Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Análise Psicológica
versão impressa ISSN 0870-8231
Aná. Psicológica vol.32 no.1 Lisboa mar. 2014
https://doi.org/10.14417/ap.720
Relationship between socio-demographic, clinical and psychosocial variables in patients with Type 2 Diabetes
Elisabete Gomes Costa*, Ricardo Pereira Campos**, Eleonora Cunha Costa*
* Universidade Católica Portuguesa, Braga;
** Casa de Saúde S. José, Barcelos
ABSTRACT
The aim of this study is to analyze the relationship between socio-demographic, clinical and psychosocial variables in patients with Type 2 Diabetes and to establish comparative patterns between genders with this disorder.
Patients from a primary care center were assessed through a researcher design form and through the HADS, the ESSS and the PSQI.
A total of 90 patients with Type 2 Diabetes were enrolled in this study (50% women), with a mean age of 56.67±6.41 years. The HADS depression presented a score of 3.77±2.98 and 6.70% of the sample revealed depression symptoms. As to anxiety, the HADS presented scores of 7.27±5.07 with 36.60% of the subjects revealing anxiety symptoms. Regarding social support, the results were positive and similar between genders. When it comes to sleep, the sample presented a PSQI of 8.68±2.87, with 73.30% of patients revealing poor sleep quality and 24.40% showing a sleep disorder. When comparing genders, women had higher anxiety (♀ 9.73±5.58; ♂ 4.80±2.91; p=0.000) and depression scores (♀ 4.26±2.69; ♂ 3.26±3.19; p=0.026), and worse sleep quality (♀ 9.88±7.46; ♂ 7.46±2.34; p=0.000).
In conclusion, we can state that anxiety symptoms are very prevalent in patients with Type 2 Diabetes and women are more vulnerable to anxiety, depression symptoms and poor sleep quality.
Key-words: Type 2 Diabetes, Anxiety, Depression, Social support, Sleep.
RESUMO
Com este estudo pretende-se analisar a relação entre variáveis sociodemográficas, clínicas e psicossociais em doentes com Diabetes Tipo 2 bem como estabelecer padrões comparativos entre géneros. Foram avaliados pacientes de uma Unidade de Cuidados Primários através de um formulário próprio de recolha de informação, da HADS, da ESSS e do PSQI.
A amostra consistiu num total de 90 pacientes com Diabetes Tipo 2 (50% mulheres), com idade média de 56.67±6.41 anos. A subescala depressão da HADS apresentou um score de 3.77±2.98 e 6.70% da amostra revelou sintomatologia depressiva. Quanto à ansiedade a HADS apresentou scores de 7.27±5.07 com 36.60% dos sujeitos a manifestarem sintomatologia ansiosa. No que se reporta ao suporte social, os resultados foram positivos e similares entre géneros. Em relação ao sono, a amostra apresentou um PSQI de 8.68±2.87, com 73.30% dos pacientes a manifestarem uma pobre qualidade do sono e 24.40% a manifestarem uma perturbação do sono. Ao comparar-se géneros, verificou-se que as mulheres apresentavam maiores scores de ansiedade (♀ 9.73±5.58; ♂ 4.80±2.91; p=0.000) e depressão (♀ 4.26±2.69; ♂ 3.26±3.19; p=0.026), e pior qualidade do sono (♀ 9.88±7.46; ♂ 7.46±2.34; p=0.000). Em conclusão, a sintomatologia ansiosa apresenta uma elevada prevalência em doentes com Diabetes Tipo 2 e as mulheres são mais vulneráveis à ansiedade, depressão e pior qualidade do sono.
Palavras-chave: Diabetes Tipo 2, Ansiedade, Depressão, Suporte social, Sono.
INTRODUCTION
Type 2 Diabetes is a metabolic disorder with multiple etiologies marked by chronic hyper-glycemia with carbohydrates metabolic disorders, lipid and protein resulting from deficiencies in the secretion or action of insulin, or both (Zimmernan & Walker, 2002). It is estimated that approximately 52 million of Europeans live with Diabetes with similar numbers of men and women (8.40% vs. 7.80%) between 20-79 years of age (Jakab, 2010), and approximately 12.30% of Portugals population has Diabetes with 90% having Type 2 Diabetes. This can be attributed to rapid social and cultural changes, population ageing, increasing urbanization, modification of alimentary habits, physical activity reduction and increased unhealthy life styles (Observatório Nacional da Diabetes, 2010). Furthermore, Type 2 Diabetes is strongly associated with obesity (Fagot-Campagna et al., 1998), and obesity stands out as a risk factor for DM2 (Hussain, Hydrie, Claussen, & Asghar, 2010).
We thank the patient for their participation and the Extensão de Saúde Dr. Vale Lima do ACES Cávado III Barcelos / Esposende staff for the valuable support.
