Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Finisterra - Revista Portuguesa de Geografia
versão impressa ISSN 0430-5027
Finisterra no.109 Lisboa dez. 2018
https://doi.org/10.18055/Finis14118
ARTIGO ORIGINAL
Differential mortality and inequalities in health services access in mainland Portugal
Mortalidade diferencial e desigualdades no acesso aos serviços de saúde em Portugal Continental
Mortalité différentielle et inégalités a l'accès aux services de sante Portugal péninsulaire
Diogo Guedes Vidal1; Manuela Pontes2; Esmeralda Barreira3; Gisela M. Oliveira4; Rui Leandro Maia5
1 PhD Student and Researcher, Fernando Pessoa Energy, Environment and Health Research Unit., University Fernando Pessoa. Porto, Portugal. E-mail: diogovidal@ufp.edu.pt
2 Assistant Professor, Researcher, Fernando Pessoa Energy, Environment and Health Research Unit., Faculty of Health Sciences, University Fernando Pessoa. Porto, Portugal. E-mail: mpontes@ufp.edu.pt
3 Assistant Professor, Researcher, Instituto Português de Oncologia, E.P.E. – Clínica do Pulmão, Porto, Portugal; Fernando Pessoa Energy, Environment and Health Research Unit., Faculty of Health Sciences, University Fernando Pessoa. Porto, Portugal. E-mail: merb@ufp.edu.pt
4 PhD, Researcher, Fernando Pessoa Energy, Environment and Health Research Unit. University Fernando Pessoa. Porto, Portugal. E-mail: gisela@ufp.edu.pt
5 Associate Professor, Researcher, Fernando Pessoa Energy, Environment and Health Research Unit., Faculty of Human and Social Sciences, University Fernando Pessoa, CITCEM – Centro de Investigação Transdisciplinar Cultura, Espaço e Memória, Praça 9 de abril, 349, 4249-004, Porto, Portugal. E-mail: rlmaia@ufp.edu.pt
ABSTRACT
The guarantee of the right to health protection, with the priority of overcoming health inequalities, is a main goal of the Portuguese National Health Service. In this context, health care access equity in mainland Portugal continues to be a challenge for public health policies, with a littoral territory where health services are concentrated and interior depopulated zones, stripped of health services and isolated in physical and social terms. Based on 2011 data from PORDATA , the present article studies how mortality is related to the distribution of health services - namely hospital infrastructures, health centres and health professionals - and with population characteristics related to illiteracy and ageing. The results show a strong association between mortality and the distribution of health services, highlighting increasing mortality in the context of decreasing health services, worsening when related to population illiteracy and ageing. Results reveal the importance of designing public policies at the local level, focused on territorial socio-cultural specificities, which are mainly materialized in a distribution of health services closer to isolated populations according to their needs.
Keywords: Differential mortality; national health service; equity; inequalities; territory.
RESUMO
O Serviço Nacional de Saúde português tem como objetivo principal assegurar o direito à proteção da saúde, tendo como prioridade a supressão das desigualdades em saúde. Neste sentido, a equidade no acesso aos cuidados de saúde em Portugal continental continua a ser um desafio para as políticas públicas em saúde, sendo visível um território litoral onde os serviços se encontram concentrados e um interior despovoado, despojado de serviços de saúde e condenado a um isolamento físico e social. Tendo por base dados relativos a 2011 obtidos do PORDATA este trabalho debruça-se sobre a forma como a mortalidade se encontra relacionada com a distribuição dos serviços de saúde – infraestruturas hospitalares, centros de saúde e profissionais de saúde – bem como com características da população relacionadas com a iliteracia e o envelhecimento. Os resultados alcançados demonstram uma relação de associação forte entre a mortalidade e a distribuição dos serviços de saúde, evidenciando que à medida que estes diminuem aumenta a mortalidade, ocorrendo um agravamento da vulnerabilidade à morte quando se relaciona com a iliteracia e o envelhecimento da população. Os resultados alcançados revelam a importância do desenho de políticas públicas à escala local, focadas nas especificidades socioculturais dos territórios e que se materializem, sobretudo, numa distribuição de serviços de saúde mais próximos das populações isoladas de acordo com as suas necessidades.
Palavras-chave: Mortalidade diferencial; serviço nacional de saúde; equidade; desigualdades; território.
RÉSUMÉ
Le Service National de Santé portugais doit avant tout garantir le droit à la protection de la santé, en supprimant les inégalités d'accès aux soins. Ceci constitue encore un défi pour les responsables. Les services sont en effet concentrés sur le Littoral, alors que l'intérieur dépeuplé en est dépourvu et est condamné à un isolement tant physique que social. À partir des données de PORDATA pour 2011, on a cherché à comprendre les rapports existants entre la mortalité et la répartition, tant des services de santé (infrastructures hospitalières, centres de santé, professionnels de santé), que des caractéristiques de la population (analphabétisme et vieillissement). Cela montre l'importance que les politiques publiques ont au niveau local, selon les spécificités socio-culturelles de celles-ci, surtout matérialisées par la répartition des services de santé et des besoins des populations les plus isolées.
Mots clés: Mortalité différentielle; service national de santé; équité; inégalités; territoire.
I. INTRODUCTION
Adequate health care services should be present in every society. It may be assumed as the main tool to minimize amenable mortality due to their capability to prevent, diagnose and apply treatment measures in a universal way. Health systems have three fundamental goals: improving health, providing services responding to the populations needs and establishing systems of fair financing (WHO, 2000). The adequate access to health care services by everyone, independently of their socioeconomic conditions is one of the implementation pillars of a National Health Service and “(…)exists when patients can get the right service at the right time in the right place” (Champman, Zechel, Carter, & Abbott, 2004, p. 374). Equity in health is a concept primarily defined by Margaret Whitehead in 1992 and suggests that although health differences are unnecessary and avoidable, they are also unfair and unjust (Whitehead, 1992). Whitehead (1992) explains the multiple dimension of this concept and refers to the fact that equity in health requires that everyone should have a fair opportunity to attain their full health care potential. The same author (1992) goes further and brings to the discussion equity in health care access related to the fact that everyone should have “equal access to available care for equal need, equal utilization for equal need, and equal quality of care for all” (Whitehead, 1992, p. 434).
