrated in HIV prevention interventions. In the present study, risk perception and HIV transmission and prevention knowledge were not significant predictors of sharing risk behaviors.
Some studies reported that education about HIV transmission in IDUs is a necessary and efficient way to reduce injecting risk behaviors (Aspinall et al., 2013; Go et al., 2013; Mackesy-Amiti et al., 2013), but itself alone is not totally accepted as a sufficient vector on HIV prevention (Madray & van Hulst, 2000; Palmateer, 2010; Sarkar et al., 1995). Furthermore, our results do not corroborate other authors who defend the efficacy of NSP in reducing injecting risk behaviors (Palmateer et al., 2010). Differently, our results seem to confirm Sarkar and col. (1995) results, which defend that harmful behaviors among IDUs are not influenced by knowledge on HIV transmission or HIV testing serostatus. Similar to our results, other evidence also shows that among HIV infected individuals who inject drugs about 40% still share needles or do not use condoms (Amirkhanian et al., 2011). Thus, it is a concern to understand the factors related with behavioral change and with safe injecting practices, besides education. The factors related with the adherence to HIV preventive programs among IDUs are not totally understood, and a multifactorial perspective involving more than individual dimensions, such as public health facilities or legal control of syringe and needles sharing, in order to a dissuasion of harmful behaviors on IDUs (Beletsky et al., 2014; Chakrapani, Newman, Shunmugam, & Dubrow, 2011). Pragmatic strategies, such as safe injecting practices are guiding public health policies in the reduction of harmful consequences of injecting drugs, like HIV infection, should not be taken as the ultimate goal of intervention, but rather the physical and mental treatment of these persons as well as the promotion of their social reintegration. Furthermore, primary prevention campaigns should fight against HIV and also against drug addiction, either at the community level or targeting at-risk groups.
Besides addiction, HIV serostatus, other comorbid physical and psychiatric diseases impair IDUs quality of life. Also, psychiatric disorders comorbidity such as psychosis, mood disorders (suicide and major depression) or personality disorders (Mackesy-Amiti et al., 2012) were consensually an accepted factor related with more harmful injecting practices on IDUs (Buckley, 2006; Santucci, 2012). Scientific literature consistently reports that those who have dual diagnosis have poor prognosis and non-adherence to treatment (Santucci, 2012). If the addiction could be a method to face psychopathology and the sharing behaviors could be the easiest way to get drugs, on the other way, the psychopathological symptoms could also increase the likelihood of drug use along with greater sharing behavior due to devaluation of risk behaviors common in some psychiatric disorders, and in our sample, in fact most of the participants recognized the risk in their communities but not in themselves. At one hand, it seems consensual among authors that people with a psychiatric disorder appear to be more vulnerable to HIV infection (Grassi, 1996; Logan, Cole, & Leukefeld, 2002), and this could be due to the fact that HIV increases behavioral disorganization and lowers the ability to self-control (Rabkin, McElhiney, & Ferrando, 2004; Stoff, 2004) and depressive symptoms (Norcini, 2013). Individuals with psychiatric disorders are more predisposed to have sharing behaviors (Disney et al., 2006; Sarin, Singh, Samson, & Sweat, 2013). So, we hypothesized that among IDUs, higher psychopathological symptoms could be the major reason in the explanation of sharing, and our results showed a positive relationship, but, when socio-demographics and HIV knowledge were controlled previously, only somatization and obsession compulsion symptoms remained statistically significant. Somatization symptoms predicted significantly more sharing of potentially infected syringes, possibly related with craving or as a result of chronic diseases, and obsession compulsion symptoms can be an indicator of the common urge for drug seeking in our sample, that put them at higher risk of sharing other materials when injecting drugs.