When considering the relationship between Type 2 Diabetes and psychosocial factors, the studies are unanimous in pointing to a high association of anxiety/depression symptoms and these being more prevalent than in normal populations (Amorim & Coelho, 2008; Zimmernan & Walker, 2002) and recurring over time (Peyrot, 2003; Peyrot & Rubin, 1999). Anxiety/depression symptoms in Type 2 Diabetes can be associated with a poor glycemia control, low adherence to the therapeutic regimen, disorder aggravation in the long run (Amorim & Coelho, 2008) and quality of life decrease (Goldney, Phillips, Fisher, & Wilson, 2004). Studies suggest that individuals with low economic income (Nascimento, Chaves, & Grossi, 2009), older patients (Ricco, Miyazaki, & Silva, 2004), and those with less social support (Amorim & Coelho, 2008), poor glycemia control (Tellez-Zenteno & Cardiel, 2002), and inactivity (Amorim & Coelho, 2008) are more vulnerable to depression symptoms. There is no agreement regarding the relationship between depression symptoms and educational level (Amorim & Coelho, 2008; Nascimento et al., 2009; Ricco et al., 2004) or marital status (Amorim & Coelho, 2008; Nascimento et al., 2009; Tellez-Zenteno & Cardiel, 2002). However education level and marital status do not reveal any association with anxiety symptoms in patients with Diabetes (Amorim & Coelho, 2008). Literature points to an association of bad alimentary habits (Papelbaum et al., 2005) and low social support as causes of anxiety symptoms (Amorim & Coelho, 2008).
When it comes to comparisons between genders, some studies show no differences regarding depression (Ramos & Ferreira, 2011) and anxiety symptoms (Khuwaja & Kadir, 2010; Ramos & Ferreira, 2011), while the majority of the authors suggest a higher prevalence of depression (Amorim & Coelho, 2008; Gucciardi, Wang, DeMelo, Amaral, & Stewart, 2008; Khuwaja & Kadir, 2010; Roupa et al., 2009), as well as a higher prevalence of anxiety in women (Amorim & Coelho, 2008; Roupa et al., 2009). The studies also suggest that women have a higher probability of having a family history of Diabetes and of having a better social support system from care givers (Gucciardi et al., 2008).
The literature highlights a significant association between a good social support system and behaviors that promote health and well-being in patients with Type 2 Diabetes (Schiotz, Bogelund, Almdal, Jensen, & Willaing, 2012), positive associations with self-efficiency (Park & Kim, 2012), and negative associations with depression symptoms and the adhesion to the therapeutic regimen (Osborn & Egede, 2012).
Data suggests a poor sleep quality in patients with Type 2 Diabetes with PSQI scores =5, with a high prevalence of sleep disturbances ranging from 52-71% (Barone & Menna-Barreto, 2011; Knutson, Ryden, Mander, & Van Cauter, 2006).
Taking into account the bibliographic research that focuses predominantly on the analysis of depression and anxiety, evidence suggests a high prevalence in patients with Type 2 Diabetes. Differences between sexes have been sometimes contradictory or inconclusive, and the same happens with the analysis of the social support, sleep quality, and its relationship with several socio-demographic, clinical and psychosocial variables. The aim of this study is to analyze the relationship between socio demographic, clinical and psychosocial variables and to establish comparative patterns between the gender of patients with Type 2 Diabetes.
RESEARCH DESIGN AND METHODS
Subjects
The selection of the sample was based on the convenience sampling method. The patients were recruited in the primary care center Extensão de Saúde Dr. Vale Lima from the ACES Cávado III Barcelos / Esposende, Portugal. The primary care center covers a region classified as predominantly rural, with about 5.300 users, of which 300 are patients with type 1 and Type 2 Diabetes. Inclusion criteria were predefined as follows: (1) established diagnosis of Type 2 Diabetes for more than 1 year; (2) age between 18-65 years; (3) absence of cancer problems; and (4) informed consent to participate in the study. The sample was reduced from 300 to 125 patients, which culminated in 90 subjects (50% women) that agreed to take part in the study. The investigation followed the ethics and deontological principles required on scientific research.
METHODS
Socio demographic and clinical characteristics
Using a researcher-design form, participants gave information about their age, gender, studies (=1st degree; and =2nd degree), marital status (married / common law marriage; unmarried), professional status (employed; unemployed; retired), and household (living with partner; living with restricted family – sons and partner; living with extended family – sons, partners and others). In the same way, a clinical data sheet was designed to collect information about the number of years with Type 2 Diabetes, number of years in pharmacological treatment, and family with Type 2 Diabetes.
Psychosocial characteristics
Anxiety and depression symptoms were assessed using the Hospital Anxiety and Depression Scale (HADS) (Pais-Ribeiro et al., 2007; Zigmond & Snaith, 1983), that consists of 14 items divided into two subscales of seven items. Each subscale ranges from 0-21, and a score between 0-7 points is within normal values. Values between 8-10 indicate possible anxiety / depression, and =11 suggests clinical anxiety / depression (Snaith & Zigmond, 1994).
Social support was evaluated with the Satisfaction with Social Support Scale (ESSS) (Pais-Ribeiro, 1999) and it consists of 15 items divided into four dimensions: satisfaction with friends, intimacy, satisfaction with family and social activities. Each item is scored from 1 (totally agree) to 5 (totally disagree). A global score can also be obtained (total ESSS), between 15-75 points, with high scores indicating higher levels of perceived social support, and scores =51 suggesting a good social support.
Sleep was assessed through the Pittsburgh Sleep Quality Index (PSQI) (Buysse, Reynolds, Monk, Berman, & Kupfer, 1986) and measured both its qualitative and quantitative aspects in the last month, and comprises seven dimensions: overall sleep quality, sleep latency, duration of sleep, sleep efficiency, sleep disturbance, need meds to sleep, day dysfunction due to sleepiness, and a total score. Each dimension is scored from 0-3 and the total score varies from 0-21, with 21 being the worse quality of sleep possible. Scores >5 suggest a poor sleep quality and >10 determine the presence of a sleep disorder (Buysse, Reynolds, Monk, Berman, & Kupfer, 1989).