In the present article, the concept under discussion is inequity in health care access that is visible when resources, like health facilities and health professionals, are unevenly distributed around the country with health services “clustered” in urban areas to the detriment of rural areas (Whitehead, 1992; Gulliford, 2002). Related with this concept is the “Inverse Care Law” theory, initially developed by Julian Tudor Hart (1971) and discussed by some authors (Hart, 2000; Furler et al., 2002; Watt, 2002; Dalrymple, 2012; Nambiar & Mander, 2017). The Inverse Care Law is based on the principle that “the availability of good medical care tends to vary inversely with the need for it in the population served” (Hart, 1971, p. 1). Moreover, those who require health care the most, like the elderly, are those who receive it last due to the absence of health services or to the physical distance to them. This theory is in accordance with past research that shows Portugal’s asymmetries’ (Santana & Freitas, 2015; Santana & Teixeira, 2017).
Inequalities in health are directly associated with the way that society is organized and, naturally, have repercussions in the uneven possibility of the freedom to “(…)lead a ?ourishing life and to enjoy good health(...)” (WHO, 2008, p. 3). Spatial and social disparities between groups continue to have a relevant influence in health inequalities. Evaluation of the populations’ health is assumed as an important issue to help decision makers in the design of public health policies. This kind of study aims to identify the main concerns and strategies to overcome the identified problems. Access to health care, based on an equity principle, is a universal right and equity in health services access defends that the specificities of each region, related to the health needs of the population, should correspond to health services available (Entidade Reguladora da Saúde, 2009; Direção-Geral da Saúde, 2015) and implies the allocation of fair shares (McCoy, 2003). According to the Graduate Medical Education National Advisory Committee study, distance to health centres should not be greater than 30 minutes (Remoaldo, 2003; Entidade Reguladora da Saúde, 2009; Direção-Geral da Saúde, 2012).
According to the World Health Organization (WHO) (2018), the health workforce is related with four dimensions: the availability of health professionals with competencies and skills to match population needs; the accessibility, as mentioned previously, the equitable distribution of health professionals and infrastructures’ taking into account the demographic composition; the equal treatment of all patients; and quality of health services.
One of the main objectives of this work is to discuss results and data of the current health care services in mainland Portugal aiming to contribute to the analysis of the organization of the health system.
II. HEALTH CARE ACCESS AND MORTALITY: EUROPEAN TRENDS
In the field of health care, European countries pursue the goal to reduce inequalities in access to health care systems (Mackenbach et al., 2017), mainly fighting against amenable mortality, defined as premature death, from multiple conditions, that should not occur in the presence of timely and effective health care (Rutstein et al., 1976; Charlton, Hartley, & Holland, 1983; Gianino, Lenzi, Fantini, Ricciardi, & Damiani, 2017). This indicator (amenable mortality) is of the utmost importance for the evaluation of quality, effectiveness and preventive actions of health services. Additionally, this measure allows the combination of multiple indicators beyond classic ones: mortality, life expectancy or potential years of life lost.
Although understood as a transversal phenomenon, health inequalities have multiple impacts on people’s lives, limiting their possibilities to act as an individual in society. Besides the progress on the amenable mortality decline proved by several studies (Nolte & Mckee, 2008; Gay, Paris, Devaux, & De Looper, 2011; Nolte & Mckee, 2012) presently, there are still profound differences between socioeconomic groups, which are translated into higher vulnerability to death. As known, recent economic difficulties in European countries had a huge negative impact on health services, namely in national health systems, related to funding constraints (Gianino, Lenzi, Fantini, Ricciardi, & Damiani, 2017; Watkins et al., 2017). These constraints did not affect populations equally mainly due to intrinsic factors related to:1) the likelihood of individuals to develop a disease, 2) early diagnosis, 3) education level, 4) social class, 5) self-perceived health and concern, 6) costs of diagnosis and treatment (Nolte & Mckee, 2004).
In the EU, in 2014, more than 562 000 deaths (considered amenable deaths ) were related with causes that could have potentially been avoided if proper health care services had offered timely and effective medical treatments (Eurostat, 2017). A deeper analysis shows that almost one million deaths could have been prevented if adequate public health care had been applied according to the characteristics of the population. Together, amenable and preventable deaths reached nearly 1.2 million in 2014 (Eurostat, 2017). A study developed in seventeen European countries, from 1980-2010, found a dramatic decline over time of death potentially avoidable in women and men in all education groups. In both sexes, more education translates into less vulnerability to amenable death, however, men are more vulnerable to this cause of death (Mackenbach et al., 2017).
Another relevant study defines the “Healthcare Access and Quality (HAQ) Index” over the period between 1990-2015. For the analysed period, some countries were able to improve health care access and quality (such as Australia and European countries, including Portugal), while others remain stagnant (GBD 2015 Healthcare Access and Quality Collaborators, 2015). This study also highlights that the geographical distribution of diseases is unequal and relates to countries’ development levels: 1) countries’ populations with the highest socio-demographic index showed more tendency to acquire diseases such as cancers; 2) chronic kidney disease, diabetes, diarrhoeal diseases, and lower respiratory infections are more common in countries with a middle socio-demographic index; 3) measles and tetanus are more common among countries with a lower socio-demographic index (GBD 2015 Healthcare Access and Quality Collaborators, 2015).