Our results showed that among all the analyzed predictors of sharing (socio-demographic variables, knowledge about HIV infection and psychopathological symptoms), gender (women) and IDUs living alone are consistent predictors of sharing behaviors. This result seems to reflect that, as a minority among IDUs, women seem to be confronted with even more challenges to cope with drug addiction and social exclusion, and the lack of social support, making them more vulnerable to HIV risk behaviors, as are harmful injecting practices. In fact, empirical evidence shows that women have more depressive symptoms than men, particularly if they are both HIV seropositive and inject drugs (Wisniewski et al., 2005). In our study, women constitute a vulnerable group for HIV infection by sharing injecting materials, however, comorbid HIV infection was not a controlled variable. Other socio-demographic variables such as lower educational status, living alone, and long-term drug use also predicted sharing injecting materials, but surprisingly knowledge about HIV did not.
Our results support the view that psychosocial and psychopathological factors seem to be interrelated and explain harmful risk injecting practices among IDUs. In our understanding, biopsychosocial framework on drug addiction (Gardner, 2011) provides an explanation for these results. In part, the chronic use of drugs may have noxious effects on brain physiological regulation mechanisms, namely on anti-reward systems (Gardner, 2011; Koob & Le Moal, 2008), resulting in compulsion to drug seeking, high allostatic load and consequently more somatic symptoms. Drug addiction is also erosive to psychosocial adaptation and results in more social discrimination and exclusion, that is higher when drug users are simultaneously seropositive, increasing psychological distress and more drug seeking to cope with this burden. To complexify the problem, a third of the participants in our study also have HIV seropositive status and literature agrees on neurobiological and psychosocial effects of HIV on brain and psychopathology, namely depression (Norcini, 2013), which in turn is associated with more risk behaviors. In our sample, depression is significantly correlated with sharing but lacks its predictive power when other variables are considered in the regression model. HIV status was not a controlled variable in the present study, an aspect to be considered in future research.
In the current study causality and etiological aspects were not addressed themes, because of methodological limitations of a cross-sectional study and correlation analysis. In future studies longitudinal risk trajectories of IDUs, encompassing multifactorial aspects associated with drug addiction and psychiatric disorders as well as their relation with HIV risk behaviors, should be further understood. Some study limitations were already addressed. Nevertheless, caution should be used when generalizing the results to other drug users. Also, we have to consider the limitations of data based on self-report and the relatively small sample size. There is a problem in using self-report questionnaire for assessing psychopathology among drug users because they might be under the influence of substances when answering them and they also might not understand some of the questions, leaving room for misreporting. Assessment by researchers/clinicians allows assessing comorbid mental and substance-use disorders and allows better diagnostic decisions. Indeed, several types of relationships between substance use and mental disorders are possible. Substance use may be causing the psychopathology, substance use may be secondary to the psychopathology, or the mental disorder and the substance-use problems may be coincidental and not related to each other in one of the ways described above.
Despite these limitations, this study contains a number of findings that may contribute to HIV prevention efforts in IDUs directing the attention to new target variables. Knowledge of HIV transmission and prevention may not be sufficient to reduce IDUs’ harmful risk behavior without improving personal risk perception, motivation, social support and mental health treatment.
In conclusion, this study provides evidence that reinforces the implementation of HIV preventive interventions, articulating both individual and social structural dimensions in a systemic integrated way. Our results did not corroborate health behavior theories (Janz & Becker, 1984; Schwarzer, 1999). In spite of it, psychosocial factors and psychopathological symptoms, in particular somatization and obsessive-compulsive symptoms seem to explain better sharing than HIV knowledge and risk perception. Some support for socio-demographic variables was found, such as female gender and those living alone need further attention in order to reduce HIV harmful behaviors. In our opinion, biopsychosocial model of drug addiction (Gardner, 2011) provides a good explanation for our findings, strengthening the interrelationship between physiological aspects of drug addiction, social exclusion and psychological distress and high allostatic load. In fact half of the participants suffer from chronic diseases, a third of them were infected with HIV and/ or other infectious diseases, a result that shows that drug addiction constitutes a serious life-threatening problem and encompasses negative social repercussions. The definition of main predictors of HIV risk behaviors seems to indicate the need to focus more on gender issues and on socially isolated individuals, and provide treatment to somatic and craving symptoms, in order to reduce sharing.