The original and Portuguese version of the instruments had adequate psychometric properties: HADS (Pais-Ribeiro et al., 2007; Zigmond & Snaith, 1983); ESSS (Pais-Ribeiro, 1999); PSQI (Bertolazi et al., 2011; Buysse et al., 1986).
Procedures
The assessment was performed in a single moment. The subjects of the sample fulfilled the evaluation protocol that was composed by the researcher-design form regarding the socio demographic and clinical variables and the HADS, the ESSS and the PSQI.
Statistical analysis
The presentation of socio demographic, clinical and psychosocial variables was based on observed frequencies and percentages in the case of categorized / ordinal variables, and the mean and standard deviation in the case of quantitative variables. The internal consistency was assessed using the Cronbachs Alpha, considering acceptable values =0.70 (Nunnally & Bernstein, 1994). The bivariate relationships between socio demographic, clinical and psychosocial variables were calculated by the U Mann-Whintey, the Chi-Square test and the r Spearman.
The statistical significance level was p<0.05, and the statistical analysis was made using the SPSS version 17.0 for Windows.
RESULTS
The sample studied was formed by 90 patients with Type 2 Diabetes, with a mean age of 56.67 years (SD=6.41), and 50% were women. The sample majority was married / common law marriage (86.70%), had studies =1st degree (74.40%), and living with restricted family (65.60%). When it comes to the employment status a homogeneous distribution was observed between employed (40%), unemployed (25.60%) and retired patients (34.40%).
Data regarding clinical variables, revealed that the sample presented a mean of 8.96 years with Type 2 Diabetes (SD=6.44; range between 2-32 years), a mean of 8.36 years on pharmacological treatment (SD=5.54; range between 1-32 years), and the majority of sample patients had relatives with Type 2 Diabetes (68.90%).
When considering the psychosocial variables, it should be mentioned that the HADS depression (a=0.632), the ESSS intimacy (a=0.568) and the total PSQI (a=0.555) revealed scores of internal consistency <0.70. It should be stressed that the sample presented low levels of anxiety and depression symptoms (scores <8 points), with the HADS anxiety revealing mean scores of 7.27 (SD=5.07) and the HADS depression reporting mean scores of 3.77 (SD=2.98). Considering that the HADS score was above 8 points, suggests the presence of anxiety / depression symptoms. It was verified that 35.60% of the sample (n=32) revealed anxiety symptoms and 6.70% presented depression symptoms (n=6). For social support, it was observed scores of 66.87 in the total ESSS (SD=8.22) and scores =3.97 in its sub scales. For sleep quality, the total PSQI score was 8.68 (SD=2.87), 73.30% (n=66) had poor sleep quality (total PSQI scores between 5-10), and 24.40% (n=22) revealed sleep disorder (total PSQI score >10).
The results show, by assessing males, that the sample had a mean age of 56.75 years (SD=6.58), mostly married (n=40), with low educational levels (34 with studies =1st degree). The majority were employed (n=23), living in restricted families (n=28), and had relatives with Type 2 Diabetes (n=30). As to the female patients, they had a mean age of 56.57 years (SD=6.30), were mostly married (n=38), with low study levels (33 with studies =1st degree), living in restricted families (n=31), and they had relatives with Type 2 Diabetes (n=32). However, as far as professional status is concerned, women presented a homogeneous distribution (Table 1).
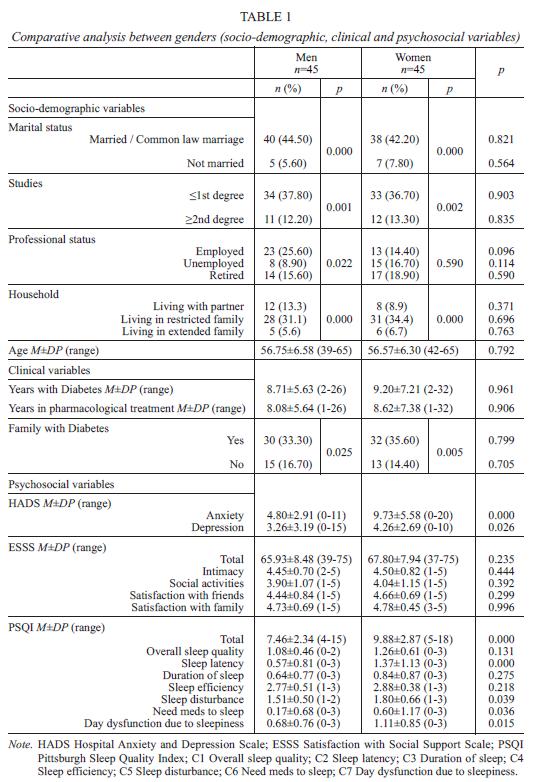
When gender-related outcomes were compared, significant statistical differences werent found regarding the clinical variables and the psychosocial variables such as social support, overall sleep quality, duration of sleep, and sleep efficiency (PSQI). Nevertheless, women revealed higher depression symptoms scores (M=9.73; p=0.000), in anxiety symptoms (M=4.26; p=0.026) and in the PSQI scores as follows: total PSQI (M=9.88; p=0.000); sleep latency (M=1.37; p=0.000); sleep disturbance (M=1.80; p=0.039); need meds to sleep (M=0.60; p=0.036); and day dysfunction due to sleepiness (M=1.11; p=0.015) (Table 1).
By proceeding to the analysis of the relationship between the anxiety and depression symptoms, with the socio-demographic and clinical variables, it was only observed that unemployed patients presented significantly higher levels of depression symptoms when compared with employed ones (5.03±3.42 vs. 2.92±2.66; p<0.050).