III. SOCIAL INEQUALITIES IN PORTUGAL: ACCESS TO THE NATIONAL HEALTH SERVICE
The Portuguese National Health Service (NHS) was created in 1979 by Law n. 56/79, 15th September, with the mission to provide access to all citizens, independent of their social and economic conditions, as well as to foreign – in a reciprocal basis –, stateless and political refugees. The system includes the management of integrated health care services, health promotion, disease prevention, diagnostic and treatment means for patients and their social and clinical rehabilitation. The Portuguese Health System Observatory (OPSS, 2003) and several studies on the evolution of the Portuguese NHS allow for an abridged chronology (Carapinheiro & Pinto, 1986; Campos, 2011; Silva, 2012): 1) 1970 to 1982 was the beginning of the NHS with its creation and expansion. In this period, the introduction of primary health care services, namely health centres, meant a huge advance in health promotion contributing to a more fair and inclusive system comprising the protection of all citizens; 2) 1982 to 1995 was characterized by changing the limits between public and private services system. Due to the integration in the Economic European Commission (UE), Portugal benefitted from many European financing programmes that allowed significant improvements of the NHS: better salary conditions to health professionals, creation of health regional administrations and private health sector stimulation; 3) From 1995 to 2002 an improvement of the public offer occurred, while the private offer remained stagnant; 4) The establishment of a mixed system between public and private services happened from 2002 to 2005, with the change of the original name from National Health System to National Health Service (although the first experience of public-private managing partnership in a public hospital in Portugal was in 1995, in the hospital Fernando de Fonseca (Amadora-Sintra); 5) From 2005 to 2009, public policies to expand and modernize the health services with efficiency was applied; 6) Since 2010, the NHS suffered many cuts derived from the economic crisis, which resulted in several austerity measures.
Throughout its 38 years of activity, the NHS has contributed to the improvement of services and health professionals’ quality. Despite this fact, Portugal continues to have a mismatch between offered services and populations needs (European Commission, 2015). In Portugal, the NHS covers all residents regardless of their legal status. However, administrative procedures and the necessity to pay most of the services are barriers to health care access (OECD/European Observatory on Health Systems and Policies, 2017). The NHS foundation was based upon the concept of the universal and general right to health protection independently of the economic and social conditions of citizens (Assembleia da República, 2005). At present, the NHS seems to be experiencing a recovery phase, but its fragility is visible through the analysis of the availability of services specially related to the lack of health professionals and infrastructures serving populations that are not living in urban areas.
IV. MATERIAL AND METHODS
The present article is a cross-sectional study based on statistics data from the PORDATA database referring to the years 2001 and 2011 (census). In 2011, the total population was registered as 10 557 560 (PORDATA, 2018a). This study’s target area includes the municipalities (N=278) of mainland Portugal (89 102km²), a south-eastern European country, located on the Iberian Peninsula. The Portuguese archipelagos of Madeira and Açores were excluded from the present study due to scarcity of available statistical data for the selected variables.
Studied variables are of qualitative and quantitative type. Qualitative variables refer to three territory typologies (fig. 1): littoral, which considered the municipalities by the sea (N=53); interior, which refers to municipalities that do not have frontiers with the ocean (N=169); and extreme interior refers to municipalities at the Portugal-Spain border and distant from the coastline (N=56).
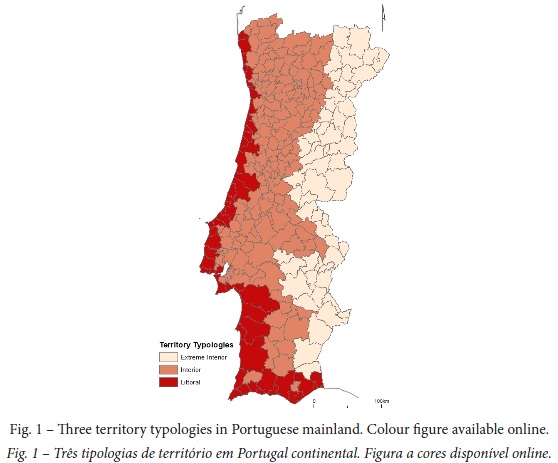
These three territory typologies were chosen to test the association with death vulnerability, expressed as gross death rate (number of deaths per resident population (×1000), in each year ). The reason behind the choice of this variable is related to the fact that urban and littoral territories offer more job opportunities and easier access to education, services and health (Maia, 2001; Maia, 2014). On the other hand, rural populations still face social barriers – especially the elderly – related to poor health services (lack of infrastructures and human resources), distance to education, culture, health services and vulnerable work conditions. People living far away from urban centres, in remote and rural areas with limited infrastructures, have less access to better health services and also to qualified health professionals (in this case it could be interesting to take into account, in future studies, the role of medical specialities in appropriate and effective health care treatments applied in urgent situations) like medical doctors and nurses (International Council of Nurses, 2011). Along with this reality, poverty and reduced physical mobility worsens with ageing enhancing unequal situations in these territories (Fundação Calouste Gulbenkian, 2014).
Independent quantitative variables are divided according to two groups. The 1st one is related to health infrastructures and human resources, specifically: health centres density by 100km2, hospitals density by 100km2, medical doctors and nurses working at health centres and medical doctors and nurses working at hospitals. Taking into account the study’s main objective to identify the NHS conditions related to accessibility, the first group of quantitative variables only considered public health (or NHS) infrastructures, thus private health services are not considered. The second group of quantitative variables relate to population characteristics: illiteracy rate (resident population with 10 years or older who cannot read or write per resident population with 10 years or older (× 1 000), in each year ) and ageing index (population with 65 years or older per population with less than 15 years (× 1 000), in each year ). In this case, it is important to continue studying the relation between these rates and mortality due to the fact that there are still inequalities in health services regarding life expectancy, thus revealing that people who live in less populated regions have lower life expectancy than urban / littoral populations (WHO, 2010). In Portugal, regions with higher vulnerability to death are those located in Centro and in Alentejo, which are sparsely populated, rural and interior regions. This is in accordance with reduced health care access and higher vulnerability to preventable death (Freitas & Costa, 2015).
Poverty puts in evidence socioeconomic inequalities in health in both rural and urbanpopulations, namely those who live in deprived areas in marginalized neighbourhoods (Santana, 2017). The gap in education is known as a factor that contributes to a poorer health condition. There is an association between better work opportunities and better health conditions, which is related to individuals’ quality of life, namely those who have balanced diets, physical activity practice, economic possibilities to go on vacations and faster access to better treatments (Alves, Correia, Barros, & Azevedo, 2012; Bastos et al., 2013). A study relates jobs types (of physical or intellectual kind) to populations’ level of education and to the occurrence of chronic back pain disease (Azevedo, Costa-Pereira, Mendonça, Dias, & Castro-Lopes, 2012). ArcMap 10.5 was applied to represent the spatial distribution of health services – number of health centres and hospitals – and data was normalized by 100km2. This option allows the understanding of which populations are most deprived of health services and, naturally, more distant from then.