References
AIDS Alert. (2010). Can ‘seek and treat’ strategy stop HIV epidemic among injection drug users?. Seeking a “tipping point” toward elimination. AIDS Alert, 25, 121-123.
AIDS Policy Law. (2013). PrEP reduces HIV infection in injection drug users. AIDS Policy & Law, 28, 4. [ Links ]
Amirkhanian, Y. A., Kelly, J. A., Kuznetsova, A. V., DiFranceisco, W. J., Musatov, V. B., & Pirogov, D. G. (2011). People with HIV in HAART-Era Russia: Transmission risk behavior prevalence, antiretroviral medication-taking, and psychosocial distress. AIDS Behavior, 15, 766-777. [ Links ]
Aspinall, E. J., Nambiar, D., Goldberg, D. J., Hickman, M., Weir, A., Van Velzen, E., . . . Hutchinson, S. J. (2013). Are needle and syringe programs associated with a reduction in HIV transmission among people who inject drugs: A systematic review and meta-analysis. International Journal of Epidemiology [Advance online publication]. [ Links ]
Barros, H. (2012). HIV incidence in drug users. A cohort study in Portugal [On-Line]. Available: http://www.emcdda.europa.eu/attachements.cfm/att_195208_EN_10%20Portugal.pdf [ Links ]
Beletsky, L., Heller, D., Jenness, S.M., Neaiqus, A., Gelpi-Acosta, C., & Hagan, H. (2014). Syringe access, syringe sharing, and police encounters among people who inject drugs in New York City: A community level perspective. International Journal of Drug Policy, 25, 105-111. [ Links ]
Bertoni, N., Singer, M., Silva, C. M. F. P., Clair, S., Malta, M., & Bastos, F. I. (2011). Knowledge of AIDS and HIV transmission among drug users in Rio de Janeiro, Brazil. Harm Reduction Journal, 8, 5. [ Links ]
Braitstein, P., Montessori, V., Chan, K., Montaner, J. S., Schechter, M. T., O’Shaughnessy, M. V., & Hogg, R. S. (2005). Quality of life, depression and fatigue among persons co-infected with HIV and hepatitis C: Outcomes from a population-based cohort. AIDS Care, 17, 505-15.
Buckley, P. F. (2006). Prevalence and consequences of the dual diagnosis of substance abuse and severe mental illness. The Journal of Clinical Psychiatry, 67, 5-9. [ Links ]
Canavarro, M. (1995). Inventário de Sintomas Psicopatológicos – B.S.I. [Brief Symptom Inventory – B.S.I]. In M. Simões, M. Gonçalves, & L. Almeida (Eds.), Testes e provas psicológicas em Portugal [Assessment and psychological instruments in Portugal] (pp. 95-109). Braga: APPORT/SHO.
Chakrapani, V., Newman, P. A., Shunmugam, M., & Dubrow, R. (2011). Social structural contexts of needle and syringe sharing behaviors of HIV positive injecting drug users in Manipur, India: A mixed methods investigation. Harm Reduction Journal, 13, 8-9. [ Links ]
Compton, W. M., Cottler, L. B., Ben-Abdallah, A., Cunningham-Williams, R., & Spitznagel, E. L. (2000). The effects of psychiatric comorbidity on response to an HIV prevention intervention. Drug and Alcohol Dependence, 58, 247-257. [ Links ]
Compton, W. M., Cottler, L. B., Shillington, A. M., & Price, R. K. (1995). Is antisocial personality disorder associated with increased HIV risk behaviors in cocaine users?. Drug and Alcohol Dependence, 37, 37-43. [ Links ]
Costa, E. (2006). Avaliação da eficácia relativa de duas intervenções psicoeducativas dirigidas à prevenção da sida e promoção da saúde em mulheres com risco para o VIH [Evaluation of efficacy of two psychoeducational interventions to HIV/ AIDS prevention and health promotion in women at risk for HIV]. Unpublished doctoral dissertation, University of Minho, Braga, Portugal. [ Links ]
Costa, E., & McIntyre, T. (2002). Portuguese translation and adaptation of the questionnaires from women’s health empowerment project. Unpublished manuscript, Department of Psychology, Minho University, Braga, Portugal.