By examining the relationship between the social support indicators and the socio-demographic and clinical variables, the employed patients presented significantly lower scores than unemployed patients in the total ESSS (p<0.050). The patients with family with Type 2 Diabetes revealed lower scores in the ESSS intimacy (p<0.050). The patients living with partners presented higher satisfaction with social activities than patients living with restricted families (p<0.050). Employed patients had lower satisfaction with family than unemployed and retired patients (p<0.050) (Table 2).
As to the relationship between the PSQI and the studied variables, the employed subjects revealed a better quality of sleep than unemployed subjects in the dimensions as follow: total PSQI (M=7.50 vs. M=10.30; p<0.050); overall sleep quality (M=0.97 vs. M=1.39; p<0.050); sleep latency (M=0.58 vs. M=1.48; p<0.050); day dysfunction due to sleepiness (M=0.72 vs. M=1.26; p<0.050). The employed patients also presented better quality of sleep scores when compared with retired patients in the dimensions: overall sleep quality (M=0.97 vs. M=1.26; p<0.050); need meds to sleep (M=0.11 vs. M=0.74; p<0.050). Retired patients presented a better sleep efficiency than employed (M=2.55 vs. M=2.97; p<0.050) and unemployed patients (M=2.55 vs. M=3.00; p<0.050). For the relationship between sleep quality and the household, it was only observed that subjects living with partners had a better sleep efficiency than subjects living in restricted families (M=2.60 vs. M=2.92; p<0.050) (Table 3).
When the correlation analysis between variables was made (Spearman R), the results revealed that the anxiety symptoms were positively correlated with depression symptoms (r=0.411; p<0.010) and all sleep quality indicators, with the exception of need meds to sleep. As far as depression symptoms is concerned, besides positively correlating with anxiety symptoms, as it was mentioned before, it was also positively correlated with all sleep quality indicators, except that of duration and efficiency of sleep. A positive correlation between depression symptoms and the age of patients was also observed (r=0.254; p<0.050), and a negative correlation with satisfaction with friends (r=-0.240; p<0.050). Besides being correlated with depression symptoms, social support presented positive correlations between the satisfaction with family and the overall sleep quality (r=0.384; p<0.010) and with age (r=0.232; p<0.050). As to sleep quality, negative correlations were observed between the efficiency of sleep and the variables as follows: number of years with Type 2 Diabetes (r=-0.213); number of years on pharmacological treatment (r=-0.228); and the patients age (r=-0.244) for a p<0.050. Sleep disturbance revealed positive correlations with the number of years on pharmacological treatment (r=0.218; p<0.050). Positive correlations between a high number of PSQI indicators was also noted (Table 4). To conclude, the number of years with Type 2 Diabetes was positively correlated with the number of years in pharmacological treatment (r=0.938; p<0.010) and with patients age (r=0.261; p<0.050), and the number of years in pharmacological treatment was positively correlated with the age of the subjects from the sample (r=0.293; p<0.010) (Table 4).
DISCUSSION
Global sample results revealed a higher prevalence of anxiety than depression symptoms (36.60% vs. 6.70%) and the anxiety symptoms were related to a worse sleep quality with the exception of need meds to sleep. For its part the depression symptoms were associated with low satisfaction with friends, with a worse sleep quality, and affected more retired and unemployed patients. Both anxiety and depression symptoms, and sleep quality aspects, affected significantly more women than men.
Our findings presented a high prevalence of patients with family with Type 2 Diabetes (68.90%). In fact, the high prevalence of Type 2 Diabetes within family could be explained by the sharing of the same genetic predispositions and similar lifestyle habits as their relatives (Kuzuya & Matsuda, 1982), with some studies suggesting that individuals with an affected first-degree relative have a 2.3 to 5.5 fold higher risk of developing Type 2 Diabetes, independent of gender, age, race, body mass index (BMI) and other demographic variables (Valdez, Yoon, Liu, & Khoury, 2007). Unlike Gucciardi et al. (2008), that suggests that women have a higher prevalence of relatives with a history of Type 2 Diabetes, our data did not found differences between genders.
Our results also contradict the literature, revealing low depression symptoms scores (3.77±2.98), and taking into consideration the normative data, the scores were within normal values (Zigmond & Snaith, 1983). As it can be observed, 6.70% of the sample presented depression symptoms (HADS depression scores =8), parameters close to 9.20% reported by Amorim and Coelho (2008) and in contrast with the studies that presented rates between 43.50 and 68.12% (Khuwaja, Lalani, et al., 2010; Ramos & Ferreira, 2011; Ricco et al., 2004; Roupa et al., 2009). The anxiety symptoms scores were higher than the depression symptoms scores (7.27±5.07 vs. 3.77±2.98), but still, as it happens with the depression symptoms, the scores are within normal values (HADS scores <8). Nonetheless, it should be stated that 36.6% of the sample presented anxiety symptoms (HADS scores =8). Our findings are consistent with the literature that points to a high prevalence of anxiety symptoms in patients with Type 2 Diabetes, with rates around 57.9% (Khuwaja, Lalani, et al., 2010).