Statistical analyses were performed with IBM® SPSS® Statistics vs.24.0 software and, in all comparative analyses, a confidence level of 95% or 99% (a = 0.05; a = 0.01) was used. Data distribution was analysed by the Kolmogorov-Simirnov test but normality in data distribution was not verified. Nevertheless, parametric tests were still applied because the condition N > 30 was verified in all of the three groups of variables. Health centres density by 100km2, hospital density by 100km2 and gross death rate comparison by territory typology was conducted by one-way ANOVA of multiple comparisons with the Tukey test ( a posteriori). The Spearman correlation test was applied to verify the statistic dependence between two variables. The Paired Samples Test was performed to verify the existence of mean differences between 2001 and 2011 for health centres and hospitals density by 100km2, medical doctors and nurses working at health centres, medical doctors and nurses working at hospitals, and gross death rate.
V. INEQUALITIES IN HEALTH SERVICES ACCESS AND RELATION WITH VULNERABILITY TO death - RESULTS
Although Portugal is a small country, profound differences based on territorial characteristics, in the dichotomy littoral / interior territories, were found.
Figure 2 represents the distribution of Portuguese health centres in 2001 and 2011 in mainland territory.
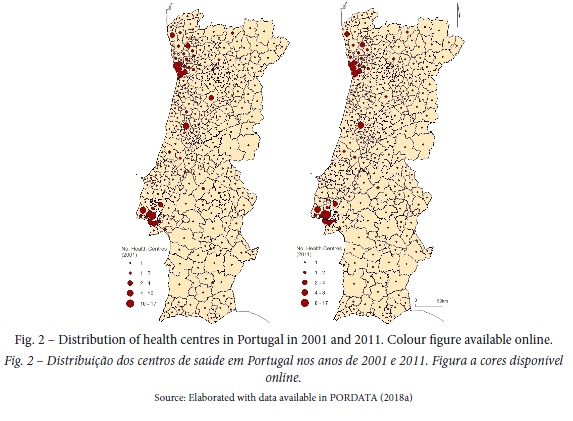
Figure 2 shows that the asymmetries of health services distribution are clear, namely the number of health centres available, and suggests that urban areas, mostly located in metropolitan areas, such as Porto and Lisboa, are those with more services which could result in better health care access (Simões et al., 2007). Another important issue to emphasize is that in the period analysed health services distribution did not benefit improvements, especially in regions where only one health centre exists for each municipality.
Figure 3 represents health centres and hospital density by 100km2 in 2011, exhibiting a visible asymmetry of health services distribution.
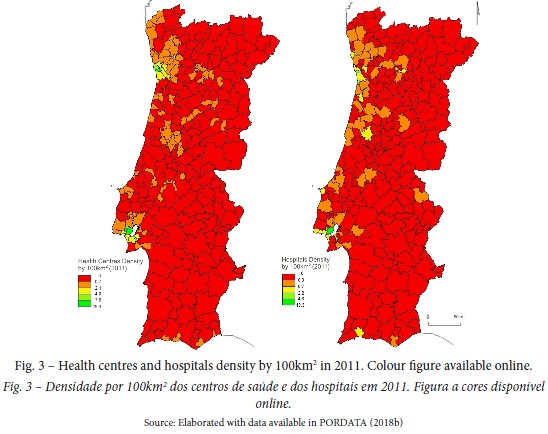
Maps show the mismatch between the availability of health services and population in a territory, a condition that is linked to higher vulnerability of death by preventable causes. In 2011, the municipalities with higher health centres density per 100km2 were Porto (19), Lisboa (16), Amadora (12), S. João da Madeira (12) and Odivelas (7). The municipalities with lower health centres density per 100km2 were Évora (0.07), Idanha-a-Nova (0.07), Castelo Branco (0.06), Alcácer do Sal (0.06) and Odemira (0.05). All the municipalities with higher health centres density are part of Porto and Lisboa metropolitan areas. On the other hand, municipalities with lower health centres density are all located in interior and extreme interior regions at the centre - south mainland. These results underline the polarization of health services and the uneven distribution of health services. Hospitals’ distribution is similar to health centres’ distribution but, generally, the existence of these infrastructures is reduced. According to figure 2, only municipalities that are assumed as urban areas have hospitals. Only some municipalities of the Porto and Lisboa metropolitan areas and also Algarve have more than 1 hospital per 100km2. The asymmetric distribution is visible when comparing regions that have 19 hospitals per 100km2 – municipalities of Porto and Lisboa – and the main territory which have 0.01 hospitals per 100km2 – Alentejo, interior Centro and interior Norte.
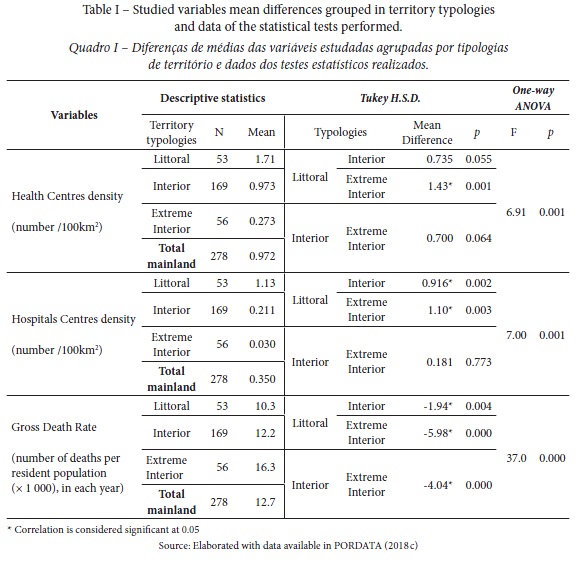
Health centres and hospitals distribution, and gross death rate differences are present between territory typologies (table I). From littoral to extreme interior mean reductions of 1.4 in health centres and of 1.1 in hospitals were found.