Crisp, B., Barber, J., Ross, M., Wodak, A., Gold, J., & Miller, M. E. (1993). Injecting drug-users and HIV/AIDS – Risk behaviors and risk perception. Drug and Alcohol Dependence, 33, 73-80.
Des Jarlais, D. C., & Semaan, S. (2008). HIV prevention for injecting drug users: The 25 years and counting. Psychosomatic Medicine, 70, 606-611. [ Links ]
Derogatis, L. R. (1992). The Brief Symptom Inventory (BSI): Administration, Scoring and Procedures Manual-II. Minneapolis: National Computer Systems. [ Links ]
Diário da República [Law of the Portuguese Republic]. (2006). Plano nacional contra a droga e toxicodependência [National plan against drug and drug addiction]. Resolution of the council of ministers, number 115, on 18 September 2006.
Disney, E., Kidorf, M., Kolodner, K., King, V., Peirce, J., Beilenson, P., & Brooner, R. K. (2006). Psychiatric comorbidity is associated with drug use and HIV risk in syringe exchange participants. The Journal of Nervous and Mental Disorders, 194, 577-583. [ Links ]
Essien, E., Ogungbade, G., Ward, D., Fernandez-Esquer, M., Smith, C., & Holmes, L. (2008). Injecting drug use is associated with HIV risk perception among Mexican Americans in the Rio Grande Valley of South Texas, USA. Public Health, 122, 397-403. [ Links ]
European Monitoring Centre for Drugs and Drug Addiction (EMCDDA). (2012). Country overviews: Portugal [On-Line]. Retrieved from http://www.emcdda.europa.eu/publications/country-overviews/pt [ Links ]
Gardner, E. L. (2011). Addiction and brain reward and antireward pathways. Advances in Psychosomatic Medicine, 30, 22-60. [ Links ]
Go, V. F., Frangakis, C., Le Minh, N., Latkin, C. A., Ha, T. V., Mo, T. T., . . . Quan, V. M. (2013). Effects of an HIV peer prevention intervention on sexual and injecting risk behaviors among injecting drug users and their risk partners in Thai Nguyen, Vietnam: A randomized controlled trial. Social Science & Medicine, 96, 154-164. [ Links ]
Goncalez, T., Sabino, E., Sales, N., Chen, Y., Chamone, D., Busch, M., . . . McFarland, W. (2010). Human immunodeficiency virus test-seeking blood donors in a large blood bank in São Paulo, Brazil. Transfusion, 50, 1806-1814. [ Links ]
Grassi, L. (1996). Risk of HIV infection in psychiatrically ill patients. AIDS Care, 8, 103-116. [ Links ]
Hobfoll, S. (2000). Grant application – Women’s health empowerment project. Unpublished manuscript, Department of Psychology, Kent State University, USA.
Hobfoll, S., Jackson, A., Lavin, J., Britton, P., & Sheperd, J. (1993). Safer sex knowledge, behaviour, and attitudes of inner-city women. Health Psychology, 12, 481-488. [ Links ]
Hobfoll, S., Jackson, A., Lavin, J., Britton, P., & Sheperd, J. (1994). Reducing inner city women’s AIDS risk activities: A study of single pregnant women. Health Psychology, 13, 397-403.
Hobfoll, S., Bansal, A., Schurg, R., Young, S., Pierce, C., Hobfoll, I., & Johnson, R. (2002). The impact of perceived child physical and sexual abuse history on Native American women’s psychological well-being and AIDS risk. Journal of Consulting and Clinical Psychology, 70, 252-257.