Nevertheless, when comparative parameters between genders are established, women revealed significantly higher scores of depression (♀=4.26 vs. ♂=3.26; p=0.026) and anxiety symptoms (♀=9.73 vs. ♂=4.80; p=0.000). These gender differences, which support a higher prevalence of depression symptoms in women with Type 2 Diabetes, have been mentioned in previous studies that pointed out rates twice as high when compared with men (Amorim & Coelho, 2008; Gucciardi et al., 2008; Khuwaja, Lalani, et al., 2010; Roupa et al., 2009). It is that known that women are significantly associated with depression in the general populations (Khuwaja & Kadir, 2010) and among people with Diabetes (Collins, Corcoran, & Perry, 2009). A possible explanation is that women play gender specific roles, which exposes them to increased work demands and responsibilities, and the social rule attributed to women allows them to be more emotional and extroversive (Khuwaja, Lalani, et al., 2010). As mentioned before, women also scored higher than men on anxiety symptoms, revealing the presence of anxiety which is consistent with the study of Amorim and Coelho (2008). In this context, it should be mentioned Roupa et al. (2009) that assessed 310 patients with Type 2 Diabetes (56% women) and women presented anxiety symptoms scores 3 times higher than men, with HADS scores =8 in about 62% female patients. On the other hand, men had HADS scores =8 in only 21% of cases (p<0.001).
When it comes to the relationship between the depression symptoms and the socio demographic variables, it was only found that employed patients presented significant lower depression scores (2.92±2.66) than retired ones (5.03±3.42). Amorim and Coelho (2008) had similar results by assessing a sample of 304 patients with Type 2 Diabetes (186 women) with a mean age of 59.25 years (SD=8.56). Mostly were married and retired and with low study levels. In this study, active patients revealed significant lower scores in depression symptoms assessed through the HADS (p<0.001), which suggests work as a protective factor of the mental area.
Relating to the association between depression symptoms and the psychosocial variables, data pointed to an association between higher levels of depression symptoms, a lower satisfaction with friends (r=-0.240; p<0.050), a worse sleep quality assessed through the total PSQI (r=0.404; p<0.001), a worse overall sleep quality (r=0.263; p<0.050), a worse sleep latency (r=0.300; p<0.001), higher levels of sleep disturbance (r=0.327; p<0.001), and higher levels of day dysfunction due to sleepiness (r=0.266; p<0.001). Positive correlations were also observed between the depression symptoms scores and patients age (r=0.254; p<0.050), suggesting higher levels of depression in elderly patients, which is in line with Tellez-Zenteno and Cardiel (2002), and represents a negative interference of depression in the psychological functioning of patients with Type 2 Diabetes .
The social support results, in the present sample, revealed normal scores pointing to satisfactory outcomes in all the ESSS domains. In a maximum score of 75 points, our sample presented mean scores of 66.87 (DP=8.22) suggesting high levels of social support satisfaction. One possible explanation for these findings are the socio-demographic characteristics of the sample, as 78% of patients were married and 70 % were living with restricted / extended family, which indicates an extended family support. There were no differences between genders on social support, even though some studies suggesting better social support by formal caregivers in women with Type 2 Diabetes (Gucciardi et al., 2008). However, employed patients revealed a worse total social support and a lower family satisfaction than unemployed patients with Type 2 Diabetes (p<0.050). In the case of satisfaction with family, it was also observed that employed patients revealed less satisfaction than retired ones (p<0.05), and as patients get older, they perceive higher levels of satisfaction with family (r=0.232; p<0.050). These findings seem to suggest that being employed contributes to a worse social support perception, which can be better explained by the labor demands, limited family lifetime and therefore a smaller social network than unemployed and retired patients. It is also possible that as patients with Type 2 Diabetes get older, they come to recognize and appreciate family ties, hence the positive correlation between age and satisfaction with family assessed through the ESSS.
Almost all sleep quality indicators (with the exception of need meds to sleep) showed positive correlations with the anxiety symptoms. In the general adult population, the prevalence of sleep disorders are between 10-20% (Roth, 2008), and sleep disorders coexist with a number of physical and psychiatric conditions, including anxiety disorders (Walsh, 2004). Moreover, when examining the sleeping patterns, 90 patients revealed disturbed sleep indices with mean scores above 5 (8.68±2.87), which suggests poor sleep quality and, near the limit of 10 points, suggests the presence of a sleep disorder (Buysse et al., 1989). Cunha, Zanetti and Hass (2008), in one of the scarce studies that assessed sleep in Type 2 Diabetes, analyzed 50 patients, 76% women, 52% married, with ages between 44-79 years, and through the PSQI concluded that the majority (52%) had a poor sleep quality (score =5). Likewise, Knutson et al. (2006) assessed 161 subjects and Vigg (2003) assessed 220 subjects, both with patients with Type 2 Diabetes, concluded that 71% presented a PSQI score =5, showing that Type 2 Diabetes is associated with sleeping problems (Barone & Menna-Barreto, 2011). Rajendran et al. (Rajendran, Parthsarathy, Tamilselvan, Seshadri, & Shuaib, 2012) evaluated 120 patients with Type 2 Diabetes (55 women), with a mean age of 53.9 years (SD=9.20) and concluded that the average length of Diabetes diagnosis (7.41±5.90) was positively correlated with the total PSQI score (r=0.181; p<0.050), suggesting that Diabetes duration has a strong influence on patients sleep (the data was independent of variables as age, gender, body mass index or meds). As in our study, the sample revealed a total PSQI score of 7.08 and 69% presented a total PSQI score =5. This data became even more troubling in unemployed patients with Type 2 Diabetes with average total PSQI scores of 10.30, versus the score of 7.50 in employed patients. The literature suggests that groups from low socio-economic status have less sleep duration and lower sleep quality (Gellis et al., 2005). Qualified employees have better sleep levels (Sekine et al., 2006), and unemployed men had a higher prevalence of sleep-related complaints (Grandner et al., 2010). The results from our study are partially in accordance with the literature. Our data supports a worse sleep quality in unemployed patients, no comparative analysis between genders was taken regarding the relationship between professional status and sleep. Nevertheless, in our study, the employed patients had better sleep patterns than the unemployed ones in the total PSQI, the overall sleep quality, sleep latency, and in day dysfunction due to sleepiness (p<0.050). The employed patients also presented a better overall sleep quality when compared to retired patients (p<0.050). For sleep efficiency, the retired patients revealed the best scores (p<0.050), with employed and unemployed patients presenting similar results. On the other hand, the retired patients presented a higher need for sleep medication than employed patients. It was also observed that women had worse sleep patterns in the total PSQI, sleep latency, sleep disturbance, need meds to sleep and day dysfunction due to sleepiness (p<0.039), which is in line with the results from the general female population (Collop, Adkins, & Phillips, 2004).