According to figure 4, between 2001 to 2011, gross death rate trend is very similar, maintaining the littoral-interior dichotomy. Extreme interior regions, by the Spain border, exhibit the highest gross death rate values.
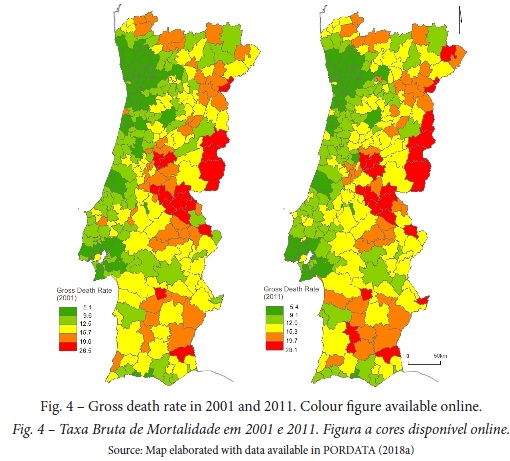
The mean gross death rate is higher (by 5.9 points) in extreme interior when compared to littoral. In order to identify variables correlations the Spearman correlation test was performed and results are presented on table II.
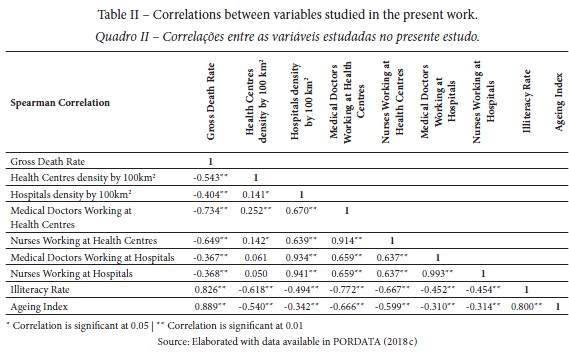
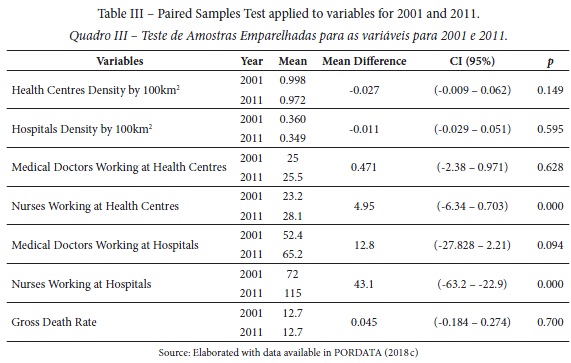
Gross death rate has a very strong association with illiteracy rate (rs = 0.826; p < 0.01) and with ageing index (rs= 0.889; p < 0.01). This suggests that in municipalities with more illiterate and aged populations, the vulnerability to death is higher. Alongside, there is a strong negative correlation between the number of health professionals at health centres and the gross death rate, namely medical doctors (rs = 0.734; p < 0.01) and nurses (rs = 0.649; p < 0.01). Results also show a negative correlation between the ageing index and health professionals at health centres: number of medical doctors (rs =0.666; p < 0.01) and nurses (rs =0.599; p < 0.01). A moderate correlation between health centres density by 100km2 and gross death rate (rs= 0.543; p < 0.01) was found at very significant level. Table III exhibits Paired Samples Test results in order to compare the years 2001 and 2011. Only two variables “nurses working at health centres” and “nurses working at hospitals” show statistically significant mean differences (p < 0,001).
VI. DISCUSSION
Health centres provide the primary answer in health promotion, such as disease prevention and treatment, services that should be available to all citizens. Access to an appropriate health care service should combine multiple dimensions: good health perceiving and service response; adaptation of health services to populations’ needs; proximity to health services; direct costs related to health services acquisitions; indirect costs related to transports to health centres or hospitals; quality of health service organization (Furtado & Pereira, 2010). Besides, distance to health services has an important role in amenable and preventable deaths. The number of inhabitants per health centre shows that in 2011, in the most populated mainland regions, there are more health centres to respond to populations needs (PORDATA, 2018b). This demographic portrait conveys the idea that the primary health services distribution is adjusted to the number of resident population. However, what this paper emphasizes is that in the less populated regions, namely in the central and northern interiors, Alentejo and in the most part of the Algarve region, ageing, depopulation and low population density contribute to an increase in death vulnerability in acute illness situations because the distance to reach the health centre is not taken into account. Results of health centres and hospitals spatial distribution reveal a clear situation of imbalance and inequity of populations living in interior and extreme interior regions that are also aged and low density populated areas. If equity to health care is merely accountable by the number of inhabitants served by a health infrastructure, than the existence of fewer health infrastructures in less populated regions would become rational. However, this criterion alone does not take into consideration the response time to acute situations or the availability of medical specialities that commonly exist only at principal hospitals.
Health centres, hospitals and gross death rate distribution are not symmetric. The difference related to health services distribution between territories typologies enhance the huge disparity in gross death rate distribution (F = 37.0; p = 0.000). Interior and extreme interior municipalities count on only one health centre. A recent study (Santana & Teixeira, 2017), reports that, in 2016, the number of available family doctors for a universe of 5210785 health users was only 2936 and the distribution continues to be very asymmetric in some interior municipalities without familiar health units. The Population Health Index (http://saudemunicipio.uc.pt/) developed at the Centro de Estudos em Geografia e Ordenamento do Território (CEGOT) da Universidade de Coimbra reveals that profound differences related to primary health care access, namely the distance between patients’ residence and health local units are still present in mainland Portugal.