Instituto Nacional de Saúde Doutor Ricardo Jorge (INSA). (2013). Infecção VIH/SIDA: A situação em Portugal a 31 de Dezembro de 2013. [HIV/AIDS: The situation of Portugal in 31 December 2013]. Lisboa: Instituto Nacional de Saúde Doutor Ricardo Jorge (Departamento de Doenças Infecciosas do INSA). Unidade de Referência e Vigilância Laboratorial Epidemiológica. Núcleo de Vigilância Laboratorial de Doenças Infecciosas, I.P. [ Links ]
Janz, N., & Becker, M. (1984). The health belief model – A decade later. Health Education Quarterly, 11, 1-47.
Kidorf, M., Disney, E. R., King, V. L., Neufeld, K., Beilenson, P. L., & Brooner, R. K. (2004). Prevalence of psychiatric and substance use disorders in opioid abusers in a community syringe exchange program. Drug and Alcohol Dependence, 74, 115-122. [ Links ]
Koob, G. F., & Le Moal, M. (2008). Addiction and the brain antireward system. Annual Review of Psychology, 59, 29-53. [ Links ]
Logan, T. K., Cole, J., & Leukefeld, C. (2002). Women, sex, and HIV: Social and contextual factors, meta-analysis of published interventions, and implications for practice and research. Psychological Bulletin, 128, 851-885. [ Links ]
Mackesy-Amiti, M. E., Donenberg, G. R., & Ouellet, L. J. (2012). Prevalence of psychiatric disorders among young injection drug users. Drug and Alcohol Dependence, 124, 70-78. [ Links ]
Mackesy-Amiti, M. E., Finnegan, L., Ouellet, L. J., Golub, E. T., Hagan, H., Hudson, S., . . . Garfein, R. S. (2013). Peer-education intervention to reduce injection risk behaviors benefits high-risk young injection drug users: A latent transition analysis of the CIDUS 3/DUIT study. AIDS & Behavior, 17, 2075-2083. [ Links ]
Madray, H., & van Hulst, Y. (2000). Reducing HIV/AIDS high-risk behavior among injection drug users: Peers vs. education. Journal of Drug Education, 30, 205-211. [ Links ]
March, J. C., Oviedo-Joekes, E., & Romero, M. (2006). Drugs and social exclusion in ten European cities. European Addiction Research, 12, 33-41. [ Links ]
March, J. C., Oviedo-Joekes, E., & Romero, M. (2007). Factors associated with reported hepatitis C and HIV among injecting drug users in ten European cities. Enfermedades Infecciosas y Microbiologia Clínica, 25, 91-97. [ Links ]
Mathers, B. M., Degenhardt, L., Ali, H., Wiessing, L., Hickman, M., Mattick, R. P., . . . Strathdee, S. A. (2010). HIV prevention, treatment, and care services for people who inject drugs: A systematic review of global, regional, and national coverage. Lancet, 375, 1014-1028. [ Links ]
Meijerink, H., van Crevel, R., & van der Ven, A. J. (2013). Intravenous drug use and the spread of HIV: An international perspective. Nederlands Tijdschrift voor Geneeskunde, 157, A5690. [ Links ]
Norcini, P. A. (2013). HIV, depression and compliance: The mediating role of cytokines. A review of the international literature. Rivista di Psichiatria, 48, 432-440. [ Links ]
Palmateer, N., Kimber, J., Hickman, M., Hutchinson, S., Rhodes, T., & Goldberg, D. (2010). Evidence for the effectiveness of sterile injecting equipment provision in preventing hepatitis C and human immunodeficiency virus transmission among injecting drug users: A review of reviews. Addiction, 105, 844-859. [ Links ]
Rabkin, J., McElhiney, M., & Ferrando, S. (2004). Mood and substance use disorders in older adults with HIV/AIDS: Methodological issues and preliminary evidence. AIDS, 18, 43-48. [ Links ]
Santucci, K. (2012). Psychiatric disease and drug abuse. Current Opinion in Pediatrics, 24, 233-237. [ Links ]