When analyzing the relationship between the PSQI and the ESSS, only positive correlations were observed between overall sleep quality and satisfaction with family (r=0.384; p<0.010). In other words, patients with worse overall sleep quality expressed a better family social support. However, as far as sleep efficiency is concerned, patients with more years with Diabetes (r=-0.231; p<0.050), with more years in pharmacological treatment (r=-0.228; p<0.050), and older patients (r=-0.244; p<0.050) revealed better results, which can suggest a positive adaptation process to Type 2 Diabetes and aging. When it comes to sleep disturbance, patients with more years in pharmacological treatment had worse scores (r=0.218; p<0.050).
The data observed in this study suggests that, when treating patients with Type 2 Diabetes, a broad assessment approach should be applied, taking into account factors such as professional status, gender, age, anxiety/depression symptoms, social support and sleep patterns perception. Identifying factors that determine the extent of the impact of Type 2 Diabetes will allow the detection of vulnerable groups/individuals and the design of more effective interventions.
However, this data presents some limitations. Firstly, future studies should include larger populations for a greater data generalization. Secondly, as coping strategies are important factors to understand how patients deal with disease and their health in general, these areas should be taken into account. Thirdly, theres an important association between obesity and Type 2 Diabetes. The relative risk of Type 2 Diabetes increases as BMI increases above 23, and association is stronger in young age groups (Colditz et al., 1990; Ni Mhurchu et al., 2006): the prevalence increases from 2% in those with BMI of 25 to 29,9kg/m2, to 8% in those with a BMI of 30 to 34,9 kg/m2, and to 13% in those with a BMI greater than 35 kg/m2 (Harris et al., 1998). Investigations focusing on weight change and Type 2 Diabetes showed that an increase in body weight of 3-20 kg was associated with an elevated risk of incident Type 2 Diabetes, and early obesity and almost any weight gain after adolescence were risk factors for Type 2 Diabetes (Schienkiewitz, Schulze, Hoffmann, Kroke, & Boeing, 2006). In fact, Type 2 Diabetes in children and adolescents is an important public health problem directly related to the epidemic of childhood obesity (Tfayli & Arslanian, 2009). Moreover, the duration of obesity seems to be a significant risk factor for Type 2 Diabetes, independently of current degree of obesity (Schienkiewitz et al., 2006). For these reasons, future studies should also include the BMI. Finally, it would be of interest to measure the impact of Type 2 Diabetes on patients health related quality of life.
In conclusion, we can state that anxiety symptoms are very prevalent in patients with Type 2 Diabetes and women are more vulnerable to anxiety, depression symptoms and poor sleep quality.
REFERENCES
Amorim, I. L., & Coelho, R. (2008). Diabetes Mellitus Tipo 2 e sintomas psicopatológicos. Psicologia, Saúde & Doenças, 9(2), 319-333. [ Links ]
Barone, M. T., & Menna-Barreto, L. (2011). Diabetes and sleep: A complex cause-and-effect relationship.Diabetes Res Clin Pract, 91(2), 129-137. doi: 10.1016/j.diabres.2010.07.011; S0168-8227(10)00388-8 [pii] [ Links ]
Bertolazi, A. N., Fagondes, S. C., Hoff, L. S., Dartora, E. G., Miozzo, I. C., de Barba, M. E., & Barreto, S. S. (2011). Validation of the Brazilian Portuguese version of the Pittsburgh Sleep Quality Index. Sleep Med, 12(1), 70-75. doi: 10.1016/j.sleep.2010.04.020; S1389-9457(10)00380-1 [pii] [ Links ]
Buysse, D. J., Reynolds, C. F., Monk, T. H., Berman, S. R., & Kupfer, D. J. (1986). The Pittsburgh Sleep Quality Index (PSQI): A new instrument for psychiatric research and practice. Psychiatry Research, 28(2), 193-213. [ Links ]
Buysse, D. J., Reynolds, C. F., Monk, T. H., Berman, S. R., & Kupfer, D. J. (1989). The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Res, 28(2), 193-213. [ Links ]
Colditz, G. A., Willett, W. C., Stampfer, M. J., Manson, J. E., Hennekens, C. H., Arky, R. A., & Speizer, F. E. (1990). Weight as a risk factor for clinical diabetes in women. Am J Epidemiol, 132(3), 501-513. [ Links ]
Collins, M. M., Corcoran, P., & Perry, I. J. (2009). Anxiety and depression symptoms in patients with diabetes. Diabet Med, 26(2), 153-161. doi: 10.1111/j.1464-5491.2008.02648.x; DME2648 [pii] [ Links ]