Although lower population density is usual in these territories, their correspondent geographical area is large, consequently, the distance from population residences to health services is considerable. Alongside this evidence, is it visible that the ageing index is higher in these territories, which contribute to physical and social barriers to health care access. Results reveal differences between littoral and interior regions: in the latter, as regions are more isolated and apart from littoral, the lack of health professionals and infrastructures exhibits higher values of gross death and illiteracy rates. This fact is emphasized in the OECD Report (2016) which refers to the fact that Portugal has a higher medical doctor’s ratio per 1000 inhabitants (4.4) when compared to the mean European ratio (3.5). On the other hand, nurses ratio per 1 000 inhabitants (also 4.4) in Portugal is about half of the European mean (8.4) ranking the country in 10th position (OECD/EU, 2016). In agreement with these results, Furtado & Pereira (2010) conclude, that rural areas, particularly in interior regions, continue to be more distant from specialized hospitals than other regions. Diverse accessibility difficulties, namely isolation, poverty and absence of health education, are the main intrinsic barriers to the population’s access to health care services (Santana, 2010). The continuous process of ageing in Portugal contributes to the aggravation of inequalities in health care access due to the fact of high dependency and poor mobility among the elderly. These results also demonstrate that the lack of education contributes to higher death vulnerability (Pereira, 2002; Pereira & Pedro, 2004; Veiga, 2005). Improving access should also take into account “(…)the social factors influencing access” (Ministry of Health and Social Policy of Spain, 2010, p. 16).
The comparison of results between 2001 and 2011 reveals that, over a decade, there were only significant increases in nurses both working at health centres and at hospitals. For all the other variables – medical doctors working both at health centres and at hospitals and health centres and hospitals density by 100km2 –, means values were not statistically different. On the other hand, the gross death rate does not present a significant decrease, following the trend of the other variables.
Some studies consider that population concentration, namely in urban and littoral areas, is beneficial to faster access to health services (Santana, 2010). Nevertheless, concentration of health infrastructures at urban and littoral areas also represents an example of a unfair access to health services. Another relevant result for the prevention of death mortality is the important role of medical doctors (rs= 0.734; p < 0.01) and nurses (rs= 0.649; p < 0.01) working at health centres, when compared with the same professionals at hospitals, medical doctors (rs= 0.367; p < 0.01) and nurses (rs= 0.368; p < 0.01). Thus, the relationship between these services and the mortality rate may be justified by health promotion activities by health centres, contributing to health literacy and disease prevention through closer and more direct contact with younger to older populations, aligning the transmitted content to the specific needs of each age group.
VII. CONCLUSIONS
The importance of an efficient and attainable national health service is related with its capacity to eliminate health inequalities, contributing to a more fair and equitable society. Health protection and promotion are fundamental rights enabling human life, health, wellbeing and life quality. In order to develop an all-inclusive, universally attainable national health service, public investments should be provided: health education and promotion (healthy eating habits, physical and social mobility) in order to prevent disease and to enhance life quality of long-morbidity patients. Health inequalities act as social inequality generators, which require investment in health literacy at local communities, enlightenment on health concepts and symptoms. Notwithstanding the recognized importance of the National Health Service in Portugal, the result of this work provides evidence for the fact that mortality is associated with the distribution of health services – number of infrastructures and professional services – and population characteristics related to illiteracy and ageing. Therefore, supported on these results, the main conclusion of the present paper is related to the way that health public policies are designed. The results show that health services are distributed only according to population density. This reality does not take into account population needs and is linked to the fact that in most ageing areas there is a lack of health services, which contributes to a differential mortality. In the health public policies field, the main conclusion is that in a decade (2001 – 2011) the distribution of health infrastructures and professionals do not suffer a significant increase, revealing a disinvestment in the promotion of a fair distribution of health services and fighting against inequity in health services access.
These results provide knowledge about mainland health care services at the municipality level. Another expected contribution from the present work is the exposure of the urgent need of more in-deep research that would associate the population’s socioeconomic realities with health care access constraints, suggesting the need for a health public policies reformulation, in particular by emphasizing the specificities and needs of each region.
ACKNOWLEDGEMENTS
This work was part of a research project of FP-ENAS - UFP Energy, Environment and Health Research Unit funded by FCT – Fundação para a Ciência e a Tecnologia, I.P. through project UID/MULTI/4546/2016.
The authors would like to thank the peer review of anonymous reviewers for their valuable comments and suggestions that contributed to the improvement of paper.
REFERENCES
Alves, E., Correia, S., Barros, H., & Azevedo, A. (2012). Prevalence of self-reported cardiovascular risk factors in Portuguese women: a survey after delivery. International Journal of Public Health, 57(5), 837-847. [ Links ]
Assembleia da República. (2005). Artigo 64. º. Constituição da República Portuguesa. VII Revisão Constitucional [Article 64th. Portuguese Republic Constitution. VII Constitutional Revision].
Azevedo, L. F., Costa-Pereira, A., Mendonça, L., Dias, C. C., & Castro-Lopes, J. M. (2012). Epidemiology of chronic pain: a population-based nationwide study on its prevalence, characteristics and associated disability in Portugal. Journal of Pain, 13(8), 773-783. [ Links ]
Bastos, J., Peleteiro, B., Barros, R., Alves, L., Severo, M., De Fátima Pina, M… Lunet, N. (2013). Sociodemographic determinants of prevalence and incidence of Helicobacter pylori infection in Portuguese adults. Helicobacter, 18(6), 413-422.