Sarin, E., Singh, B., Samson, L., & Sweat, M. (2013). Suicidal ideation and HIV risk behaviors among a cohort of injecting drug users in New Delhi, India. Substance Abuse Treatment, Prevention and Policy, 8, 2. [ Links ]
Sarkar, S., et al. (1995). A cross sectional study on factors including HIV testing and counseling determining unsafe injecting practices among injecting drug users of Manipur. Indian Journal of Public Health, 39, 86-92. [ Links ]
Schroder, K., Hobfoll, S., Jackson, A., & Lavin, J. (2001). Proximal and distal predictors of AIDS risk behaviours among inner-city African and European American women. Journal of Health Psychology, 6, 169-190. [ Links ]
Schwarzer, R. (1999). Self-regulatory processes in the adoption and maintenance of health behavior. Journal of Health Psychology, 4, 115-127. [ Links ]
Semaan, S., Fleming, P., Worrell, C., Stolp, H., Baack, B., & Miller, M. (2011). Potential role of safer injection facilities in reducing HIV and hepatitis C infections and overdose mortality in the United States. Drug Alcohol Dependence, 118, 100-110. [ Links ]
Stoff, D. (2004). Mental health research in HIV/AIDS and aging: Problems and prospects. AIDS, 18, 3-10. [ Links ]
Tavakkoli, M., Ferrando, S. J., Rabkin, J., Marks, K., & Talal, A. H. (2013). Depression and fatigue in chronic hepatitis C patients with and without HIV co-infection. Psychosomatics, 54, 466-471. [ Links ]
Tsui, H., Lau, J., Xiang, W., Gu, J., & Wang, Z. (2012). Should associations between HIV-related risk perceptions and behaviors or intentions be positive or negative?. PLoS ONE, 7, e52124. [ Links ]
United Nations Office on Drugs and Crime (UNODC). (2013). World Drug Report 2013. Vienna: United Nations Publication Sales. [ Links ]
United Nations Program on HIV/AIDS (UNAIDS). (2012). Report for Portugal [On-Line]. Retrieved from http://www.unaids.org/en/regionscountries/countries/portugal/ [ Links ]
Vermeer, W., Bos, A., Mbwambo, J., Kaaya, S., & Schaalma, H. (2009). Social and cognitive variables predicting voluntary HIV counseling and testing among Tanzanian medical students. Patient Education and Counseling, 75, 135-140. [ Links ]
Wisniewski, A. B., Apel, S., Selnes, O. A., Nath, A., McArthur, J. C., & Dobs, A. S. (2005). Depressive symptoms, quality of life and neuropsychological performance in HIV/AIDS: The impact of gender and injection drug use. Journal of Neurovirology, 11, 138-143. [ Links ]
World Health Organization (WHO). (2013). Key facts on HIV epidemics in Portugal and progress in 2011 [On-Line]. Retrieved from http://www.euro.who.int/_data/assets/pdf_file/0009/191088/Portugal-HIVAIDS-Country-Profile-2011-revision-2012-final.pdf [ Links ]
Zafar, T., Brahmbhatt, H., Imam, G., Ul Hassan, S., & Strathdee, S. (2003). HIV knowledge and risk behaviors among Pakistani and Afghani drug users in Quetta, Pakistan. Journal of Acquired Immune Deficiency Syndromes, 32, 394-398. [ Links ]
A correspondência relativa a este artigo deverá ser enviada para: Eleonora C. V. Costa, Portuguese Catholic University, Centro Regional de Braga, Campus Camões, 4710-362 Braga, Portugal. E-mail: eleonora@braga.ucp.pt
This work was supported by the Center for Philosophical and Humanistic Studies of the Portuguese Catholic University, funded by the Foundation for Science and Technology under grant number PEst-OE/FIL/UI0683/2014
Submissão: 04/10/2014 Aceitação: 19/08/2015