Collop, N. A., Adkins, D., & Phillips, B. A. (2004). Gender differences in sleep and sleep-disordered breathing. Clin Chest Med, 25(2), 257-268. doi: 10.1016/j.ccm.2004.01.002; S0272523104000164 [pii] [ Links ]
Cunha, M. C. B., Zanetti, M. L., & Hass, V. J. (2008). Sleep quality in type 2 diabetics. Revista Latino-Americana de Enfermagem, 16, 850-855. [ Links ]
Fagot-Campagna, A., Balkau, B., Simon, D., Warnet, J. M., Claude, J. R., Ducimetiere, P., & Eschwege, E. (1998). High free fatty acid concentration: An independent risk factor for hypertension in the Paris Prospective Study. Int J Epidemiol, 27(5), 808-813. [ Links ]
Gellis, L. A., Lichstein, K. L., Scarinci, I. C., Durence, H. H., Raylor, D. J., Bush, A. J., & Riedel, B. W. (2005). Socioeconomic status and insomnia. Journal of Abnormal Psychology, 114(2), 111-118. [ Links ]
Goldney, R. D., Phillips, P. J., Fisher, L. J., & Wilson, D. H. (2004). Diabetes, depression, and quality of life: A population study. Diabetes Care, 27(5), 1066-1070. [ Links ]
Grandner, M. A., Patel, N. P., Gehrman, P. R., Xie, D., Sha, D., Weaver, T., & Gooneratne, N. (2010). Who gets the best sleep? Ethnic and socioeconomic factors related to sleep complaints. Sleep Med, 11(5), 470-478. doi: 10.1016/j.sleep.2009.10.006; S1389-9457(10)00096-1 [pii] [ Links ]
Gucciardi, E., Wang, S. C., DeMelo, M., Amaral, L., & Stewart, D. E. (2008). Characteristics of men and women with diabetes: Observations during patients initial visit to a diabetes education centre. Can Fam Physician, 54(2), 219-227. [ Links ]
Harris, M. I., Flegal, K. M., Cowie, C. C., Eberhardt, M. S., Goldstein, D. E., Little, R. R., . . . Byrd-Holt, D. D. (1998). Prevalence of diabetes, impaired fasting glucose, and impaired glucose tolerance in U.S. adults. The Third National Health and Nutrition Examination Survey, 1988-1994. Diabetes Care, 21(4), 518-524. [ Links ]
Hussain, A., Hydrie, M. Z. I., Claussen, B., & Asghar, S. (2010). Type 2 Diabetes: A review article. Journal of Diabetology, 2(1), 1-7. [ Links ]
Jakab, Z. (2010). Delivering for Diabetes in Europe. Paper presented at the Plenary Meeting of the European Parliaments EU Diabetes Working Group, Brussels, Belgium. http://www.euro.who.int/data/assets/ pdf_file/0007/128059/RD_speech_Diabetes_Brussels_Dec_2010.pdf
Khuwaja, A. K., & Kadir, M. M. (2010). Gender differences and clustering pattern of behavioural risk factors for chronic non-communicable diseases: Community-based study from a developing country. Chronic Illn, 6(3), 163-170. doi: 10.1177/1742395309352255; 1742395309352255 [pii] [ Links ]
Khuwaja, A. K., Lalani, S., Dhanani, R., Azam, I. S., Rafique, G., & White, F. (2010). Anxiety and depression among outpatients with type 2 diabetes: A multi-centre study of prevalence and associated factors. Diabetol Metab Syndr, 2, 72. doi: 10.1186/1758-5996-2-72; 1758-5996-2-72 [pii] [ Links ]
Knutson, K. L., Ryden, A. M., Mander, B. A., & Van Cauter, E. (2006). Role of sleep duration and quality in the risk and severity of type 2 diabetes mellitus. Arch Intern Med, 166(16), 1768-1774. doi: 10.1001/archinte. 166.16.1768; 166/16/1768 [pii] [ Links ]
Kuzuya, T., & Matsuda, A. (1982). Family histories of diabetes among Japanese patients with type 1 (insulin-dependent) and type 2 (non-insulin-dependent) diabetes. Diabetologia, 22(5), 372-374. [ Links ]
Nascimento, A. B., Chaves, E. C., & Grossi, S. A. A. (2009). Depressão, cortisol urinário e perfil sócio-demográfico de portadores de Diabetes Mellitus Tipo 2. Revista da Escola de Enfermagem da USP, 43(2), 1272-1276. [ Links ]
Ni Mhurchu, C., Parag, V., Nakamura, M., Patel, A., Rodgers, A., & Lam, T. H. (2006). Body mass index and risk of diabetes mellitus in the Asia-Pacific region. Asia Pac J Clin Nutr, 15(2), 127-133. [ Links ]
Nunnally, J. C., & Bernstein, I. H. (1994). Psychometric theory (3rd ed.). New York: McGraw-Hill. [ Links ]
Observatório Nacional da Diabetes. (2010). Diabetes: factos e números 2010 – Relatório anual do observatório nacional da Diabetes. Lisboa: Ministério da Saúde de Portugal. [ Links ]
Osborn, C. Y., & Egede, L. E. (2012). The relationship between depressive symptoms and medication nonadherence in type 2 diabetes: The role of social support. Gen Hosp Psychiatry, 34(3), 249-253. doi: 10.1016/j. genhosppsych.2012.01.015; S0163-8343(12)00030-8 [pii] [ Links ]
Pais-Ribeiro, J. L. (1999). Escala de Satisfação com o Suporte Social (ESSS). Análise Psicológica, XVII(3), 547-558. [ Links ]