Campos, A. C. (2011). O Percurso da Saúde: Portugal na Europa [The path of Health: Portugal in Europe]. Coimbra: Almedina. [ Links ]
Carapinheiro, G., & Pinto, M. P. (1986). Políticas de saúde num país em mudança: Portugal nos anos 70 e 80 [Health policies in a changing country: Portugal in 70's and 80's]. Sociologia, Problemas e Práticas, 1, 71-109. [ Links ]
Champman, J. L., Zechel, A., Carter, Y. H., & Abbott, S. (2004). Systematic review of recent innovation in service provision to improve access to primary care. British Journal of General Practice, 54(502), 374-381. [ Links ]
Charlton, J., Hartley, R., & Holland, W. (1983). Geographical variation in mortality from conditions amenable to medical intervention in England and Wales. The Lancet, 691-696. [ Links ]
Dalrymple, T. (2012). The inverse care law. BMJ, 344. doi: 10.1136/bmj.e1633 [ Links ]
Direção-Geral da Saúde. (2015). Plano Nacional de Saúde. Revisão e Extensão a 2020 [National Health Plan. Revision and Extension to 2020]. Lisboa: Direção-Geral da Saúde. [ Links ]
Direção-Geral da Saúde. (2012). Plano Nacional de Saúde 2012-2016 - 3.2. Eixo Estratégico - Equidade e Acesso aos Cuidados de Saúde [National Health Plan 2012-2016 - 3.2. Strategic Axes - Equity and Access to Health Care]. Lisboa: Direção-Geral da Saúde. [ Links ]
Entidade Reguladora da Saúde. (2009). Estudo do Acesso aos Cuidados de Saúde Primários do SNS [Access to NHS Primary Cares Study]. Porto: Entidade Reguladora da Saúde. [ Links ]
European Commission. (2015). Social situation monitor - income inequality in EU countries. Brussels: European Commission. [ Links ]
Eurostat. (2017). Amenable and Preventable deaths statistics. Retrieved from http://ec.europa.eu/eurostat/statistics-explained/index.php/Amenable_and_preventable_deaths_statistics [ Links ]
Freitas, Â., & Costa, C. (2015). Resultados em Saúde e Determinantes Contextuais [Health Results and Contextual Determinants]. In P. Santana (Ed.) A Geografia da Saúde da População. Evolução nos últimos 20 anos em Portugal Continental [Health population Geography. Last 20 years Mainland Portugal Evolution] (pp. 15-79). Coimbra: CEGOT - Universidade de Coimra.
Fundação Calouste Gulbenkian. (2014). Um Futuro para a Saúde - todos temos um papel a desempenhar [A Future for Health – We all have a role to play]. Lisboa: Fundação Calouste Gulbenkian. [ Links ]
Furler, J. S, Harris, E., Chondros, P., Davies, P. G. P., Harris, M. F., & Young, D. Y. (2002). The inverse care law revisited: impact of disadvantaged location on accessing longer GP consultation times. Medical Journal of Australia, 177, 80–83. Retrieved from https://www.mja.com.au/journal/2002/177/2/inverse-care-law-revisited-impact-disadvantaged-location-accessing-longer-gp [ Links ]
Furtado, C., & Pereira, J. (2010). Equidade e Acesso aos Cuidados de Saúde [Equity in Health Care Access]. Lisboa: Alto Comissariado da Saúde. Retrieved from http://www.acs.min-saude.pt/pns2011-2016/files/2010/08/EA1.pdf [ Links ]
Hart, J. T. (2000). Commentary: Three decades of the Inverse Care Law. British Medical Journal, 320(1), 15-19. [ Links ]
Hart, J. T. (1971). The Inverse Care Law. The Lancet, 297, 405-412. doi: 10.1016/S0140-6736(71)92410-X [ Links ]
Gay, J. G., Paris, V., Devaux, M., & De Looper, M. (2011). Mortality amenable to health care in 31 OECD countries: estimates and methodological issues. OECD Publishing: OECD Health Working Papers - No.55. [ Links ]
GBD 2015 Healthcare Access and Quality Collaborators. (2015). Healthcare Access and Quality Index based on mortality from causes amenable to personal health care in 195 countries and territories, 1990–2015: a novel analysis from the Global Burden of Disease Study 2015. The Lancet, 390, 231-266. [ Links ]
Gianino, M. M., Lenzi, J., Fantini, M. P., Ricciardi, W., & Damiani, G. (2017). Declining amenable mortality: a reflection of health care systems? BMC Health Services Research, 17(735), 1-8. [ Links ]
Gulliford, M., Figueroa-Munoz, J., Morgan, M., Hughes, D., Gibson, B., Beech, R., & Hudson, M. (2002). What does 'access to health care' mean? J. Health Serv. Res. Policy, 7, 186-188. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/12171751 [ Links ]
International Council of Nurses. (2011). Closing the gap: Increasing access and equity. Geneva: Internacional Council of Nurses. [ Links ]
Mackenbach, J. P., Hu, Y., Artnik, B., Bopp, M., Costa, G., Kalediene, R… Nusselder, W. J. (2017). Trends In Inequalities In Mortality Amenable To Health Care In 17 European Countries. Health Affairs, 36(6), 1110-1118.
Maia, R. L. (2001). Descontinuidades e Permanências nas Estruturas da Economia e da Sociedade Portuguesas nos Últimos Sessenta Anos [Discontinuities and Permanence’s in Portuguese Economy and Society structures in the Last Sixty Years]. Actas do IV Congresso Português de Sociologia (pp. 1-22). Coimbra: Associação Portuguesa de Sociologia.