Pais-Ribeiro, J. L., Silva, I., Ferreira, T., Martins, A., Meneses, R., & Baltar, M. (2007). Validation study of a Portuguese version of the Hospital Anxiety and Depression Scale. Psychol Health Med, 12(2), 225-235. [ Links ]
Papelbaum, M., Appolinario, J. C., Moreira Rde, O., Ellinger, V. C., Kupfer, R., & Coutinho, W. F. (2005). Prevalence of eating disorders and psychiatric comorbidity in a clinical sample of type 2 diabetes mellitus patients. Rev Bras Psiquiatr, 27(2), 135-138. [ Links ]
Park, H., & Kim, M. T. (2012). Impact of social role strain, depression, social support and age on diabetes self-efficacy in Korean women with type 2 diabetes. J Cardiovasc Nurs, 27(1), 76-83. [ Links ] doi: 10.1097/JCN. 0b013e318214d9d9
Peyrot, M. (2003). Depression: A quiet killer by any name. Diabetes Care, 26(10), 2952-2953. [ Links ]
Peyrot, M., & Rubin, R. R. (1999). Persistence of depressive symptoms in diabetic adults. Diabetes Care, 22(3), 448-452. [ Links ]
Rajendran, A., Parthsarathy, S., Tamilselvan, B., Seshadri, K. G., & Shuaib, M. (2012). Prevalence and correlates of disordered sleep in southeast asian indians with type 2 diabetes. Diabetes Metab J, 36(1), 70-76. doi: 10.4093/dmj.2012.36.1.70 [ Links ]
Ramos, L., & Ferreira, E. A. P. (2011). Fatores emocionais, qualidade de vida e adesão ao tratamento em adultos com Diabetes Tipo 2. Revista Brasileira de Crescimento e Desenvolvimento Humano, 21(3), 867-877. [ Links ]
Ricco, R. C., Miyazaki, M. C. O. S., & Silva, R. C. M. A. (2004). Depressão em pacientes adultos portadores de doenças crónicas: Diabetes mellitus e hepatites virais. Arquivos de Ciências da Saúde, 7(9), 156-160. [ Links ]
Roth, T. (2008). Novel outcome measures of sleep, sleep loss and insomnia. Sleep Med, 9(Suppl. 1), S1-2. doi: 10.1016/S1389-9457(08)70009-1; S1389-9457(08)70009-1 [pii] [ Links ]
Roupa, Z., Koulouri, A., P, S., Makrinika, E., Marneras, X., Lahana, I., & Gourni, M. (2009). Anxiety and depression in patients with type 2 diabetes mellitus, depending on sex and body mass index. Health Science Journal, 3(1), 32-40. [ Links ]
Schienkiewitz, A., Schulze, M. B., Hoffmann, K., Kroke, A., & Boeing, H. (2006). Body mass index history and risk of type 2 diabetes: Results from the European Prospective Investigation into Cancer and Nutrition (EPIC) – Potsdam Study. The American Journal of Clinical Nutrition, 84(2), 427-433. [ Links ]
Schiotz, M. L., Bogelund, M., Almdal, T., Jensen, B. B., & Willaing, I. (2012). Social support and self-management behaviour among patients with Type 2 diabetes. Diabet Med, 29(5), 654-661. doi: 10.1111/j.1464-5491. 2011.03485.x [ Links ]
Sekine, M., Chandola, T., Martikainen, P., McGeoghegan, D., Marmot, M., & Kagamimori, S. (2006). Explaining social inequalities in health by sleep: The Japanese civil servants study. Journal of Public Health (Oxford), 28(1), 63-70. [ Links ]
Snaith, R. P., & Zigmond, A. S. (1994). HADS: Hospital Anxiety and Depression Scale. Windsor: NFER Nelson. [ Links ]
Tellez-Zenteno, J. F., & Cardiel, M. H. (2002). Risk factors associated with depression in patients with type 2 diabetes mellitus. Arch Med Res, 33(1), 53-60. [ Links ]
Tfayli, H., & Arslanian, S. (2009). Pathophysiology of type 2 diabetes mellitus in youth: The evolving chameleon. Arq Bras Endocrinol Metabol, 53(2), 165-174. doi: S0004-27302009000200008 [pii] [ Links ]
Valdez, R., Yoon, P. W., Liu, T., & Khoury, M. J. (2007). Family history and prevalence of diabetes in the U.S. population: The 6-year results from the National Health and Nutrition Examination Survey (1999-2004). Diabetes Care, 30(10), 2517-2522. doi: 10.2337/dc07-0720; dc07-0720 [pii] [ Links ]
Vigg, A. (2003). Sleep in Type 2 diabetes. J Assoc Physicians India, 51, 479-481. [ Links ]
Walsh, J. K. (2004). Clinical and socioeconomic correlates of insomnia. Journal of Clinical Psychiatry, 659(Suppl. 8), 13-19. [ Links ]
Zigmond, A. S., & Snaith, R. P. (1983). The hospital anxiety and depression scale. Acta Psychiatr Scand, 67(6), 361-370. [ Links ]
Zimmernan, B. R., & Walker, E. A. (2002). Guia completo sobre Diabetes. Rio de Janeiro: Anima Editora. [ Links ]
Submissão: 09/07/2013 Aceitação: 22/10/2013
A correspondência relativa a este artigo deverá ser enviada para: Elisabete Gomes Costa, Universidade Católica Portuguesa, Praça da Faculdade de Filosofia, 4710-297 Braga. E-mail: famgomescosta@sapo.pt