Maia, R. L. (2014). Competition and Complementarity: Notes on the Internacional Projection of Europe's West Coast. In P. M. Santos & P. C. Seixas (Eds.), Globalization and Metropolization: Perspectives on Europe's West Coast (pp. 27-40). Berkeley: Institute of Governmental Studies. [ Links ]
McCoy, D. (2003). Health Sector Responses to HIV/AIDS and treatments access in southern Africa: Addressing equity. United Kingdom: Regional Network for Equity in Health in Southern Africa (EQUINET) in co-operation with Oxfam GB. [ Links ]
Ministry of Health and Social Policy of Spain. (2010). Moving forward in Health. Monitoring Social Determinants of Health and the re-education of Health Inequalities: An Independent Report Commissioned through the Spanish Presidency of the EU. Spain: Ministry of Health and Social Policy in Spain. [ Links ]
Nambiar, D., & Mander, H. (2017). Inverse care and the role of the state: the health of the urban poor. Bull. World Health Organization, 95(2), 152-153. doi: 10.2471/BLT.16.179325 [ Links ]
Nolte, E., & Mckee, C. M. (2008). Measuring the health of nations: updating an earlier analysis. Health Affairs, 27, 58-71. [ Links ]
Nolte, E., & Mckee, C. M. (2012). Amenable mortality - deaths avoidable through health care - progress in the US lags that of three European countries. Health Affairs, 31, 2114-2122. [ Links ]
Nolte, E., & Mckee, M. (2004). Does health care save lives? Avoidable mortality revisited. London: The Nuffield Trust. [ Links ]
Observatório Português dos Sistemas de Saúde. (OPSS). (2003). Evolução do Sistema de Saúde [Health System Evolution]. Retrieved from http://www.opss.pt/node/141 [ Links ]
European Observatory on Health Systems and Policies. (OECD). (2017). Portugal: Country Health Profile 2017. Brussels: European Observatory on Health Systems and Policies. [ Links ]
European Observatory on Health Systems and Policies. (OECD). (2016). Health at a Glance: Europe 2016 - State of Health in the EU Cycle. Paris: OECD Publishing [ Links ]
Pereira, J. (2002). Prestação de cuidados de acordo com as necessidades? Um estudo empírico aplicado ao sistema português [Care giving according to needs? an empirical study applied to Portuguese system]. In S. F. Piola & S. M. Vianna (Eds.), Economia da Saúde: conceitos e contribuição para a gestão de saúde [Health Economics: concepts and contribution to health management] (pp. 141-166). Brasília: IPEA. [ Links ]
Pereira, J., & Pedro, J. (2004). Education, income and health inequalities in Portugal. Applied Health Economics and Health Policy, 3(52). [ Links ]
PORDATA. (2018a). População Residente [Resident Population]. Retrieved from https://www.pordata.pt/Municipios/População+residente-359. [ Links ]
PORDATA. (2018b). SNS: habitantes por centros de saúde e extensão [NHS: inhabitants by health center and extension]. Retrieved from https://www.pordata.pt/Municipios/SNS+habitantes+por+centro+de+sa%c3%bade+e+extens%c3%a3o-499 [ Links ]
Remoaldo, P. C. (2003). Acessibilidade aos cuidados primários de saúde dos concelhos de Guimarães e de Cabeceiras de Basto [Accessibility to primary health care in the municipalities of Guimarães and Cabeceiras de Basto]. Revista Portuguesa de Clínica Geral, 19, 107-119. [ Links ]
Rutstein, D., Berenberg, W., Chalmers, T., Child, C., Fishman, A., & Perrin, E. (1976). Measuring the quality of medical care. New England Journal of Medicine, 294, 582-588. [ Links ]
Santana, P. (2017). Promoting Population Health and Equity. Coimbra: Coimbra University Press. [ Links ]
Santana, P. (2010). Os ganhos em saúde e no acesso aos serviços de saúde. Avaliação das últimas três décadas [Health gains and health services access. Evaluation of the last three decades]. In J. Simões (Ed.), Trinta anos do Serviço Nacional de Saúde. Um percurso comentado [Thirty years of the National Health Service. An annotated course] (pp. 1-41). Coimbra: Almedina. [ Links ]
Santana, P., & Freitas, A. (2015). Índice de saúde da população nos últimos 20 anos. A saúde da população [Population health index over the last 20 years. Health Popualtion]. In P. Santana (Coord.), A Geografia da Saúde da População. Evolução nos últimos 20 anos em Portugal Continental [The Health Geography of Population. Evolution in the last 20 years in mainland Portuga] (pp. 80-105). Porto, Coimbra: CEGOT. [ Links ]
Santana, P., & Ferreira, P. L. (2017). Equidade em saúde. O papel das condições socioeconómicas e dos cuidados de saúde primários [Equity in health. The role of socio-economic conditions and primary health care]. In F. Cravidão, L. Cunha, P. Santa & N. Santos (Orgs.), Espaços e Tempos em Geografia. Homenagem a António Gama [Spaces and Times in Geography. Tribute to António Gama] (pp. 403-424). Imprensa da Universidade de Coimbra.
Silva, M. V. (2012). Políticas públicas de saúde: tendências recentes [Health public policies: recent trends]. Sociologia, Problemas e Práticas, 69, 121-128. [ Links ]
Simões, J., Teixeira, M., Barros, P., Pereira, J., Moreira, P., Ferreira, A… Silva, S. (2007). Comissão para a sustentabilidade do financiamento do Serviço Nacional de Saúde - Relatório Final [Commission for the sustainability of the financing of the National Health Service - Final Report].
Veiga, P. (2005). Income-related health inequality in Portugal. Working Paper - Universidade do Minho, 28. [ Links ]
Watkins, J., Wullaningsih, W., Zhou, C. D., Marshall, D. C., Sylianteng, G. D., Rosa, P. G… Maruthappu, M. (2017). Effects of health and social care spending constraints on mortality in England: a time trend analysis. BMJ Open, 7, 1-9.
Watt, G. (2002). The inverse care law today. The Lancet, 360, 252-254. doi: 10.1016/S0140-6736(02)09466-7 [ Links ]
Whitehead, M. (1992). The concepts and principles of equity in health. International Journal of Health Services, 22(3), 429-445. [ Links ]
World Health Organization. (WHO). (2018). What do we mean by availability, accessibility, acceptability and quality (AAAQ) of the health workforce? Global Health Workforce Alliance, World Health Organization. Retrieved from http://www.who.int/workforcealliance/media/qa/04/en/ [ Links ]
World Health Organization. (WHO). (2010). Portugal Health System Performance Assessment. Denmark: WHO Regional Office for Europe. [ Links ]
World Health Organization. (WHO). (2008). Commission on Social Determinants of Health. Closing the gap in a generation: health equity through action on the social determinants of health. Final report of the Commission on Social Determinants of Health. Retrieved from http://apps.who.int/iris/bitstream/handle/10665/43943/9789241563703_eng.pdf;jsessionid=BF9D1569579DA0D27E4890B9CEDF7BB4?sequence=1 [ Links ]
World Health Organization. (WHO). (2000). The World Health Report 2000. Health systems: improving performance. Geneva: World Health Organization.
Recebido: março 2018. Aceite: setembro 2018.














